Ways To Minimize Urine Leakage After A Hysterectomy
Routine bladder control can be a difficult feat for many women after a hysterectomy, but there are things you can do to minimize leaking.
If you’re experiencing urine leakage after a hysterectomy, take these steps to minimize the problem.
Make life easier on yourself by preventing accidents and embarrassing leaks.
Do You Need Cervical Screening After A Hysterectomy
You will not need cervical screening if both your uterus and cervix are removed. If the cervix is left behind, the PAP smear may be advised.
Sometimes, even after a total hysterectomy, especially if done for a cancerous condition, a PAP smear may be recommended to detect any cancerous changes in the surrounding area.
If your mother took the drug diethylstilbestrol while she was pregnant with you, regular PAP tests are recommended because DES exposure in the uterus increases your risk of cervical cancer.
Is Urinary Incontinence Normal After Hysterectomy
The most common after-hysterectomy problem is pelvic floor dysfunction. However, the most common type of pelvic floor dysfunction is urinary incontinence, and often after the surgery. But not all women suffer from it only about 30% or so experience one or more symptoms of post-surgical SUI/stress voiding.
Hysterectomy does not cause urinary incontinence. Loss of support for the bladder neck and urethra is what causes it.
The incidence of urinary incontinence after hysterectomy varies depending on which surgical technique is used. The highest incidence is after vaginal hysterectomies because these procedures disrupt supporting structures of the bladder more than abdominal procedures.
About half of patients who have vaginal hysterectomy experience urinary incontinence after their surgery, most often due to injury to the urethra or bladder neck during the procedure.
After an abdominal hysterectomy, about 10-20 percent of women will experience stress-related urinary incontinence, but the risk seems to increase to 40-50 percent when combined with other pelvic surgery such as bladder or vaginal surgery.
You May Like: How To Fix A Fallen Bladder
Any Side Effects Of The Sling Procedures
Generally, just local discomfort.
For same reasons as vaginal stabilization post-hysterectomy, we sometimes see hypertonicity of pelvic floor muscles post-sling procedure, and pelvic floor PT is highly effective at reducing the hypertonicity, and the concomitant pelvic pain or leakage that is associated with it.
In rare cases, if the tape is compressing the urethra, the client is unable to pee on their own, post-procedure. In this case, the standard of care is to have the tape loosened, or removed, as quickly as possible. Otherwise, there is a risk of needing to self-catheterize.
Studies show that when the tape is compressing the urethra, there are excellent outcomes if it is loosened in the first 7-10 days, so dont wait to check in with your surgeon.
So if youve had this procedure done, and peeing is not getting easier after a day post-procedure, you need to get your cute butt back to the surgeons office, pronto.
What Are The Different Types Of Hysterectomies
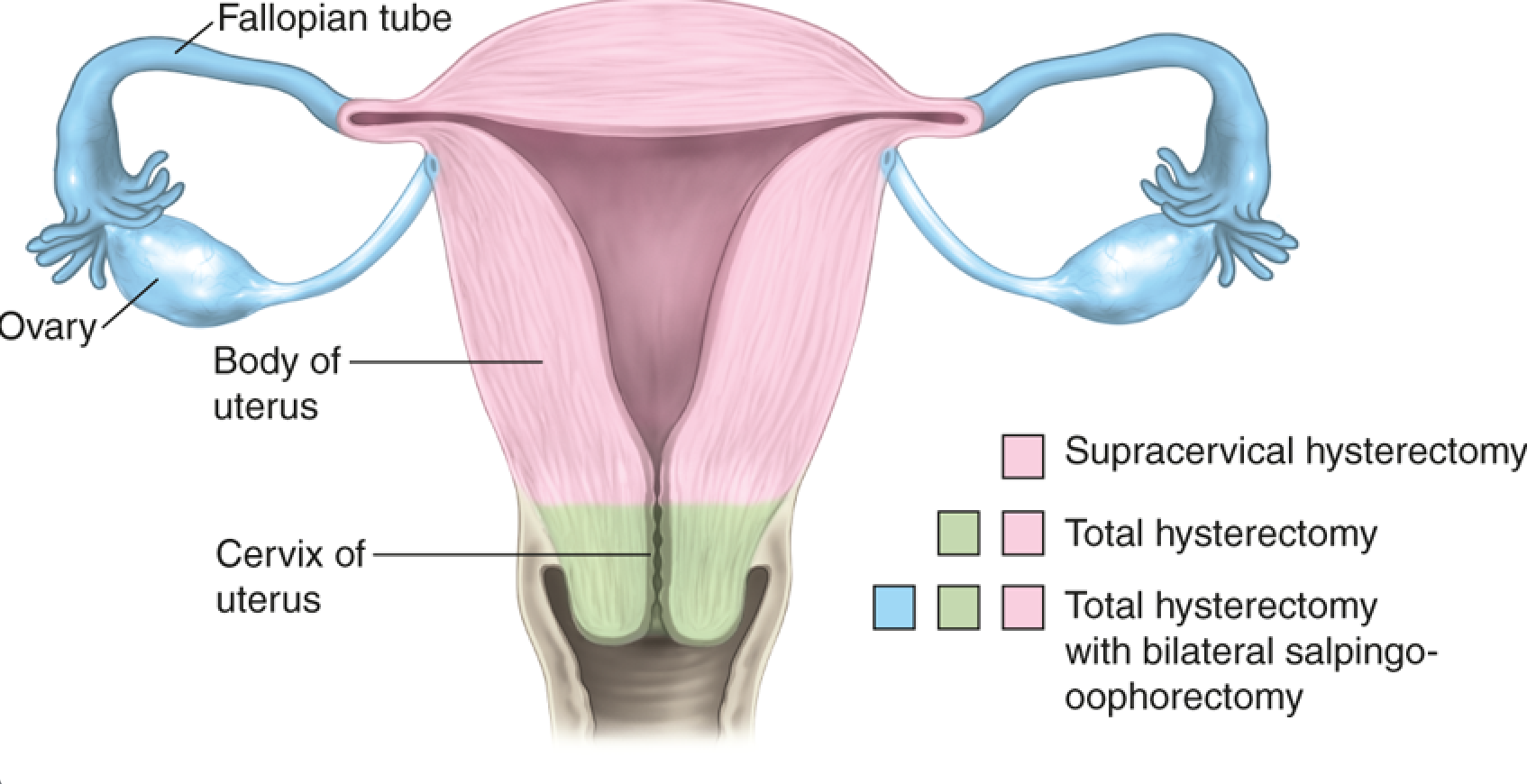
To fully envision how your body may change after a hysterectomy, you need to know the different types of surgery. Dr. Macey may recommend one of three types of hysterectomies:
- Partial or supracervical hysterectomy: Upper part of the uterus is removed, while the cervix is left in place
- Total hysterectomy: Entire uterus and cervix are removed
- Radical hysterectomy: Uterus, cervix, and upper part of your vagina are removed
Although a hysterectomy doesnt include your ovaries or fallopian tubes, they may also be removed depending on the reason for your surgery. When one or both ovaries are removed, the procedure is called an oophorectomy. Removal of your fallopian tubes is called a salpingectomy.
Don’t Miss: Can Being Constipated Affect Your Bladder
Bladder Function After Hysterectomy
A number of studies have shown no short-term urinary adverse effects of hysterectomy. However, longer-term follow-up shows an increased risk. This large Swedish study over a 31 year period showed a 2.4-fold risk of urinary stress incontinence surgery in women who had hysterectomies for benign conditions. This Danish study of women aged 40 to 60 years also showed a 2.4-fold risk of stress incontinence in women who had a hysterectomy. A small China study showed a 7.6% rate of pelvic organ prolapse and 67.4% rate of urinary incontinence 6 years post total hysterectomy.
A systematic review of 12 MEDLINE articles that used original data published over a 32 year period âwas consistent with increased odds for incontinence in women with hysterectomyâ¦.Among women who were 60 years or older, summary odds ratio for urinary incontinence was increased by 60% but odds were not increased for women younger than 60 years.â Another review of this same data consistently found an increased risk of incontinence many years after hysterectomy. However, this study also concluded that âOral estrogen replacement therapy seems to have little short-term clinical benefit in regard to incontinence and is associated consistently with increased risk of incontinence in women aged 60 years and older in epidemiologic studies.â
Natural Treatment For Loss Of Bladder Control
As a ND, I always prefer the natural treatment first Do no harm is the guiding principle for naturopathic medicine. When it comes to natural treatments for loss of bladder control with or without hysterectomy, Ive been using a Chinese herbal formula, Better WOMAN, for my patients for more than two years now. I have found that most women experience significant improvement in their urinary leakage well within two months.
I also recommend Kegel exercises to enhance the tone of the pelvic floor, and sometimes some special pelvic floor rehabilitation techniques with womens heath physical therapies.
Also Check: Sjogren’s Syndrome And Bladder Problems
What Happens After A Hysterectomy
The amount of time you spend in the hospital following a hysterectomy varies depending on what kind of surgery you had. Your healthcare provider will want to monitor you and ensure there are no signs of complications like blood clots or bleeding. You’ll walk around as soon as possible after your surgery to prevent blood clots in your legs.
If you had an abdominal hysterectomy, you might stay in the hospital for a few days. Vaginal and laparoscopic hysterectomies are less invasive and typically do not require any overnight stay in the hospital.
Your healthcare provider will go over recovery instructions, including restrictions to your day-to-day activities. Be sure to discuss any concerns you have about your recovery or the procedure.
How Does Premature Menopause Affect Your Body
Youll go through the same changes during premature menopause as you would if you entered menopause naturally. The sudden loss of hormones triggers all the classic symptoms, including:
- Hot flashes and night sweats
- Vaginal dryness
Since estrogen affects tissues throughout your body, system-wide changes take place such as:
- Loss of bone density and increased risk for osteoporosis
- Accelerated skin aging due to dehydration and loss of collagen
- Changes in blood vessels that increase the risk for cardiovascular disease
Although hormone-related changes following an oophorectomy can be difficult and affect your quality of life, its important to know that medical therapies and rejuvenation with the advanced MonaLisa Touch® are available to alleviate premature menopause symptoms.
Read Also: How To Treat A Leaky Bladder
Visit A Pelvic Floor Physical Therapist
If you are experiencing urinary incontinence, there is a good chance that your pelvic floor muscles may not function properly.
A pelvic floor physical therapist can help you restore function to these muscles, which may help improve your urinary control.
Some benefits of working with a physical therapist include:
- Learning exercises to helpstrengthen your pelvic floor muscles on your own
- Practicing the relaxation of your pelvic floor muscles to maintain bladder control and
- Dealing with stress and anxiety that may contribute to urinary leakage
Rehabilitation of the pelvic floor muscles has been shown to decrease the risk of future urinary tract infections, which is another benefit of visiting a physical therapist.
Bladder Problems After Hysterectomy And What To Do About It
It is not uncommon that women complain about bladder problems after hysterectomy like lack of bladder control, bladder spasms, a burning feeling, and frequent visits to the bathroom.
We all know that having problems with our bladder is a part of getting old.
But, if you have to face problems like incontinence in your early forties, that is hard to accept. However, there is often no need for concern, as most of these problems will resolve in time. A hysterectomy is a major operation that can weaken the ligaments or damage supporting structures.
After the hysterectomy, your bladder will miss the support it had from your uterus, and its place in the pelvis will be different. During your hysterectomy recovery period, the pelvis tissues will heal, and your feeling and control of the bladder will gradually return.
Sometimes these problems bladder after hysterectomy persist. Bladder issues that may need medical attention are:
- bladder injury
Don’t Miss: What Doctor To See For Bladder Infection
Here’s What Really Happens To Your Body After You’ve Had A Hysterectomy
You’ve probably heard about hysterectomies in passing, but quite possibly don’t know much about the specifics of them, despite the fact that they’re very common within the United States. In fact, nearly 500,000 women undergo a hysterectomy every year, making the procedure the second-most common surgery among women within the country .
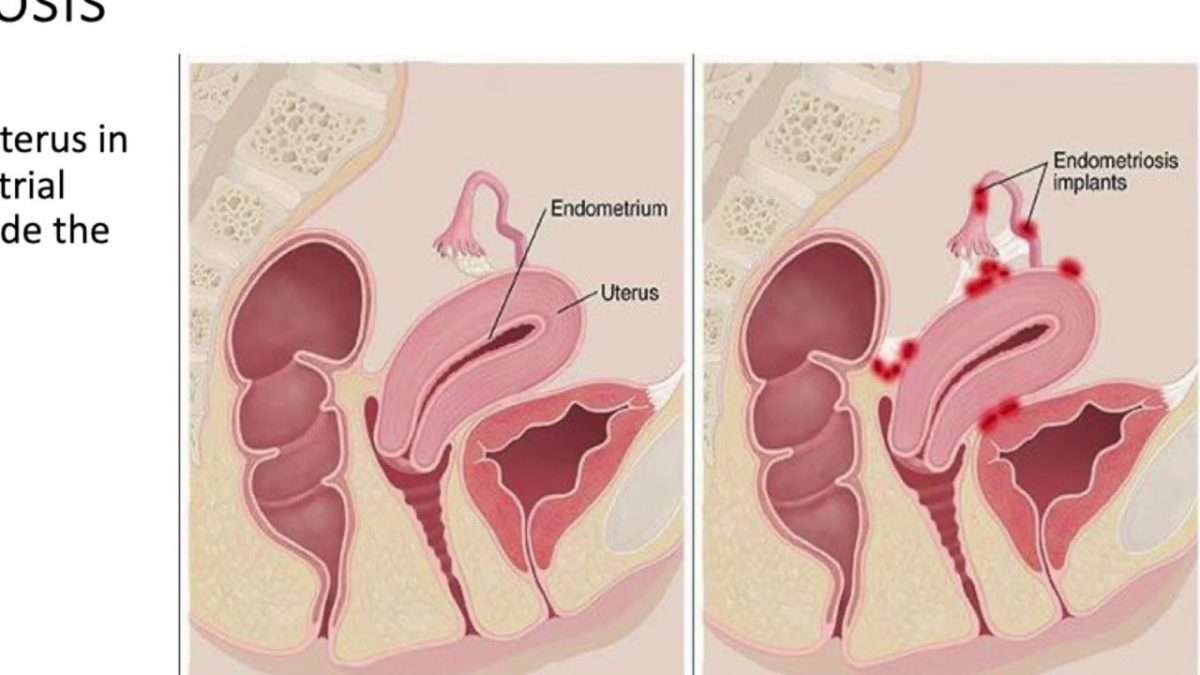
As WebMD tells us, a hysterectomy is, quite simply, the surgical removal of the uterus. There’s a lot more to this surgery, however, particularly in the healing process and aftermath of the surgery. In many cases of a hysterectomy, the fallopian tubes and ovaries might be removed, as well, depending on the circumstances. There are lots of benefits to the removal of all three, such as protecting against ovarian cancer and preserving hormonal levels, per Yale News. But for the most part, a standard hysterectomy typically involves only the removal of the uterus. Some of the most common reasons for going through with this major surgery include the presence of cancer, endometriosis, uterine fibroids, infection, abnormal bleeding, uterine prolapse, and more. The general consensus is that, while hysterectomies are certainly major surgeries, the risk is ultimately worth it, due to the reduction or elimination of disease, pain, or negative side effects .
How Will I Feel After A Hysterectomy
Physically
After a hysterectomy, your periods will stop. Occasionally, you may feel bloated and have symptoms similar to when you were menstruating. It is normal to have light vaginal bleeding or a dark brown discharge for about four to six weeks after surgery.
You may feel discomfort at the incision site for about four weeks, and any redness, bruising or swelling will disappear in four to six weeks. Feeling burning or itching around the incision is normal. You may also experience a numb feeling around the incision and down your leg. This is normal and, if present, usually lasts about two months. It’s normal to have scarring, both internally and externally. Laparoscopic surgeries will cause smaller, less visible scars as opposed to abdominal hysterectomy.
If the ovaries remain, you should not experience hormone-related effects. If the ovaries were removed with the uterus before menopause, you may experience the symptoms that often occur with menopause, such as hot flashes. Your healthcare provider may prescribe hormone replacement therapy to relieve menopausal symptoms.
People who undergo a subtotal hysterectomy may continue to have a light period for a year after the procedure. This happens because small amounts of the endometrial lining can remain in the cervix, causing light periods.
Emotionally
Emotional reactions to a hysterectomy vary and can depend on how well you were prepared for the surgery, the reason for having it and whether the problem has been treated.
Read Also: Can I Have A Bladder Infection Without Pain
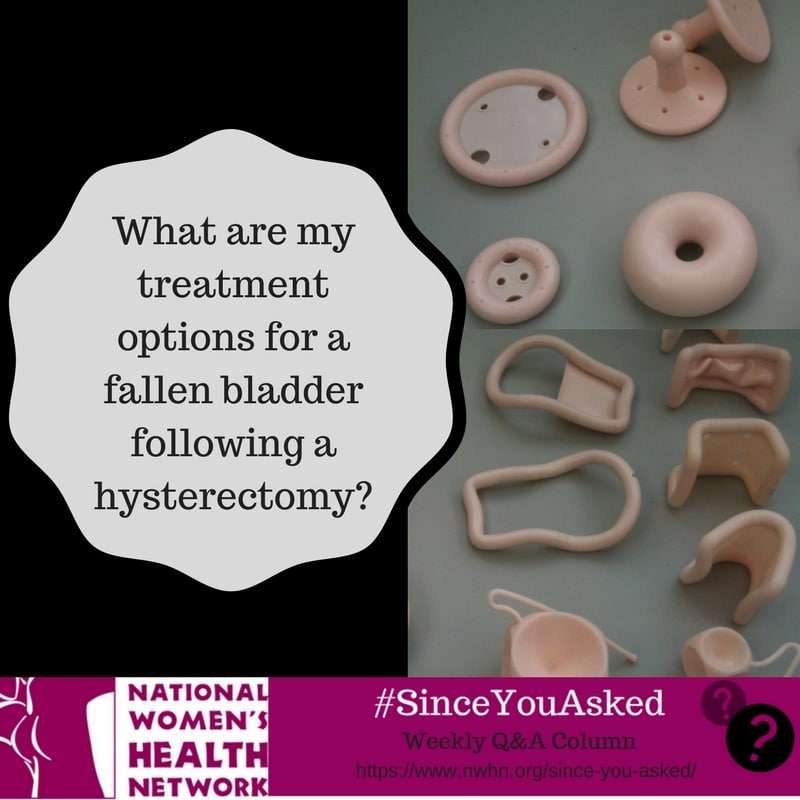
Treatment Of A Vault Prolapse
A vaginal vault prolapse is a defect that occur highs in the vagina, entailing a surgical approach through either the vagina or the abdomen. Generally, the abdomen is the entry of choice for a severe vaginal vault prolapse.
The surgical procedure for correction of vault prolapse is a sacrocolpopexy, in which the surgeon attaches the vagina to a strong ligament over the backbone using a special mesh. This procedure can be performed either as a keyhole operation or as an open procedure.
Oxford is one of few centres in the UK that can offer the laparoscopic technique, as it requires a high level of laparoscopic skills and special equipment. We perform many laparoscopic sacrocolpopexy operations and have published our results in peer-reviewed journals.
What Is A Hysterectomy
A hysterectomy is the surgical removal of the uterus, and most likely, the cervix. Depending on the reason for the surgery, a hysterectomy may involve removing surrounding organs and tissues, such as the fallopian tubes and ovaries. The uterus is where a baby grows during pregnancy. It’s lining is the blood you shed during your menstrual period. You lose the ability to get pregnant and you will not get your period after a hysterectomy.
You May Like: Can Bladder Cancer Be Cured If Caught Early
What Are The Most Common Side Effects Of A Hysterectomy
Some of the most common side effects of a hysterectomy are vaginal drainage and irritation at the incision sites.
If your ovaries were removed at the time of your hysterectomy, you may experience menopausal symptoms such as:
Your doctor will discuss treatment options to avoid the side effects of menopause mentioned above.
How To Deal With Changes After A Hysterectomy
A hysterectomy that also involves the removal of ovaries results in the permanent cessation of a womans menstrual cycle. This condition is known as surgical menopause or surgery-induced menopause. Hormonal changes also take place during menopause for which the doctor may recommendhormone replacement therapy .
Menopause results in a decrease in the estrogen hormone that gives rise to signs and symptoms of menopause. HRT aims at making up for the loss of estrogen by replacing it with synthetic estrogen.
If you experience vaginal dryness and pain during sex, you can use a vaginal lubricant just before performing the carnal act.
You may feel depressed or stressed due to the loss of one or more of your reproductive organs. You can relax and destress yourself by indulging in massage therapy, deep breathing, meditation, and yoga.
Also Check: How To Control Bladder Pressure
Why Is A Hysterectomy Performed
Healthcare providers perform hysterectomies to treat:
- Abnormal or heavy vaginal bleeding that is not controlled by other treatment methods.
- Severe pain with menses that is not controlled by other treatment methods
- Leiomyomas or uterine fibroids .
- Increased pelvic pain related to the uterus but not controlled by other treatment.
- Uterine prolapse that can lead to urinary incontinence or difficulty with bowel movements.
- Cervical or uterine cancer or abnormalities that may lead to cancer for cancer prevention.
- Conditions with the lining of your uterus like hyperplasia, recurrent uterine polyps or adenomyosis.
Sex Drive And Functioning
Research shows that a woman’s sex drive after a hysterectomy tends to actually be the same or better, perhaps due to a reduction in symptoms like pain or bleeding. Every woman is different, however, and some women do notice a reduced libido after surgery.
Besides a change in sex drive, some women experience physical changes that affect their sexual functioning, such as:
- Difficulty reaching orgasm
- Vaginal shortening
- Loss of vaginal lubrication
If you are experiencing a loss of sexual desire or functioning after your hysterectomy, be sure to reach out to your healthcare provider for a proper evaluation and treatment plan. Your healthcare provider can discuss several therapies with you, including non-medication and medication options like:
- Sexual education and partner involvement
Also Check: Why Is My Bladder Constantly Leaking
What Is The Most Profound Change You Will Experience
Being told you may need a hysterectomy is a difficult and deeply emotional experience because it means your menstrual periods stop, and you wont be able to get pregnant. Dr. Macey only recommends a hysterectomy when all other treatment options have been considered tried, if possible and failed to improve your symptoms.
The most common health conditions treated with a hysterectomy — uterine fibroids, endometriosis, abnormal uterine bleeding, and uterine prolapse — can often be treated with procedures that preserve your uterus, but it depends on the severity of your problem and your overall health. If you have cervical cancer, uterine cancer, or severe uterine hemorrhage, hysterectomy may be the best choice for your health.
What Are The Long
Following any type of hysterectomy, youll no longer have your period. You also cant get pregnant. These are permanent effects of having a hysterectomy.
Problems with organ prolapse can happen after a hysterectomy. A 2014 study of more than 150,000 patient records reported that 12 percent of hysterectomy patients required pelvic organ prolapse surgery.
In some organ prolapse cases, the vagina is no longer connected to the uterus and cervix. The vagina can telescope down on itself, or even bulge outside the body.
Other organs such as the bowel or the bladder can prolapse down to where the uterus used to be and push on the vagina. If the bladder is involved, this can lead to urinary problems. Surgery can correct these issues.
Most women do not experience prolapse after hysterectomy. To prevent prolapse problems, if you know you are going to have a hysterectomy, consider doing pelvic floor exercises to strengthen the muscles supporting your internal organs. Kegel exercises can be done anytime and anywhere.
If you have your ovaries removed during the procedure, your menopause symptoms can last for several years. If you dont have your ovaries removed and havent gone through menopause yet, you may begin menopause sooner than expected.
If you have your ovaries removed and go into menopause, some of your symptoms may impact your sex life. Sexual side effects of menopause can include:
- vaginal dryness
- pain during sex
- anesthesia side effects
- bowel blockage
Read Also: What To Avoid With Bladder Infection