What Is Bladder Prolapse Surgery With Mesh
Bladder prolapse surgery is most commonly performed through the vaginal entrance. They can also do it abdominal but doctors prefer transvaginal as it is easier, faster, and not as invasive. What they aim to do, is to settle the bladder in its original position and mobilize it. For this, they use a surgical mesh that is made of synthetic material or animal tissue.
To reinforce the vaginal wall the surgeon will insert a mesh through an incision in the anterior wall of the vagina. The vaginal wall is straightened and the bladder is then being supported.
Depending on a womans condition and the complexity of the procedure, they do bladder lift surgery with regional, or local anesthesia, or if necessary, under general anesthesia.
A good thing to know about this surgery is that most often, they release women from the hospital the same day after the surgery.
Are There Less Invasive Treatments For Bladder Prolapse
In recent years the doctors are trying to avoid the procedure as long as it is possible. They test other less invasive techniques every day, and some of them show great results.
Electrical stimulation and a procedure called biofeedback can help to straighten the pelvic muscles.
For electrical stimulation, they attach a probe to another medical device that measures and delivers small electrical currents. The probe aims at the muscles group within the area of the vagina and makes contractions. The result is that these muscles become stronger.
Another less intrusive stimulation is electrical stimulation with less power which they perform from outside of the body. This treatment magnetically stimulates the pudendal nerve .
In biofeedback, the doctors are monitoring the vaginal muscle activity of the vagina and the pelvic floor, using a specific sensor. After that, different exercises can be prescribed to straighten these muscles.
But if symptoms of the bladder prolapse start interfering with a womans life or if she is not responding correctly to a treatment, bladder support surgery might be the only solution.
Anterior Colporrhaphy With Graft
A biologic or synthetic graft may be used to provide extra support to the weakened tissues. It can be sutured to the cardinal-uterosacral ligament complex proximally, the endopelvic fascia distally, and the obturator fascia laterally.
The initial part of the technique is similar to that of standard anterior colporrhaphy . The graft is then trimmed to a trapezoid shape, with the size tailored to the dimensions of the anterior vaginal wall. Proximally, 2 sutures polyglactin) are taken through the cardinal ligaments. Distally, another 2 sutures are taken through the pericervical fascia close to the pubic bones, 1 on each side. The graft is secured to these sutures, and lateral sutures are used to secure the graft to the obturator fascia.
Ready-to-go kits have been developed to speed up the repair process and reduce the need for extensive dissection and suturing. These kits usually include the graft body , the graft arms and legs, and the passers needed for guiding the graft arms through the supporting structures . With the Gynemesh, Prolift Anterior, and Perigee, the graft is secured via the transobturator approach. The Elevate anterior and Uphold LITE are inserted using a single incision. The Elevate anterior has 4 arms with 2 distal arms secured into the obturator membrane and fascia, and the posterior arms are inserted into the sacrospinous ligaments. The Uphold LITE has only 2 anchors that are inserted into the sacrospinous ligaments.
Recommended Reading: Best Natural Cure For Bladder Infection
Prolapse Surgery Success Rate
About a third of women who have prolapse surgery need more than one operation because there is a 25-30% chance the prolapse can return or a different type of prolapse develops. For example, a prolapse of the womb can occur after an operation for prolapse of the vagina and vice versa.
Prolapse surgery usually improves or cures the symptom of something coming down below or the lump in the vagina. Symptoms that relate to bladder and bowel problems, including constipation or incontinence, are not always improved. Similarly, problems with your sex life may not be improved with surgery.
In some cases, some new bowel or bladder symptoms develop after prolapse surgery, which may require further treatment in the future, including further surgery. Some women develop incontinence after prolapse surgery and some have problems emptying their bladder and need to use a catheter afterwards. This problem usually gets better with time. There is a small risk of venous thrombosis with any pelvic surgery. To reduce this risk you will be given an injection every day and some anti-embolic stockings to wear.
Possible Risks And Side Effects Of Vaginal Prolapse Repair

Complications differ depending on the organ involved. However, most side effects are rare. Possible complications include:
- Vaginal sores for those with a bulging uterus
- Pain and discomfort during sex
- Constipation or diarrhea
Copyright © All About Women Online Medical Marketing Services and Search Engine Friendly Web Design by SEO Advantage, Inc. Site info
Gainesville and Lake City OB/GYN CareOB/GYN doctors at All About Women, Obstetrics & Gynecology offer personalized, technologically advanced obstetrics and gynecology services from Board Certified OB/GYB physicians. Besides expert women’s healthcare, permanent birth control and prenatal care, OB/GYN doctors also offers advanced hysterectomy surgery in and around the Gainesville area.
Women’s Health Care in Alachua & Columbia CountiesWith offices in Gainesville and Lake City, Florida, All About Women, M.D. provides expert OB/GYN services covering the entire range of women’s healthcare needs. Our OB/GYN physicians and nurse midwives provide expert care during pregnancy as well as state of the art in-office treatments for gynecologic disorders including Novasure endometrial ablation to treat/stop heavy menstrual bleeding.
Also Check: How Do Poise Bladder Supports Work
What Is The Treatment For A Fallen Bladder
There are a few treatment options a person may have when it comes to treating a fallen bladder, which typically affects female patients. In some cases, the symptoms of this condition are so mild that a woman might choose to refuse treatment. If the symptoms of this condition are troublesome, however, a doctor may recommend the placement of a device in the vagina. When a person has a severe case of this condition, surgery is often a more reliable treatment. Additionally, some doctors may recommend trying electrical stimulation or hormone therapy in order to help strengthen the vital muscles of the pelvic floor.
One of the most common treatments for a fallen bladder is referred to as a pessary. This is a medical device a doctor places into a patient’s vagina to hold the bladder in its proper place. A pessary does not remain in place permanently, however. Instead, it is usually removed and cleaned periodically. With many types of pessaries, a patient can take care of this maintenance on her own. In some cases, however, doctors have to remove and clean the devices for their patients.
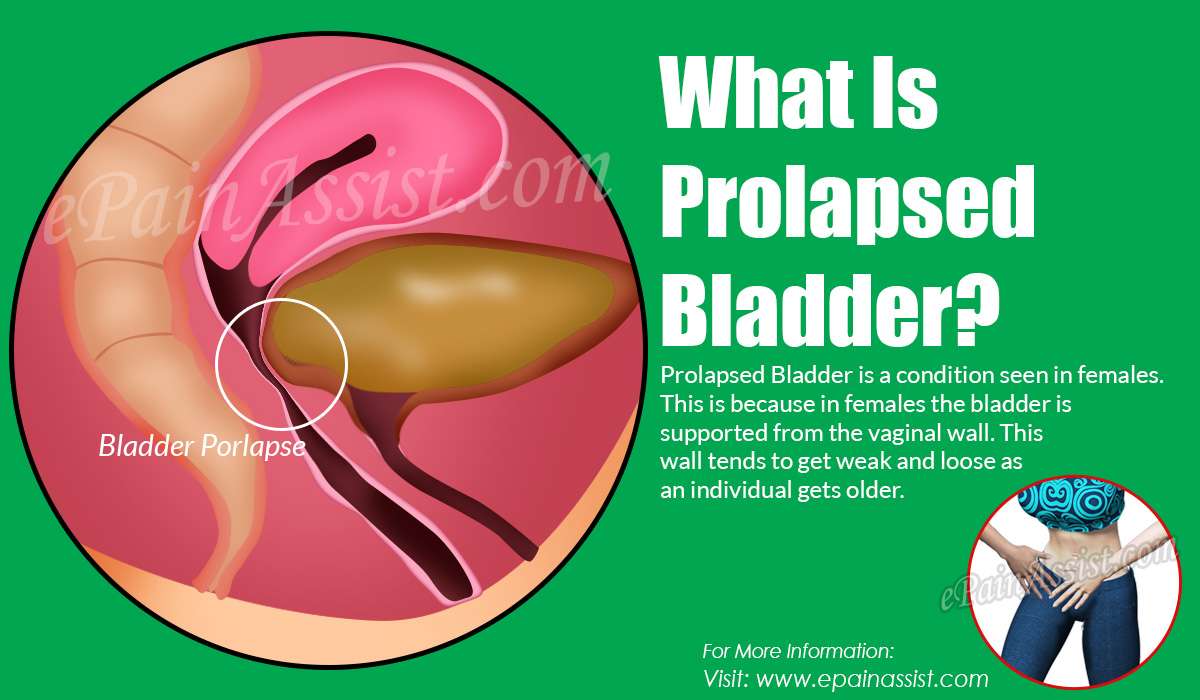
Risk Factors And Other Causes Of A Prolapsed Bladder
Prolapsed bladders in women are commonly associated with menopause. The lower levels of estrogen associated with menopause can cause the vaginal walls to weaken. If they deteriorate enough, the bladder is no longer supported and can fall into the vagina. This can cause urinary problems such as stress incontinence.
Other risk factors for bladder prolapse are:
- Childbirth
- Surgery, such as a hysterectomy
- Constipation or irregular bowel movements
- Excessive strain on the pelvic muscles from things like long-term constipation, lifting heavy objects or weight gain
- Chronic coughing
Don’t Miss: Will Bladder Infections Go Away By Themselves
Is A Pessary Better Than Surgery
Although POP surgery has several advantages over pessary treatment, the risk of complications is higher and it might be less cost-effective. Since previous studies have shown promising results with pessary treatment, it might be an equivalent option in the treatment of POP, probably with less risk and lower cost.
Pfmt Can Be Effective For Mild Prolapse But Is Usually Not Successful For Moderate And Advanced Prolapse
Unless another health problem is present that would require an abdominal incision, the bladder and urethra are usually repaired through an incision in the wall of the vagina. Many women have a vaginal pack inserted at the end of a prolapse operation, to prevent bleeding. This makes sexual intercourse impossible.
Don’t Miss: New Drug For Bladder Cancer
What Are The Symptoms Of Pop
Some women do not notice symptoms at all. Other women will be told they have a prolapse when they have a routine OB/GYN exam.
Unfortunately, many women have chronic uncomfortable symptoms from a prolapse, including back or groin pain, pressure in the pelvic area, the feeling that something is coming out of the vagina, painful intercourse, or spotting and bleeding.
Bladder Prolapse Causes Symptoms And Treatment
If something feels wrong with your vagina, paired with pelvic and lower back discomfort, you may have a prolapsed bladder. Find out what you can do about it!
You may notice something feels wrong with your vagina. You may feel extra tissue in your vagina that feels a little bit like a ball. Paired with pelvic and lower back discomfort, this may be a sign that you have a prolapsed bladder. Use this guide to understand common bladder prolapses causes, symptoms and treatment options.
Recommended Reading: How To Get Rid Of A Bladder Infection Without Antibiotics
Stages Of Bladder Prolapse
The severity of bladder prolapse can be measured in several ways. Terms such as mild, moderate and severe are not always completely accurate, as they depend on a persons opinion, but are often used in day-to-day conversations to help people understand the severity of the prolapse.A more commonly used grading is:
- Stage 1 the bladder protrudes a little way into the vagina
- Stage 2 the bladder protrudes so far into the vagina that its close to the vaginal opening
- Stage 3 the bladder protrudes out of the vagina
- Stage 4 most severe form, in which all pelvic organs including the bladder protrude out of the vagina.
Many gynaecologists now use the Pelvic Organ Prolapse Quantification system, which measures in centimetres where the prolapse is in relation to the vaginal entrance to ascertain the stage of prolapse.
How Do I Know Which Repair Is Best For Me
As a pelvic-floor surgery specialist, Dr. Christi has more experience in these techniques than most surgeons in Houston, and can confidently determine the best option for you. Not only is she trained as a urologist, but also as a urogynecologist. Because Dr. Christi has many different options at her disposal, you can rest assured that she will recommend the best option and provide the most expert surgery possible.
Read Also: Botox Injections For Bladder Control
Symptoms Of Bladder Prolapse
The symptoms of bladder prolapse depend on the severity of the prolapse, your level of physical activity and the presence of any other type of prolapse.They include:
- urinary stress incontinence leaking urine when coughing, sneezing, laughing, running or walking, or urge incontinence, which is urgently needing to go and leaking on the way
- needing to empty your bladder more frequently
- inability to completely empty your bladder when going to the toilet
- recurrent urinary tract infections
- protrusion of the vaginal wall out through the vaginal entrance
- needing to go back to the toilet immediately after finishing passing urine.
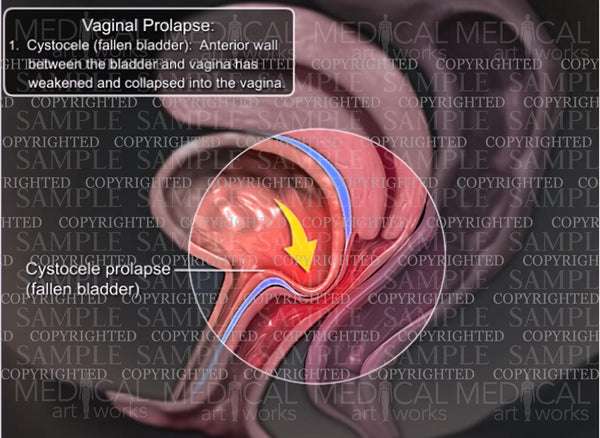
What Is A Cystocele
A cystocele occurs when the wall between a woman’s bladder and her vagina weakens and allows the bladder to droop into the vagina. This condition may cause discomfort and problems with emptying the bladder.
A bladder that has dropped from its normal position may cause two kinds of problems — unwanted urine leakage and incomplete emptying of the bladder. In some women, a fallen bladder stretches the opening into the urethra, causing urine leakage when the woman coughs, sneezes, laughs, or moves in any way that puts pressure on the bladder.
A cystocele is mild — grade 1 — when the bladder droops only a short way into the vagina. With a more severe – grade 2 – cystocele, the bladder sinks far enough to reach the opening of the vagina. The most advanced — grade 3 — cystocele occurs when the bladder bulges out through the opening of the vagina.
Also Check: Bristol Myers Squibb Bladder Cancer
What Exams And Tests Diagnose A Prolapsed Bladder
An exam of the female genitalia and pelvis is usually required in diagnosing a prolapsed bladder. Seeing the bladder bulging into the vagina on examination is diagnostic. In addition, you will be asked to strain/cough/bear down to determine the extent of the bladder prolapse, as well as determine if you have urinary leakage with increased pressure .
For less obvious cases, the doctor may use a voiding cystourethrogram to help with the diagnosis. During the voiding cystourethrogram, a catheter is placed into the bladder through the urethra. The bladder is emptied and then a sterile contrast is passed through the catheter into the bladder until the bladder is full enough to void. A series of X-ray films then are taken during bladder filling and during urination. These X-ray films help the doctor determine the shape of the bladder and the cause of urinary difficulty. The doctor may also test or take X-ray films of different parts in the abdomen to rule out other possible causes of discomfort or urinary difficulty.
After diagnosis, the doctor may test the nerves, muscles, and the intensity of the urine stream to help decide what type of treatment is appropriate.
A test called urodynamics or video urodynamics may be performed at the doctor’s discretion. Urodynamics measures pressure and volume relationships in the bladder and can also assess the function of the urethra and may be crucial in the decision-making of the urologist/urogynecologist.
Prolapsed Bladder Care At Home
For mild-to-moderate cases of prolapsed bladder, the doctor may recommend activity modification such as avoiding heavy lifting or straining. The doctor may also recommend Kegel exercises. These are exercises used to tighten the muscles of the pelvic floor. Kegel exercises might be used to treat mild-to-moderate prolapses or to supplement other treatments for prolapses that are more serious.
You May Like: Robotic Surgery For Bladder Cancer
Is There A Possibility Of Recurrence After Surgery
The results of a study carried out by then Radcliff John Hospital in Oxford show that 10.8 % of women undergoing pelvic organ prolapse surgery have a second or third operation within the next 11 years. The study followed a group of 2099 women that had surgery for POP between 1995 and 2005. Worth mentioning is that of the women that needed repeat surgery, 61,5% needed surgery in a different area than the site of the original operation.
Exams And Tests For A Prolapsed Bladder
An exam of the female genitalia and pelvis, known as a pelvic exam, is required in order to diagnose a prolapsed bladder. A bladder that has entered the vagina confirms the diagnosis.
For less obvious cases, the doctor may use a voiding cystourethrogram to help with the diagnosis. A voiding cystourethrogram is a series of X-rays that are taken during urination. These help the doctor determine the shape of the bladder and the cause of urinary difficulty. The doctor may also test or take X-rays of different parts of the abdomen to rule out other possible causes of discomfort or urinary difficulty.
After diagnosis, the doctor may test the nerves, muscles, and the intensity of the urine stream to help decide what type of treatment is appropriate.
A test called urodynamics or video urodynamics may be performed at the doctor’s discretion. These tests are sometimes referred to as “EKGs of the bladder”. Urodynamics measures pressure and volume relationships in the bladder and may be crucial in the decision making of the urologist.
Cystoscopy may also be performed to identify treatment options. This test is an outpatient office procedure that is sometimes performed on a television screen so the person can see what the urologist sees. Cystoscopy has little risk and is tolerable for the vast majority of people.
Recommended Reading: What Is Overactive Bladder Syndrome
Treatment For Symptomatic Bladder Prolapse
If you have symptoms of bladder prolapse it is recommended that, as for people with no symptoms, you make the same lifestyle changes, do pelvic floor muscle training and treat any chronic cough. Make them part of your routine.
However, sometimes prolapse can be more severe and these measures may not be enough on their own to relieve symptoms.
For these cases, there can be two different approaches:
1. Non-surgical approach vaginal pessaries
A pessary is a device made mostly of silicone. It is inserted in the vagina to support the bladder prolapse and front vaginal wall. Pessaries come in different shapes and sizes.You do not need surgery to put in a pessary. It can be done in the rooms of a pelvic floor physiotherapist, continence nurse or your gynaecologist.
Some women may prefer this option if they wish to avoid or delay surgery, and it may be the safest option for women who are unfit for surgery.You will need regular check-ups with your healthcare professional if you are using a vaginal pessary long-term.
2.Surgical approach
Suggestions may include:
- resting each day.
What Happens During The Procedure
Before the surgery,
- Your gynecologist /urologist will examine your condition and identify the fallen bladder.
- They may discuss the symptoms to confirm the exact reason and may order some additional tests to assess any more damage to the urinary system.
During the surgery,
- Under general anesthesia, an incision is made in the vaginal wall.
- The tissue between the bladder wall and the vaginal wall is tightened with stitches to allow the strengthening of the muscles and ligaments.
- Sometimes, extra tissue may be removed, or tissue grafts are used .
Also Check: Cramping In Bladder Or Uterus