Evaluation Of Patients With The Oab Syndrome
There are usually no clinical signs on examination, so a careful history is essential. Table presents the questions a clinician should ask a patient presumed to have OAB. The primary care physician should take a focused history and perform a primary evaluation for urinary tract disorders, such as recurrent urinary tract infections, urinary bladder calculi, and bladder tumors. Such an evaluation is necessary to rule out general conditions and risk factors that cause incontinence such as diabetes mellitus, stroke, lumbar disc disease or spinal cord injury, Parkinson’s disease, multiple sclerosis, pelvic surgery, multiple vaginal deliveries and obstetric history, immobility, dementia, and psychiatric disease.
Are Claims For Newer Drugs For Overactive Bladder Warranted
Two previous Therapeutics Letters on drugs for overactive bladder concluded that the antimuscarinic drugs had limited short-term potential symptomatic benefit and significant risk of adverse effects .1, 2 This Letter compares drugs to one another, including newer drugs introduced since 2007, when our most recent Letter on this topic was published.2
Adverse Event Assessment Of Antimuscarinics For Treating Overactive Bladder: A Network Meta
-
Affiliations Horten Centre for Patient Oriented Research, University of Zürich, Zürich, Switzerland, Neuro-Urology, Spinal Cord Injury Centre, Balgrist University Hospital, Zürich, Switzerland
-
Affiliation Horten Centre for Patient Oriented Research, University of Zürich, Zürich, Switzerland
-
Affiliation Horten Centre for Patient Oriented Research, University of Zürich, Zürich, Switzerland
-
Affiliation Horten Centre for Patient Oriented Research, University of Zürich, Zürich, Switzerland
-
Affiliation Horten Centre for Patient Oriented Research, University of Zürich, Zürich, Switzerland
-
Affiliation Department of Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, Ontario, Canada
-
Affiliations Horten Centre for Patient Oriented Research, University of Zürich, Zürich, Switzerland, Department of Clinical Epidemiology and Medical Technology Assessment, Maastricht University Medical Centre, Maastricht, The Netherlands
Read Also: Does Uti Cause Bladder Leakage
Side Effects Of Antimuscarinic Drugs And Safety Precautions
Dry mouth and constipation are the most common and bothersome side effects of antimuscarinic agents. In addition constipation may potentiate symptoms due to the effect of the presence of excessive stool in the rectal ampulla. This may decrease the bladder capacity and therefore, should constipation appear, an early use of fiber and stool softeners is recommended .
Constipation may lead to the discontinuation of medication in up to 50% of patients . Another reason for not following the recommended oral drug regime during the first 2 to 3 months may be that improvement appears gradually or only to a small degree.
Contraindications for the use of antimuscarinic agents are patients with closed angle glaucoma, myasthenia gravis, severe ulcerative colitis, a toxic megacolon, or intestinal obstruction because of their anticholinergic effects on the bowel. However, treatment decisions should be individualized and their prescription might need approval from the clinician caring for these disorders.
Compliance in using antimuscarinic may not be sufficient, as shown in a 2011 systematic review of 149 papers that found discontinuation rates of 4383% in the first 30 days of treatment, and more than half of patients never refilled the initial prescription . Regular follow-ups are important in monitoring treatment effects and adherence. All available antimuscarinic drugs come as an oral preparation.
Risk Of Overactive Bladder Associated With Medications For Dementia
A study from the University of Houston College of Pharmacy, and published in the Journal of the American Geriatrics Society, has evaluated the risk of overactive bladder as a side effect of cholinesterase inhibitor drugs taken for dementia and Alzheimer’s disease. The research was based on the dissertation work of the study’s first author Prajakta Masurkar.
Dementia is a group of symptoms associated with a decline in memory, reasoning or other thinking skills. Alzheimer’s disease is the most common cause of dementia, accounting for 60%80% of cases. ChEI drugs, including donepezil, galantamine and rivastigmine, increase communication between nerve cells to enhance cognition.
“The study found that the risk of overactive bladder varies across individual ChEIs,” reports Rajender R. Aparasu, Mustafa and Sanober Lokhandwala Endowed Professor of Pharmacy and chair, Department of Pharmaceutical Health Outcomes and Policy. “Using a national cohort of older adults with dementia, we also found that donepezil was associated with a 13% increased risk of OAB compared to rivastigmine, whereas there was no differential risk of OAB with galantamine and rivastigmine.”
Using Medicare data, the study examined 524,975 adults with dementia who were users of ChEIs . The primary outcome of interest was OAB diagnosis or prescription of antimuscarinics, drugs which help correct overactive bladder, within six months of ChEI initiation.
This study opens a new door.
Don’t Miss: What Does Bladder Cancer Look Like On Ultrasound
Pathophysiology Of The Oab Syndrome
Various factors may be involved in OAB and the major cause may vary from individual to individual. The etiology of OAB is still under investigation and is not well understood. However, 4 theories have been proposed to explain the pathophysiology of OAB:
The neurogenic theory: reduction in the inhibitory neural impulses and increase in the afferent impulses from the bladder trigger the voiding reflex .
The myogenic theory: the detrusor muscle becomes more sensitive to cholinergic stimulation leading to increased spontaneous activity .
The autonomous bladder theory: alteration or exacerbation of phasic activity is generated by muscarinic stimulation .
The afferent signaling theory: spontaneous bladder contractions during filling result in increased afferent output and hence the awareness of bladder filling .
Muscarinic Receptor Antagonists For Overactive Bladder
Paul Abrams
Bristol Urological Institute, Southmead Hospital, Bristol, UK and Wake Forest Institute for Regenerative Medicine, Winston-Salem, NC, USA
Karl-Erik Andersson
Bristol Urological Institute, Southmead Hospital, Bristol, UK and Wake Forest Institute for Regenerative Medicine, Winston-Salem, NC, USA
Paul Abrams
Bristol Urological Institute, Southmead Hospital, Bristol, UK and Wake Forest Institute for Regenerative Medicine, Winston-Salem, NC, USA
Karl-Erik Andersson
Bristol Urological Institute, Southmead Hospital, Bristol, UK and Wake Forest Institute for Regenerative Medicine, Winston-Salem, NC, USA
Also Check: Where Is My Bladder Located Female
Posterior Tibial Nerve Stimulation
Electrostimulation is included within the conservative therapies used to treat OAB by acting on the afferent nerves of the pelvic floor. When conducting a systematic review, two clinical trials compared the action of the electrostimulation with oxybutynin in patients with UUI, showing a similar efficacy between the two treatments .
Posterior tibial nerve stimulation is performed using a neuromodulator that utilizes the peroneal nerve for afferent access to the S3 spinal cord region. The mechanism that makes the neuromodulation of the bladderurethra reflexes possible is based on the fact that the nerve fibres of the posterior tibial region share sensitive inputs with the S3 root. Current indications include overactive bladder with or without UUI and chronic pelvic pain.
The stimulation can be done in a percutaneous manner with a thin 34 G needle inserted just below the medial malleolus of the ankle , although it can also be done in a transcutaneous manner . Adequate stimulation applied using the neuromodulator, regarding the frequency, intensity and length of the impulses, is demonstrated when the big toe is observed flexing or the remaining toes show extension or flexion. The normal treatment scheme consists of 12 weekly sessions of 30 min.
The side effects associated with this technique are infrequent and mild. The most common include cases of a painful feeling and transitory bleeding or bruising at the puncture site .
Search Strategy And Selection Criteria
This systematic review was done according to the PRISMA statement . A review protocol was elaborated, which is available on file with the authors. To identify randomized controlled trials of antimuscarinics versus placebo , we started with the recent Cochrane review by Nabi et al. and a literature search update from June 2005 to November 2007 kindly provided by the Cochrane Incontinence Review Group according to their previously published search strategy . Head-to-head comparative trials without a placebo arm were identified from the two recent meta-analysis by Chapple et al. and by Novara et al. . In addition, we searched reference lists and conference abstracts by hand, checked relevant reviews, book chapters, and contacted manufacturers and trialists. The search strategies are available on request.
Two investigators independently assessed reports for eligibility. To be included, studies had to be randomized controlled trials comparing at least one antimuscarinic for treating OAB with placebo or with another antimuscarinic. All currently used antimuscarinics were included, i.e. darifenacin, fesoterodine, oxybutynin, propiverine, solifenacin, tolterodine, and trospium chloride. Trials with intravesical antimuscarinic administration, drugs with less direct antimuscarinic effects , and drugs no longer used in clinical practice were excluded. In the case of multiple publications on the same patients, the most complete report was chosen for each trial.
Read Also: How To Test For A Bladder Infection At Home
Antimuscarinic Drug Class Review
We conducted a systematic review of direct comparator randomized controlled trials of antimuscarinic drugs in OAB, using Cochrane review methods. For infrequent harms, including cognitive effects in the elderly, we also reviewed RCTs in people without OAB, placebo-controlled RCTs, and non-randomized studies. Outcomes were considered in a hierarchy based on importance to the patient: mortality, serious adverse events including cognitive impairment and urinary retention, quality of life, patient-reported improvement, withdrawals due to adverse effects, urgency incontinence, nocturia, and anticholinergic effects such as dry mouth, constipation or blurred vision.
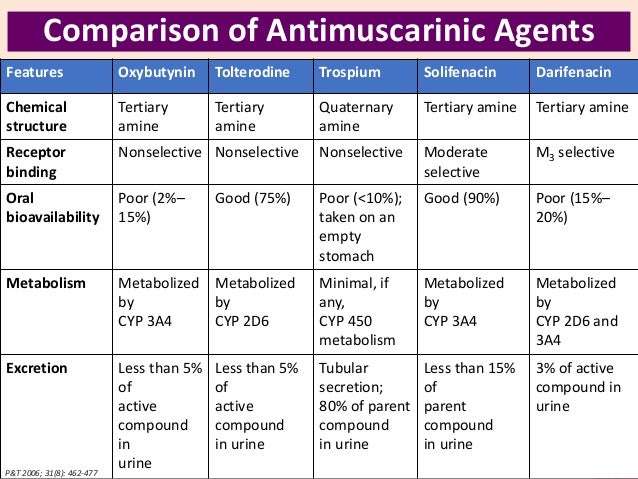
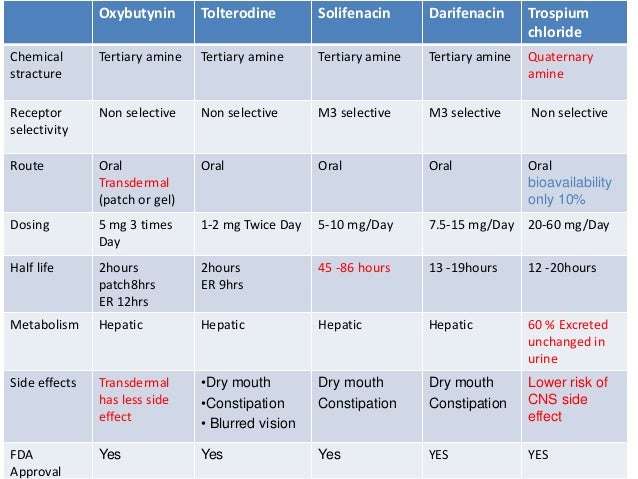
Results: We identified two recent systematic reviews6, 10 and 35 direct, active comparator RCTs in patients with OAB, mostly of 12 weeks duration. Most compared oxybutynin IR with other formulations of oxybutynin, tolterodine , darifenacin, solifenacin or trospium IR.Efficacy differences were small and of doubtful clinical relevance. For example, condition-specific quality of life did not differ or differences were below the threshold for clinical relevance, and incontinence episodes did not differ, or differed by 0.2-0.6 episodes/day. Differences between drugs in pharmacokinetics, metabolism, drug-drug interactions, bladder selectivity, and propensity to cross the blood brain barrier were not reflected in clinically meaningful differences.
Prescription Drugs For Overactive Bladder
There are several prescription drugs for overactive bladder .
The FDA approved medications, or drugs, currently available on the U.S. market for the treatment of urinary incontinence are for a specific condition called overactive bladder . Some are also used for OAB with urge urinary incontinence . You may have seen advertisements on television or in magazines for these medications. Most of the prescription drugs for OAB partially calm the bladder muscles that cause abnormal contractions, thereby reducing the frequency and severity of the overwhelming urge to urinate. Some of these drugs may also increase the bladders capacity to hold urine and delay the initial urge to void. This class of drugs is referred to as antimuscarinics.
The currently FDA approved antimuscarinic drugs for OAB are: Oxybutynin, Tolterodine, Solifenacin, Hyoscyamine, and Darifenacin. These drugs are sold under the names of: Ditropan, Detrol, Vesicare, Enablex, Levbid, Cytospaz and Oxytrol. Most of these are oral medications and need a doctors prescription. Only one drug will be available over-the-counter as of September 2013, and it is in a skin patch form for women only.
Note: Drugs that are currently approved may be suddenly taken off the market, and new drugs are being introduced. Your healthcare provider and pharmacist can help you know which current drugs on the market may be the best for your circumstances.
Who May Need a Prescription?
Possible Side Effects
Key Points to Remember
Also Check: Things To Avoid When You Have A Bladder Infection
Exposures And Outcome Definitions
Antimuscarinic medication exposure was identified via National Drug Codes and generic names using PDE files. The selective antimuscarinic cohort included new users of solifenacin or darifenacin. The non-selective antimuscarinic cohort included new users of oxybutynin, fesoterodine, tolterodine, or trospium. The primary outcome of this study was the time to all-cause mortality during the follow-up duration of maximum 6 months after initiation of either non-selective or selective drug class . The MBSF part A/B/C/D summary file was used to identify mortality events for all beneficiaries. Patients were followed until they died or were censored if they switched to the other antimuscarinic medication class from the index antimuscarinic medication class, or discontinued their antimuscarinic medication , or had a gap of 7 days between two consecutive refills, or reached the end of their follow-up period or end of study period , whichever happened earlier.
Antimuscarinic Drugs To Treat Overactive Bladder
- Accepted 20 January 2012
A 45 year old woman presents to her general practitioner complaining of troublesome urinary symptoms increasingly affecting her quality of life. She is currently voiding more than 10 times a day and rising three times at night. In addition she notices a sudden urgent desire to void and on two occasions has leaked urine before reaching the toilet. She gives no history of urinary tract infection or haematuria. Her periods remain regular.
In the past she has had two vaginal deliveries, has no significant medical history, and is not taking any medication. Pelvic examination is unremarkable and urine analysis normal. Ultrasound examination shows no post-void residual urine.
Based on the history, clinical examination, and basic investigations you make a symptomatic diagnosis of overactive bladder. After discussing her bladder symptoms, you offer lifestyle advice including the moderation of fluids and reduction of caffeine intake. In addition you refer her for bladder retraining and start treatment with antimuscarinic drugs.
Also Check: Surgical Treatment For Overactive Bladder
Antimuscarinic Drugs And Cognition
Most direct comparator RCTs did not actively assess cognition and were under-powered for infrequent serious cognitive adverse events one poor-quality RCT showed no difference in cognition between oxybutynin IR and oxybutynin ER.27
An additional 15 RCTs assessed cognitive effects, mainly in healthy volunteers and/or vs. placebo. Assessed outcomes included recall on computerized cognitive tests and Mini Mental Status Evaluation. None of the RCTs allowed a conclusion of different cognitive effects with any specific antimuscarinic vs. another. No RCT assessed cognition with chronic use of antimuscarinic drugs.A recently published, population-based cohort study in people age 65 assessed risk of new onset dementia following long-term cumulative exposure to anticholinergic drugs .28 Exposure equivalent to oxybutynin 5 mg daily for > 3 years was associated with an increased risk of dementia compared with no exposure: adjusted hazard ratio 1.54 . These findings are consistent with two shorter-term cohort studies 29, 30 and a recent systematic review.31
How Anticholinergic Bladder Medications Work
Anticholinergic drugs are often prescribed to treat OAB. These drugs work by relaxing your bladder muscles. They also help prevent urine leaks by controlling bladder spasms.
Most of these drugs come as oral tablets or capsules. They also come in transdermal patches and topical gels. Most are only available as prescriptions, but the patch is available over the counter.
Oxybutynin is an anticholinergic drug for overactive bladder. Its available in the following forms:
- oral tablet
- transdermal patch
- topical gel
You take this drug on a daily basis. Its available in several strengths. The oral tablet comes in immediate-release or extended-release forms. Immediate-release drugs release into your body right away, and extended-release drugs release into your body slowly. You may need the take the immediate-release form up to three times per day.
Don’t Miss: Best Pills For Bladder Infection
Newer Agents For The Management Of Overactive Bladder
BENJAMIN J. EPSTEIN, PHARM.D., B.C.P.S., JOHN G. GUMS, PHARM.D., and EMERSON MOLINA, PHARM.D., University of Florida, Gainesville, Florida Fort Lauderdale, Florida
Am Fam Physician. 2006 Dec 15 74:2061-2068.
Overactive bladder is a clinical syndrome characterized by one or more symptoms of urgency , frequency , nocturia, and incontinence. In persons without overactive bladder, the need to empty the bladder becomes progressively more demanding in overactive bladder, urgency is characterized by unheralded messages of an immediate need to empty the bladder. These signals are difficult to delay. The inability to delay urination results in episodes of incontinence in up to 40 percent of patients with overactive bladder.
A = consistent, good-quality patient-oriented evidence B = inconsistent or limited-quality patient-oriented evidence C = consensus, disease-oriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, see page 2008 or.
Percutaneous Tibial Nerve Simulation
A less invasive option called percutaneous tibial nerve stimulation is also available. It only takes about half an hour per session to perform and is usually done in a doctors office.
In PNTS, a needle electrode is inserted near the ankle that delivers electrical pulses to the tibial nerve. This nerve is linked directly to the sacral nerve.
As in SNS, these electrical pulses help block inappropriate bladder signaling.
Read Also: Botox Injection For Bladder Incontinence
Rationale For Anticholinergic Use
Detrusor muscle contractions are essential for normal micturition, but involuntary contractions produce the symptoms of overactive bladder. Contractions depend on the activation of muscarinic receptors in the bladder by acetylcholine. The M3 muscarinic receptor-subtype is thought to be the most important in regulating detrusor contractions.
Anticholinergic drugs block muscarinic receptor activation and inhibit the spontaneous detrusor contractions found in overactive bladder. Drug efficacy is dose-dependent, but effectiveness is often limited by unwanted antimuscarinic effects in distant organs where other acetylcholine receptor-subtypes predominate . These adverse effects are also dose-dependent. They commonly include dry mouth, dry eyes, confusion, constipation, somnolence, blurred vision and increased heart rate.
There are no currently available drugs with pure selectivity for the muscarinic receptors in the detrusor. To try to improve the benefit:harm ratio a number of anticholinergics have been developed with greater selectivity for the detrusor or the M3 receptor, or with extended release properties.
What Is Overactive Bladder
Overactive bladder is the term used to describe the symptom complex of urinary urgency, usually accompanied by frequency and nocturia, with or without urge urinary incontinence, in the absence of urinary tract infection or other obvious pathology.1
Epidemiological studies in North America have reported a prevalence of overactive bladder in women of 16.9%, and the prevalence increases with agefrom 4.8% in women under 25 years to 30.9% in those aged over 65 years.2 Prevalence data from Europe are similar, with frequency the most commonly reported symptom , and 54% reporting urgency and 36% urge incontinence.3
The symptoms of overactive bladder are most likely due to involuntary contractions of the detrusor muscle during the filling phase of the micturition cycle abnormalities in afferent sensation may also play a role. Detrusor overactivity1 is mediated by acetylcholine induced stimulation of muscarinic receptors
Read Also: Is Bladder Cancer Slow Growing