Information Sources And Study Selection
Studies were identified by searching Ovid MEDLINE for the period 1946 to November 2013 , the Cochrane library , Google Scholar , NHS Evidence . An example search strategy was shown in Figure 1, which indicates the keywords used.
Fig. 1
Search strategy.
In addition, reference lists of relevant articles were searched to identify other relevant studies . For articles that did not have a complete electronic version of the full text available, the article was requested from the British Library Document Supply Service 2 articles were obtained through this means.
Ta T1 Low And Intermediate Transitional Cell Carcinoma Of The Bladder: Recurrence Rates And The Timing Of Check Cystoscopies Within The First Year
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Unlimited fulltext viewing Of this article
- Organize, annotate And mark up articles
- Printing And downloading restrictions apply
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Ascertainment Of Survival Outcomes
We used the Registered Persons Database to verify OS . This database contains both the date of last contact with the healthcare system and the date of death for all individuals who ever received coverage by OHIP. The Office of the Registrar General-Deaths database was queried to calculate CSS . Professional data abstractors maintain this database by translating each death certificate into a leading cause of death according to the methodology developed by Becker etal. . Patients were censored at their date of last contact with the healthcare system or if they died due to a leading cause of death other than BC . The date of diagnosis was defined as time zero. Maximal follow-up was 30 September 2019 and 31 December 2016 for OS and CSS, respectively.
Also Check: How Quickly Can A Bladder Infection Start
Permission To Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as NCIs PDQ cancer information summary about breast cancer prevention states the risks in the following way: .
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Bladder Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated < MM/DD/YYYY> . Available at: . Accessed < MM/DD/YYYY> .
Images in this summary are used with permission of the author, artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Treatment For Hg T1 Bladder Cancer With Pt0 Histology At Second Tur
TURBT followed by intravesical BCG therapy provides lower incidences of recurrence and progression than those obtained by TURBT alone . Sylvester et al. performed a meta-analysis on the efficacy of intravesical BCG therapy. They evaluated 24 trials involving a total of 4863 patients and concluded that intravesical BCG significantly reduces the risk of progression after TURBT in NMIBC patients who receive maintenance treatment. Since T1 bladder cancer is considered to be high-risk cancer regardless of the pathological findings for the second TUR specimen , various guidelines recommend full-dose intravesical BCG for 13 years except in the case of immediate cystectomy. Alternatively, mitomycin C is also recommended by the National Comprehensive Cancer Network guidelines . This is based on a meta-analysis that showed no statistically significant difference between BCG and MMC for progression and survival .
Protocol and study design of the JCOG1019 trial .
Don’t Miss: Does Drinking Water Help With Overactive Bladder
Other Options During Follow
Since 2019, the EAU guideline has a recommendation on outpatient fulguration or laser vaporization of small papillary recurrences in follow-up of patients known with previous low-grade Ta tumors . Although the recommendation is weak, this is often common practice in daily routine. Outpatient fulguration obviously does not prevent a cystoscopy, but it does reduce subsequent therapeutic burden.
Understanding The Statistics: Cancer Survival
It is important to remember that all cancer survival numbers are based on averages across huge numbers of people. These numbers cannot predict what will happen in your individual case.
Survival rates will not tell you how long you will live after you have been diagnosed with bladder cancer. But, these numbers can give you an idea of how likely your treatment will be successful. Also, survival rates take into account your age at diagnosis but not whether you have other health conditions too.
Also Check: What Can Cause Uncontrollable Bladder
Treatment Of Stages Ii And Iii Bladder Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
- Transurethral resection with fulguration.
- A clinical trial of a new treatment.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Role Of Cystectomy In Nmibc
Guideline Statement 27
27. In a patient with Ta low- or intermediate-risk disease, a clinician should not perform radical cystectomy until bladder-sparing modalities have failed.
Discussion
Low-grade, noninvasive tumors very rarely metastasize, and even large-volume, multifocal cancers can usually be managed with techniques, such as staged resection. Patients with low-grade recurrences can be successfully managed with intravesical chemotherapy 225 or BCG. 177,226,227 In addition, small, multifocal recurrences despite intravesical therapy can usually be treated effectively with office fulguration, repeat TURBT or even surveillance, in select cases. 64-67
Guideline Statement 28
28. In a high-risk patient who is fit for surgery with persistent high-grade T1 disease on repeat resection, or T1 tumors with associated CIS, LVI, or variant histologies, a clinician should consider offering initial radical cystectomy.
Discussion
Guideline Statement 29
29. In a high-risk patient with persistent or recurrent disease within one year following treatment with two induction cycles of BCG or BCG maintenance, a clinician should offer radical cystectomy.
Recommended Reading: How To Stop Bladder Leakage While Exercising
What Are The Risk Factors For Bladder Cancer
Some factors increase the risk of bladder cancer:
- Cigarette smoking is the biggest risk factor it more than doubles the risk. Pipe and cigar smoking and exposure to second-hand smoking may also increase one’s risk.
- Prior radiation exposure is the next most common risk factor .
- Certain chemotherapy drugs also increase the risk of bladder cancer.
- Environmental exposures increase the risk of bladder cancer. People who work with chemicals, such as aromatic amines are at risk. Extensive exposure to rubber, leather, some textiles, paint, and hairdressing supplies, typically related to occupational exposure, also appears to increase the risk.
- Infection with a parasite known as Schistosoma haematobium, which is more common in developing countries and the Middle East.
- People who have frequent infections of the bladder, bladder stones, or other diseases of the urinary tract, or who have chronic need for a catheter in the bladder, may be at higher risk of squamous cell carcinoma.
- Patients with a previous bladder cancer are at increased risk to form new or recurrent bladder tumors.
Other risk factors include diets high in fried meats and animal fats, and older age. In addition, men have a three-fold higher risk than women.
Categories Of Bladder Cancer
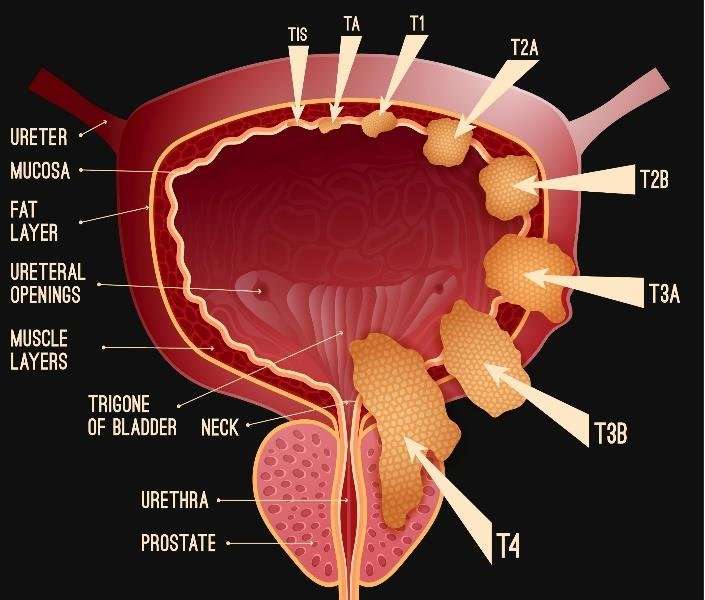
Bladder cancers fall into five broad categories based on their grade andstage – a full explanation of these terms can be found below:
- Low risk non-muscle invasive bladder cancerThese are small , single low grade Grade 1 or Grade 2) bladdercancers that haven’t grown beyond the inner layer of the bladder. They are usuallydescribed as papillary and are called pTa – where the p indicatesthat this has been found out by biopsy.
- Intermediate risk non-muscle invasive bladder cancerThese are larger or multiple low grade pTa bladder cancers.Small, single low grade pT1 tumours are also in this category where T1indicates that the cancer has grown a little further into the bladder wall. Also if low risk tumours keep growing backthey fall into this category.
- High risk non-muscle invasive bladder cancerThese are Grade 3 pTa or pT1 bladder cancers. All larger ormultiple T1 tumours are also included. Carcinomain Situ is also in this category.
- Muscle invasive bladder cancerThese are bladder cancers which are pT2 or pT3 which indicates that the cancerhas grown further into the bladder wall and is found in the inner muscle layer.
- Advanced bladder cancerThese are bladder cancers which are pT4 which indicates that it has grownthrough the bladder wall or have spread to nearby lymph nodes to varying degrees- referred to as N1, N2 or N3) or to other sites in the body referred to as M1.
Also Check: How Long Can A Puppy Hold His Bladder
Enhanced Cystoscopy And Imaging For Follow
As mentioned above, white light cystoscopy has limitations with sensitivity for papillary tumors of 7080%, which is lower in case of CIS . These numbers are in trials, and for the studies performed with blue light in the setting of a transurethral resection, so in the operating room. Can we also use these techniques to improve our performance during outpatient follow-up, which usually is done with flexible instruments.
NBI is easy to perform in an outpatient setting, since it does not require additional preparation and the specific equipment can be used both in the clinical as well as in the outpatient setting. The real advantage of NBI, however, remains to be proven, since published data are limited and not in agreement. Mukherjee et al. showed in a randomized controlled trial NBI to be better in tumor detection and resection as compared to white light , whereas an earlier and larger study did not show a difference in recurrence rate after 1 year of follow-up .
The consequence of better tools in follow-up, in this case better cystoscopy, has been shown to result in more confidence and less anxiety among patients and urologists, resulting in longer intervals between cystoscopies . Another way to improve the sensitivity of cystoscopy might be the use of artificial intelligence , which was shown to improve both sensitivity and specificity resulting in a better bladder cancer detection and resection .
Treatment For Hg Pt1 Bladder Cancer With Pt2 Or More Histology At Second Tur

There is no doubt about the need to perform radical cystectomy for patients with muscle-invasive disease at the second TUR. Most of these tumors are understaged at the initial TURBT due to technical problems, and may not be large or bulky like muscle-invasive tumors that are diagnosed at the initial TURBT and/or with computed tomography or magnetic resonance imaging. The discussion on the treatment strategies for these tumors does not include whether cystectomy should be performed but whether neoadjuvant chemotherapy and/or extended lymph node dissection should be performed.
Several randomized Phase III trials and meta-analyses demonstrated the survival benefit of cisplatin-based neoadjuvant chemotherapy for patients with MIBC. However, whether neoadjuvant chemotherapy prolongs the survival of patients with T1 cancer at the initial TURBT and with muscle-invasive disease detected by a second TUR is unclear. Neoadjuvant chemotherapy offers potential advantages in tumor downstaging and eradication of micrometastases, so this therapy should be indicated for patients who have risk factors for locally advanced disease or nodal metastasis.
Read Also: How Do I Get Rid Of A Bladder Infection
Bladder Cancer Is A Disease In Which Malignant Cells Form In The Tissues Of The Bladder
The bladder is a hollow organ in the lower part of the abdomen. It is shaped like a small balloon and has a muscular wall that allows it to get larger or smaller to store urine made by the kidneys. There are two kidneys, one on each side of the backbone, above the waist. Tiny tubules in the kidneys filter and clean the blood. They take out waste products and make urine. The urine passes from each kidney through a long tube called a ureter into the bladder. The bladder holds the urine until it passes through the urethra and leaves the body.
There are three types of bladder cancer that begin in cells in the lining of the bladder. These cancers are named for the type of cells that become malignant :
- Transitional cell carcinoma: Cancer that begins in cells in the innermost tissue layer of the bladder. These cells are able to stretch when the bladder is full and shrink when it is emptied. Most bladder cancers begin in the transitional cells. Transitional cell carcinoma can be low-grade or high-grade:
- Low-grade transitional cell carcinoma often recurs after treatment, but rarely spreads into the muscle layer of the bladder or to other parts of the body.
- High-grade transitional cell carcinoma often recurs after treatment and often spreads into the muscle layer of the bladder, to other parts of the body, and to lymph nodes. Almost all deaths from bladder cancer are due to high-grade disease.
See the following PDQ summaries for more information:
Scoringmodels Using The Who 1973 Classification System
6.1.1.1.The 2006 European Organisation forResearch and Treatment of Cancer scoring model
To be able to predict both the short- and long-term risks of diseaserecurrence and progression in individual patients, the EORTC Genito-Urinary Cancer Grouppublished a scoring system and risk tables based on the WHO 1973 classification in 2006 . The scoring system is based on the six most significantclinical and pathological factors in patients mainly treated by intravesical chemotherapy:
- Number of tumours
- Concurrent CIS
- WHO 1973 tumour grade.
Using the 2006 EORTC scoring model, individual probabilities of recurrenceand progression at one and five years may be calculated.
6.1.1.2.The model for patients with TaG1/G2 tumours treated with chemotherapy
Patients with TaG1/G2 tumours receiving chemotherapy were stratified intothree risk groups for recurrence, taking into account the history of recurrences, history ofintravesical treatment, tumour grade , number of tumours and adjuvant chemotherapy.
6.1.1.3.Club Urologico Español deTratamiento Oncologico scoring model for BCG-treated patients
- gender
6.1.1.4.The 2016 EORTC scoring model forpatients treated with maintenance BCG
Don’t Miss: How To Regain Bladder Control After Prostate Surgery
Predictive Factors For Residual Hg Disease At Retur
On univariable analysis, predictive factors for residual HG disease at reTUR were size> 3 cm , multifocality , concomitant CIS , NLR> 3 and BMI . On multivariable analysis, size > 3 cm , concomitant CIS , overweight and obesity status according to BMI remained as significant independent predictors for HG residual disease at reTUR .
Table 1
Association of HG/G3 on reTUR with clinical and pathologic characteristics of 1155 patients after primary T1 HG/G3 NMIBC
| All patients |
|---|
TURBT: transurethral resection of bladder tumor, OR: Odds ratio, CI: Confidence interval
Smoking Can Affect The Risk Of Bladder Cancer
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer not having risk factors doesn’t mean that you will not get cancer. Talk to your doctor if you think you may be at risk for bladder cancer.
Risk factors for bladder cancer include the following:
- Using tobacco, especially smoking cigarettes.
- Having a family history of bladder cancer.
- Having certain changes in the genes that are linked to bladder cancer.
- Being exposed to paints, dyes, metals, or petroleum products in the workplace.
- Past treatment with radiation therapy to the pelvis or with certain anticancer drugs, such as cyclophosphamide or ifosfamide.
- Taking Aristolochia fangchi, a Chinese herb.
- Drinking water from a well that has high levels of arsenic.
- Drinking water that has been treated with chlorine.
- Having a history of bladder infections, including bladder infections caused by Schistosoma haematobium.
- Using urinarycatheters for a long time.
Older age is a risk factor for most cancers. The chance of getting cancer increases as you get older.
Read Also: How To Know If Cat Has Bladder Infection
Future Directions In The Treatment Of T1 Disease
The development of novel intravesical therapies represents an important area of active research for T1 disease. Intravesical gemcitabine, for example, has now been evaluated in several randomized trials. A meta-analysis of 6 trials noted that gemcitabine was superior to intravesical BCG for reducing recurrence in the setting of prior BCG-failure, but was notassociated with lower recurrence or progression rates in BCG-naïve patients . Intravesical docetaxel also appears to have activity in BCG-failures . Viral vector-based therapies hold promise, with a phase 1 study of intravesical adenovirus-mediated interferon-2b demonstrating activity in the setting of BCG failures .
Future paradigms are likely to include both novel intravesical agents and drug delivery mechanisms to improve the bladder-preserving treatment options for T1 patients.
After Bladder Cancer Has Been Diagnosed Tests Are Done To Find Out If Cancer Cells Have Spread Within The Bladder Or To Other Parts Of The Body
The process used to find out if cancer has spread within thebladder lining and muscle or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment. The following tests and procedures may be used in the staging process:
Also Check: Is Heat Good For Bladder Infection