Immunotherapy For Bladder Cancer Has A Long History Including The First Fda
Bladder cancer is the sixth most common cancer in the United States and ninth most common worldwide. Most bladder cancers begin in transitional epithelial cells that make up the inner lining of the bladder. As these tumors grow, they can invade the surrounding connective tissue and muscle. In advanced disease, tumors spread beyond the bladder to nearby lymph nodes or pelvic organs or metastasize to more distant organs, such as the lungs, liver, or bone.
Cancers of the bladder make up about 5% of new U.S. cancer cases each year, mostly in older people. In 2021, there will be an estimated 83,000 new cases diagnosed and approximately 17,000 deaths in the U.S. alone. In 2017, roughly 550,000 new cases and 200,000 deaths due to bladder cancer globally. Men are more likely than women to be affected by bladder cancerabout 75% of new cases and deaths are in menbut the reasons for this gender difference are not clear. Because their disease is likely to recur, or come back, patients with bladder cancer must undergo surveillance for an extended period.
When considered by stage, the 5-year relative survival rates for patients with tumors restricted to the inner layer of the bladder or those with disease localized to the bladder are 96% and 70%, respectively. The rates drop to 34% for those with disease that has spread locally beyond the bladder and to 5% for patients with distant metastases.
Where Do These Numbers Come From
The American Cancer Society relies on information from the SEER* database, maintained by the National Cancer Institute , to provide survival statistics for different types of cancer.
The SEER database tracks 5-year relative survival rates for bladder cancer in the United States, based on how far the cancer has spread. The SEER database, however, does not group cancers by AJCC TNM stages . Instead, it groups cancers into localized, regional, and distant stages:
- Localized: There is no sign that the cancer has spread outside of the bladder.
- Regional: The cancer has spread from the bladder to nearby structures or lymph nodes.
- Distant: The cancer has spread to distant parts of the body such as the lungs, liver or bones.
Genetic Factors In Pathogenesis
Divergent, yet interconnected and overlapping, molecular pathways are likely responsible for the development of noninvasive and invasive bladder tumors. Somatic mutations in fibroblast growth receptor3 and tumor protein p53 in tumor cells appear to be important early molecular events in the noninvasive and invasive pathways, respectively.
FGFR-3, Ras, and PIK3CA mutations occur with high frequency in noninvasive tumors, leading to upregulation of Akt and mitogen-activated protein kinase . Loss of heterozygosity on chromosome 9 is among the most frequent genetic alterations in bladder tumors and is considered an early event.
Large numbers of genomic changes have been detected using karyotyping and comparative genomic hybridization analysis in urothelial carcinoma. Numerically common are losses of 2q, 5q, 8p, 9p, 10q, 18q, and Y. Gains of 1q, 5p, 8q, and 17q are frequently present, and high-level amplifications can be found however, the target genes in the regions of amplifications have not been conclusively identified.
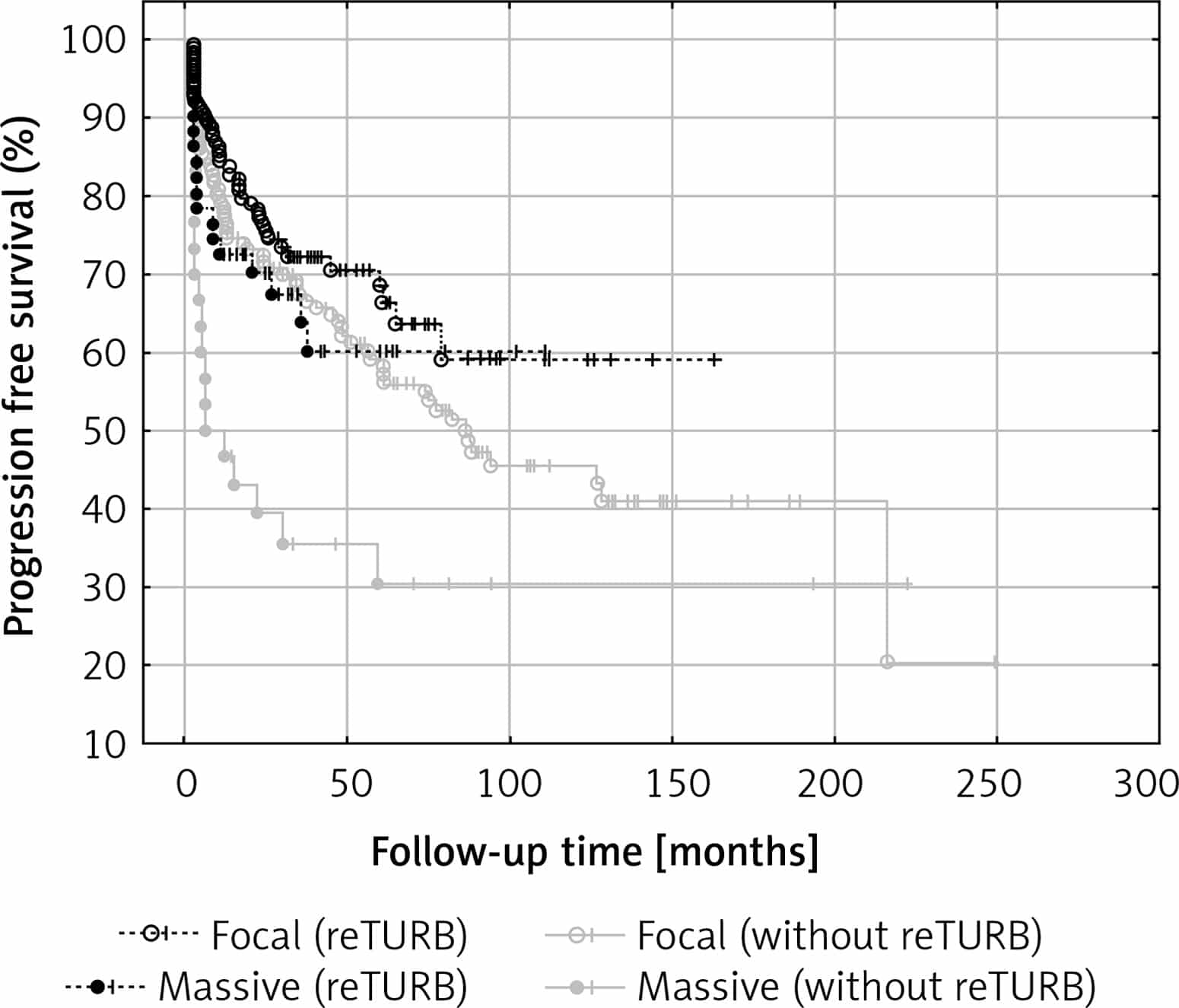
Alterations in the TP53 gene are noted in approximately 60% of invasive bladder cancers. Progression-free survival is significantly shorter in patients with TP53 mutations and is an independent predictor of death among patients with muscle-invasive bladder cancer.
You May Like: Does Diabetes Cause Bladder Problems
Chemotherapy Plus Immunotherapy Before Surgery Is Beneficial For Invasive Bladder Cancer Outcomes
By ckalnen
A new study is the first to report the beneficial use of chemotherapy plus immunotherapy before surgical removal of the bladder in muscle-invasive bladder cancer . Researchers at the University of North Carolina Lineberger Comprehensive Cancer Center led the study, reporting that the regimen reduced the invasiveness of the cancer in 56% of patients in a phase II clinical trial.
The findings were published in the Journal of Clinical Oncology.
Downstaging, or treating tumors so that they become less invasive prior to surgical removal, is an important tool in muscle-invasive bladder cancer, said UNC Linebergers Tracy Rose, MD, MPH, assistant professor at the UNC School of Medicine and lead author of this finding. If we can treat a tumor pre-surgically so that it regresses to a stage where it is superficial and does not invade the bladder muscle wall, the chances of long-term survival are better.
Nearly 25% of all bladder cancers are muscle invasive. Surgical removal of the bladder is performed in many MIBC cases, but often microscopic cancer cells have already spread to lymph nodes, greatly reducing chances of a cure. In these cases, clinicians often use cisplatin chemotherapy before removal of the bladder to reduce tumor volume and kill micro-metastases. Despite this aggressive treatment, more than half of patients see their cancer return within two years.
Filed Under:
Cris Impact In Bladder Cancer
Thanks to groundbreaking advancements in immunology research and clinical trials, immunotherapy has become one of the most promising bladder cancer treatments of our time.
Lloyd J. Old, in partnership with Baruj Benacerraf and Donald Clarke, demonstrated in 1959 that BCG, the tuberculosis vaccine, could inhibit tumor growth in mice. In subsequent years, CRI funded Alvaro Morales of Queens University in Canada, who, in 1980, demonstrated that BCG is effective in the prevention of recurrence of non-muscle invasive bladder cancer in human patients. The FDA approved the use of BCG for superficial bladder cancer in 1990.
In the early 70s my rejection by the National Cancer Institute of Canada to test BCG on superficial bladder tumors included the reviewer comment BCG is not only ineffective and dangerous but a throwback from the stone age of tumor immunology. If I hadnt subsequently applied to and been approved for a grant from CRI, BCG might never have become the standard therapy for the treatment and prevention of early stage bladder cancer.
Alvaro Morales
Other CRI-funded research into bladder cancer includes:
New and developing bladder cancer immunotherapies have the potential to reduce recurrence rates and improve survival rates for patients with bladder cancer. You can explore CRIs current research into bladder cancer in our funding directory.
- Immunomodulators
- Oncolytic Virus Therapy
Don’t Miss: Why Does Coffee Irritate My Bladder
Can We Combine Immunotherapy With Other Treatments
Lab studies have shown that some checkpoint blocker therapies, while potent, are even more powerful when combined with other drugs. Clinical trials are underway at Johns Hopkins and elsewhere to test combinations that can involve the addition of standard therapies such as radiation, chemotherapy or other medications to a checkpoint blocker to rev up the immune system.
Prognosis In Squamous Cell Carcinoma
Tumor stage, lymph node involvement, and tumor grade have been shown to be of independent prognostic value in SCC. However, pathologic stage is the most important prognostic factor. In one relatively large series of 154 cases, the overall 5-year survival rate was 56% for pT1 and 68% for pT2 tumors. However, the 5-year survival rate for pT3 and pT4 tumors was only 19%.
Several studies have demonstrated grading to be a significant morphologic parameter in SCC. In one series, 5-year survival rates for grade 1, 2, and 3 SCC was 62%, 52%, and 35%, respectively. In the same study of patients undergoing cystectomy, the investigators suggested that a higher number of newly formed blood vessels predicts unfavorable disease outcome.
In SCC, the survival rate appears to be better with radical surgery than with radiation therapy and/or chemotherapy. In locally advanced tumors, however, neoadjuvant radiation improves the outcome. Sex and age have not been prognostically significant in SCC.
Don’t Miss: Bladder Neck Contracture After Prostatectomy
Immunotherapy Improves Survival In Advanced Bladder Cancer Patients
by Queen Mary, University of London
An immunotherapy drug called ‘avelumab’ has been shown to significantly improve survival in patients with the most common type of bladder cancer, according to results from a phase III clinical trial led by Queen Mary University of London and Barts Cancer Centre, UK.
This is the first time an immune therapy has resulted in a survival advantage in this setting in bladder cancer, and will potentially benefit thousands of patients each year.
The results were published in the New England Journal of Medicine and found that avelumab led to a 31 percent reduction in risk of death of bladder cancer and extended median survival in advanced bladder cancer by more than seven months.
Approximately 550,000 new cases of bladder cancer are diagnosed each year , making it the tenth most common cancer worldwide. This trial focused on the group of these patients whose cancer had spread beyond the bladder , which is difficult to treat and results in more than 200,000 deaths each year worldwide.
Chemotherapy is the current initial standard of care in the treatment of these advanced cancers. After chemotherapy is finished, patients are checked regularly because the cancer tends to return quickly. When it returns it is difficult to treat and outcomes are poor.
More information:New England Journal of MedicineJournal information:
Immunotherapy In The Treatment Of Urothelial Bladder Cancer: Insights From Single
- 1State Key Laboratory of Oncogenes and Related Genes, Shanghai Cancer Institute, Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 2Department of Urology, Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
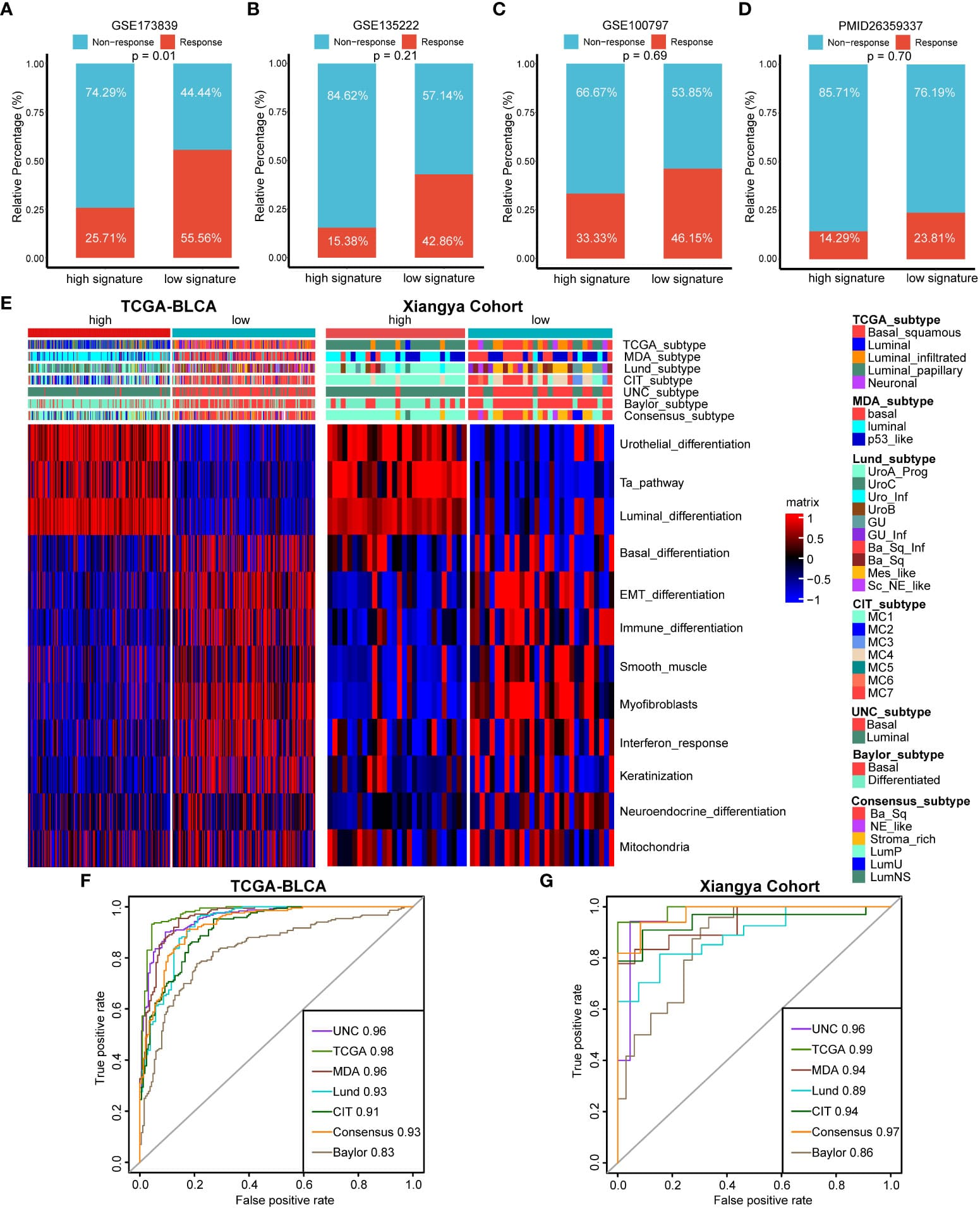
Urothelial bladder cancer is a global challenge of public health with limited therapeutic options. Although the emergence of cancer immunotherapy, most notably immune checkpoint inhibitors, represents a major breakthrough in the past decade, many patients still suffer from unsatisfactory clinical outcome. A thorough understanding of the fundamental cellular and molecular mechanisms responsible for antitumor immunity may lead to optimized treatment guidelines and new immunotherapeutic strategies. With technological developments and protocol refinements, single-cell approaches have become powerful tools that provide unprecedented insights into the kaleidoscopic tumor microenvironment and intricate cell-cell communications. In this review, we summarize recent applications of single-cell analysis in characterizing the UBC multicellular ecosystem, and discuss how to leverage the high-resolution information for more effective immune-based therapies.
Recommended Reading: How Do They Treat Bladder Cancer
Is There Any Preparation Involved
Its important that you follow your doctors instructions for what to do before and after the procedure. Tell your doctor about all the medications you take. Certain immunosuppressants, antimicrobial therapies, and radiation therapies can interfere with BCG treatment.
Youll be advised to limit your fluid intake for four hours prior to the procedure. You might be told to avoid caffeine for a few hours longer than that, because its a diuretic and could make things more difficult.
Youll be asked to urinate just before the procedure so youll be able to hold the medication in your bladder for several hours.
What Can I Expect Following Treatment
You may be advised to drink plenty of fluid to flush the rest of the medication from your bladder.
For six hours after each treatment, youll have to be very careful when you urinate to avoid transmitting BCG to others. Men should urinate while seated to avoid splashing.
Disinfect the urine by adding 2 cups of bleach into the toilet. Let it stand for about 20 minutes before flushing. You should also wash your genital area very carefully after you urinate, so your skin doesnt become irritated from the BCG. Wash your hands thoroughly, too.
Men can pass BCG to their partner during sex. For that reason, you should avoid sex for 48 hours after each treatment. Use a condom between treatments and for six weeks following your final treatment.
Women should avoid getting pregnant or breastfeeding while on BCG therapy.
Treatment is usually given every week for six weeks. After that, you might need to do it once a month for six months to a year.
One benefit of BCG is that while it affects the cells in your bladder, it doesnt have a major effect on any other part of your body. But there can be a few side effects such as:
When comparing BCG to other bladder cancer treatments, its important to remember that treatment isnt the same for everybody. Some of the factors that determine your options are:
- type of bladder cancer
- your age and general health
- how well you tolerate certain treatments
Recommended Reading: Can Zantac Cause Bladder Cancer
The Importance Of Keeping The Promise And Potential Of Immunotherapy Alive
Almost 40 percent of men and women will be diagnosed with cancer during their lifetime. Thankfully, in this day of medical advancements and innovation, cancer is no longer a certain death sentence. More than 15.5 million people lived beyond a cancer diagnosis as of Jan. 1, 2016, and that number is expected to surpass 20 million by 2026. The goal in cancer treatment now is to target care more precisely to patients through individualized health care. This is called precision medicine, and it is an especially welcome change for cancer patients who traditionally have been exposed to treatment such as chemotherapy and radiation that attacks their cancer but often damages healthy tissue in the process.
Precision medicine is at the heart of immunotherapy, currently one of the hottest areas of cancer research. Immunotherapy is a new approach that harnesses the power of our immune systems to identify and control diseases such as cancer. Immunotherapy is being studied in just about every type of cancer. The number of cancers successfully treated by immunotherapy stands at 15 and growing and includes skin, lung, kidney and bladder cancers.
Starting Immunotherapy: What To Expect
The FDA has approved several immunotherapy drugs to treat bladder cancer:
Once you and your doctor decide to start one of these treatments, it helps to know a bit about what you can expect while youâre getting it.
How do you get immunotherapy?
To get immunotherapy, youâll go to a treatment center on a regular schedule to get the medicine through an infusion, a tube that goes into a vein. Your doctor will decide how many rounds of treatment you need.
Your doctor will order some lab tests before and during your treatment to see how your body responds to the drug.
You take the medicine through a tube that goes in one of your veins.
A doctor or nurse will look after you when youâre getting the IV to make sure you donât have any bad reactions or side effects. If you do, your doctor might slow down the infusion or delay or stop the treatment.
Speak up if you feel any of these while youâre getting treatment:
Some immunotherapy drugs can also affect your ability to have children. Talk to your doctor before you start treatment to figure out the options you have if you want to have a baby in the future.
Recommended Reading: What Happens When You Remove Your Bladder
Heres How The Other Fda
- Pembrolizumab can be given for locally advanced or metastatic bladder cancer that resists standard chemotherapy drugs.
- Pembrolizumab or atezolizumab can be given to people too sick to receive chemotherapy.
- Atezolizumab can be given to people who have metastatic bladder cancer with high levels of PD-L1 that has not been previously treated and who also cannot receive cisplatin chemotherapy.
Researchers are also gaining a better understanding of who is likely to respond to these drugs and how to make them work better in combinations.
The emergence of checkpoint inhibitors has been a revolution for some people who have highly aggressive, life-threatening bladder cancer, Dr. Rosenberg says. But immunotherapy still doesnt work in enough patients. We have to find better ways to improve response rates and survival. Even if checkpoint inhibitors and antibody-drug conjugates dont represent a cure for bladder cancer, anything that could help people live longer or delay progression of the disease in some cases, allowing them to avoid bladder removal or chemotherapy after surgery will improve their quality of life.
- New drug types are being used to treat bladder cancer, especially metastatic bladder cancer.
- Antibody-drug conjugates carry anti-cancer drugs directly to tumor cells.
- Checkpoint inhibitors enable the immune system to attack cancer.
- These drugs, especially when combined, show promise for treating bladder cancer at various stages.
Survival For All Stages Of Bladder Cancer
Generally, for people diagnosed with bladder cancer in England:
- around 75 out of every 100 survive their cancer for 1 year or more after diagnosis
- almost 55 out of every 100 survive their cancer for 5 years or more after they are diagnosed
- around 45 out of every 100 survive their cancer for 10 years or more after diagnosis
Cancer survival by stage at diagnosis for England, 2019Office for National Statistics
These statistics are for net survival. Net survival estimates the number of people who survive their cancer rather than calculating the number of people diagnosed with cancer who are still alive. In other words, it is the survival of cancer patients after taking into account that some people would have died from other causes if they had not had cancer.
Recommended Reading: Bladder Control Products By Mail
Subtleties And Future Questions
Several factors have to be carefully considered in interpreting the trial results, explained Dr. Apolo.
A major one is that the study did not directly compare survival between people who got avelumab immediately versus when their cancer progressed. Only about half of the participants who initially received supportive care alone went on to receive immunotherapy after their cancer got worse. There could be many reasons for this, including lack of access to these drugs in different countries, Dr. Apolo said.
But it also might be that, for some people, the cancer was progressing too rapidly, she added. When these tumors start growing, they start growing very quickly. So if you wait to start at the time of progression, maybe its too late, added Dr. Apolo.
Not all patients will be caught by the second-line safety net, agreed Dr. Plimack.
So, for now, said Dr. Balar, the takeaway message from the JAVELIN study is after chemotherapy, dont wait to give immunotherapy.
But more and more, studies are looking at whether some patients should receive immunotherapy as first-line treatment, he continued. Immunotherapy is one of the most important advances weve made in the last 30 years, Dr. Balar said.
The JAVELIN results cant provide any insight into which patients benefit from first-line treatment with a platinum-based chemotherapy, he added. This trial wasnt designed to ask: Is chemotherapy necessarily the best choice for every patient? he explained.