What Kind Of Doctor Is Best
Start with your primary care doctor. Your doctor may recommend a specialist with certification in Female Pelvic Medicine and Reproductive Surgery , such as a gynecologist, a urologist or a urogynecologist, also known as a urogyn. A urogynecologist is a medical doctor who has completed a residency in obstetrics and gynecology or urology. He or she has received additional training and experience in evaluating and treating conditions that affect the female pelvic organs, as well as the muscles and connective tissue that support them. Common problems treated by a urogynecologist include urinary incontinence or leakage, pelvic organ prolapse and overactive bladder.
What Are The Side Effects Of Uterine Prolapse Surgery
Bladder or bowel injuries occur in about 2 out of 100 women who have sacrocolpopexy or sacrohysteropexy surgery. Wound infections are possible too. Like in all forms of abdominal surgery, scar tissue may lead to adhesions that cause pain or digestive problems. The use of synthetic meshes is associated with certain risks.
Potential Complications Related To Synthetic Non
Unfortunately there is no such thing as a perfect mesh. The perfect mesh would reinforce the repair, not be associated with infection, would reduce the rate of prolapse recurrence and not be associated with any shrinkage that could result in vaginal narrowing, shortening or pain. Such a mesh is unfortunately yet to be designed.
Potential complications related to use of permanent synthetic mesh in prolapse repair include:
- This may cause no symptoms
- Mesh exposure can cause symptoms of
- Vaginal discharge or bleeding
- Pain related to intercourse for either partner
Read Also: How To Remove Bladder Cancer
A Second Medical Opinion May Help
If a doctor recommends surgery for the treatment of a prolapse, it can be a good idea to find out about the other treatment options particularly if they recommend a hysterectomy. Its important to understand why they have suggested removing the womb: Is it because of the prolapse, or are there other reasons? What advantages and disadvantages would a hysterectomy have? And how important is it to you that you keep your womb?
If you are feeling unsure, it’s a good idea to seek a second medical opinion in other words, to talk with a doctor in a different practice or hospital.
Our decision aid may be helpful, too. It provides a brief summary of the main pros and cons of the different treatment options.
What Is A Vaginal Mesh Suspension
This mesh operation is called a sacral colpopexy and is most often performed through an abdominal incision. However, recent innovations now allow this procedure to be performed laparoscopically by experienced laparoscopic surgeons. In some centers the addition of the Da Vinci Robot has assited with laparoscopic support surgery. As with other laparoscopic procedures, the hospital stay is shorter and the recovery faster.
Read Also: What Can Help With Bladder Leakage
What Pelvic Floor Surgeries Use Mesh
It is important to note that the FDA has only stopped the sale and distribution of devices containing mesh used for the transvaginal repair of pelvic organ prolapse.
Two common pelvic floor surgeries that use mesh and are not affected by the FDA announcement are as follows:
- Transabdominal mesh to treat pelvic organ prolapse: This minimally invasive surgery is done by making a small incision in the abdomen or laparoscopically and inserting the mesh to support organs. This technique has existed for more than 30 years and is well studied and safe. Women should not be afraid of this, Dr. Harmanli says.
- Midurethral sling procedure: This surgery is the most common one used to treat stress urinary incontinence. A surgeon makes three small incisions and places a narrow strip of synthetic mesh under the urethra to lift and support it along with the neck of the bladder. This is the safest and least complicated procedure a woman can have for urinary incontinence, Dr. Harmanli says. There are approximately 20 years of high-quality data supporting this surgery. The risks are very minimal, and when there is a complication, it can be corrected with another surgery, but that is hardly ever needed.
Treatment That Offers Strength And Security
The urogynecology experts at Main Line Health offer prolapsed bladder surgery as part of female pelvic reconstructive surgery to treat pelvic floor conditions. A urogynecologist is an expert in gynecology with added training in neuro-urologic testing and pelvic reconstructive surgery.
In some cases, a special mesh material may be put in place during surgery to support your bladder even more. Talk to your doctor about the benefits of using mesh for support and whether its right for your situation.
Laparoscopic surgery requires less downtime than traditional surgery. Youll have less pain and a faster recovery. After prolapsed bladder surgery, you can expect to return to normal activities in about six weeks.
To schedule an appointment with a specialist at Main Line Health, or .
Recommended Reading: How To Diagnose Bladder Infection
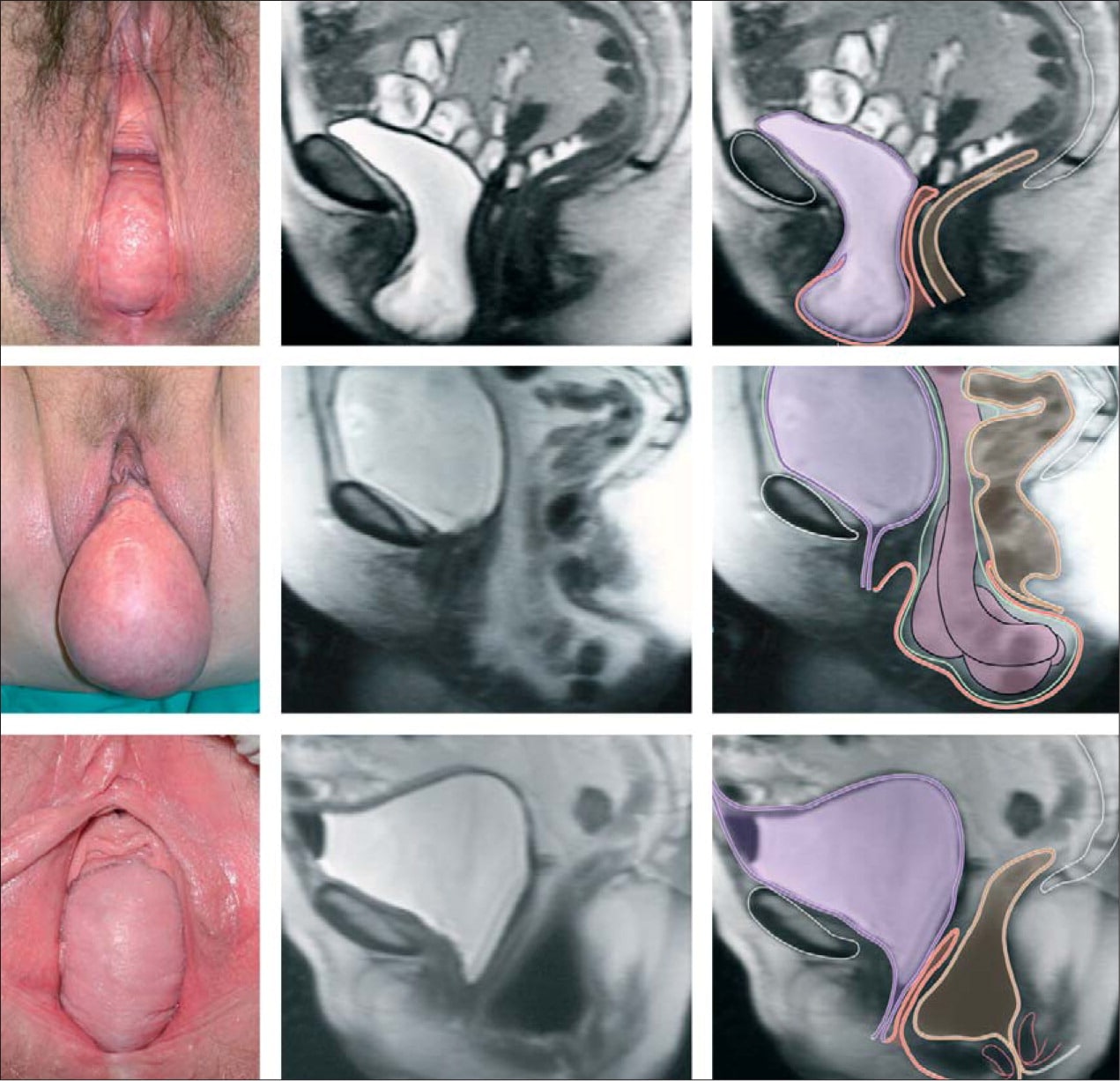
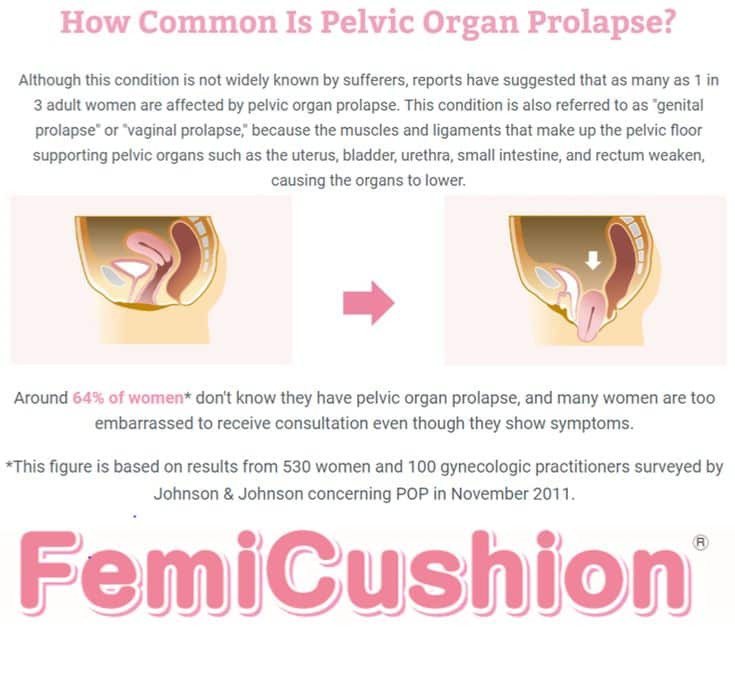
What To Do If You Have Been Diagnosed With Prolapse
If you have been diagnosed with or think you may have a prolapse, you can find out about the different types of treatments that may be offered to you here, as well as ways of helping yourself. This information should be used in conjunction with support from your GP or health professional to help you find the right course of treatment best suited to your individual needs enabling you to manage your condition and improve your quality of life.
Please use this information carefully and always speak to your GP or health professional, they can explain what is causing your problem and how the different treatments may help you. They will also talk to you about any side effects, these are extra problems that can be caused by the treatment.
Together, you can decide which treatment is the most suitable.
You May Like: Uti Bladder Infection Kidney Infection
Advantages Of A Minimally Invasive Laparoscopic Approach
While still considered major surgery, the minimally invasive laparoscopic approach offers several advantages over a vaginal approach or traditional open abdominal surgery, including:
- Shorter hospital stays
- Less blood loss because the surgeon works through small incisions with limited tissue disruption
- Faster recovery and return to normal activities
- Fewer complications than open or transvaginal surgery
- The surgeon has a better view of the pelvic structures, resulting in less risk of damaging surrounding organs
- Better access to the pelvic organs from multiple angles
- Lower risk of prolapse recurrence than with an open abdominal or transvaginal approach
Don’t Miss: Chemotherapy For Bladder Cancer Survival Rate
Finding The Right Doctor For Pelvic Prolapse Surgery
If you plan to have pelvic prolapse surgery, youll want a highly qualified experienced doctor to perform the procedure. While obstetrician-gynecologists commonly perform pelvic prolapse surgeries, female pelvic medicine and reconstructive surgeons specialize in these types of surgeries. How do you find the best surgeon for you? Here are important factors to keep in mind.
Read Also: Where Is The Bladder Located
Make An Appointment With A Urogynecologist
Call 801-2132995 to request an appointment with one of our urogynecologists to discuss your prolapse and find out if prolapse surgery is the right option for you. Physicians can also refer patients to a urogynecologist using our online referral form, or by contacting our office.
You do not need a referral to see a urogynecology specialist at U of U Health, but some insurance plans require that you get a referral from your primary care provider to see a specialist. Contact your insurance carrier with questions.
Don’t Miss: Is There A Test For Bladder Cancer
What Does A Laparoscopic Approach To Correcting Pelvic Organ Prolapse Involve
In a laparoscopy, the surgeon inserts very small, specialized instruments through tiny abdominal incisions to examine and operate on your pelvic organs. During surgery, your doctor may use your own body tissue or synthetic mesh to suspend the fallen organ at the correct height or to build pelvic floor support.
Determine Your Insurance Benefit
Your insurance coverage is a practical matter. To receive the most insurance benefits and pay the least out-of-pocket for your surgery, you need to choose a doctor that participates in your plan.
But keep in mind, just because a doctor participates in your insurance plan doesnt mean he or she is a high-quality doctor. You still need to consider the doctors experience and expertise.
Also Check: Can A Bladder Infection Cause Back Pain
What Are My Other Surgical Options
Ask your physician if he or she is aware of new, minimally invasive procedures.
Women need to be their own best advocate, which is why getting a second opinion is always good practice. Since there are different surgical options for treating pelvic organ prolapse, getting a second opinion is a way you can ask questions about how the surgery will be performed, the recovery time, and possible complications.
Pros & Cons Of Pelvic Organ Prolapse Surgery
Let us help you by stating all the Pros & Cons you can expect from a Prolapse Surgery.
A. Pros Improved Position of Pelvic Organssurgeries are expected to fix the position of displaced organs .
No More Pessary these devices are usually suggested by doctors until a patient decides to have surgery. If you had trouble wearing these devices, surgery will free you from the hassle of using them.
Favorable studies on surgery success and quality of life this ones double-sided. Although some prolapse surgeries are successful according to studies and show an improved QoL among patients, there is also a high failure rate and lack of data available according to other studies. This makes it difficult to look at prolapse surgeries objectively.
B. Cons Risks, Complications, and Recurrence prolapse surgeries arent guaranteed cures. Just like other operations, theres a chance you could develop mild to severe complications or recurrence depending on the type of surgery, your lifestyle post-surgery, and the effectiveness of the surgery itself.
Long Recovery Period women are expected to rest and avoid strenuous activities anywhere from 6 weeks to 2.5 months. If youre a mother, you might need to arrange how the chores, children, and your job will be taken care of while recovering.
High Cost prolapse surgeries usually cost around $5,000 to $9,000 depending on the type, medical provider, and additional medications needed.
Outcomes of POP Surgery
Nerve damage
You May Like: Bladder Cancer Chemo Treatment Side Effects
What Types Of Bladder Prolapse Repair Surgery Are Available
Bladder prolapse surgery is often called a bladder lift as it involves the movement of the bladder back up into place where it is then stitched. Many of these surgeries can be performed alongside other prolapse repair surgeries, to resolve all prolapses during one operation.
These surgeries do have relatively high initial success rates, however, it is not uncommon for symptoms to return over time, meaning further surgery is required.
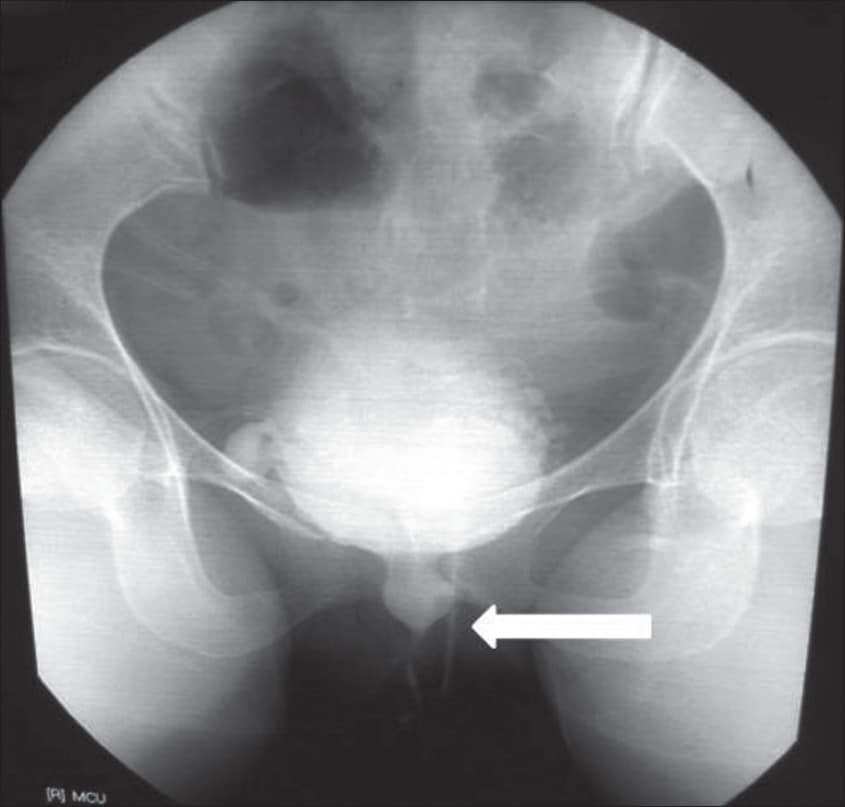
Prolapsed Bladder Symptoms In Men:
- Male urinary dysfunction: This condition can involve leaking urine after peeing, frequent urination and other bladder and bowel issues.
- Erectile Dysfunction : ED is when men cant get or maintain an erection during sex. Sometimes pelvic muscle tension or pain can contribute to this issue.
- Prostatitis: Pelvic floor dysfunction and prolapse symptoms closely resemble prostatitis, which is an infection or inflammation of the prostate. Prostatitis can have many causes including bacteria, sexually transmitted infections or trauma to the nervous system.
- A sense that something is falling out
- Trouble emptying your bowel or bladder completely
- Urine leakage, frequency, chronic urinary tract infections, difficulty urinating
- Difficult bowel movements or trapping of stool
Also Check: Malignant Neoplasm Of Lateral Wall Of Urinary Bladder
Side Effects Of Surgery
Your doctor should have an in-depth discussion with you about the risks and benefits of the 4 different types of surgery, including mesh surgery, before you decide together whether one of them could be an option.
Doctors must also keep detailed records about the type of surgery they do, including any complications you get after you have had your surgery.
You should be given a copy of this record.
Possible side effects of all 4 types of surgery, including mesh surgery, include:
- bleeding, which may require a blood transfusion
- damage to the surrounding organs, such as your bladder or bowel
- an infection â you may be given antibiotics to take during and after surgery to reduce the risk
- changes to your sex life, such as discomfort during intercourse â but this should improve over time
- vaginal discharge and bleeding
- experiencing more prolapse symptoms, which may require further surgery
- a blood clot forming in 1 of your veins, such as in your leg â you may be given medicine to help reduce this risk after surgery
If you have any of the following symptoms after your surgery, let your surgeon or a GP know as soon as possible:
- a high temperature
When Did Mesh Start Appearing In Pelvic Floor Surgery
Polypropylene mesh has been used for abdominal hernias since the 1950s. Historically, pelvic organ prolapse was repaired with native tissue, or attaching the prolapsed organ to a surrounding ligament or muscle with stitches. Although this is still a good option for many women, some women dont have enoughor strong enoughnative tissue, Dr. Rickey explains. Also, this technique is not always effective long-term, Dr. Harmanli notes.
Meanwhile, the FDA approved the first pelvic mesh for stress urinary incontinence in 1996. In 2002, the first mesh for transvaginal repair of pelvic organ prolapse was approved. It was around that time when manufacturers began marketing kits that included surgical tools and mesh for transvaginal prolapse procedures, the first of which received FDA clearance in 2002.
Also Check: What Do They Give You For Bladder Infection
What Are Other Options For Pelvic Floor Disorder Treatment
But when such methods dont work for women, surgery may be helpful. Until a better product is designed that can be used transvaginally for repair of pelvic organ prolapse, Dr. Harmanli says he will continue to perform the procedure through the abdomen for women with severe prolapse. For cases that are moderate or for women where we cant easily go through the abdomen, we will offer transvaginal repair using native tissue, he explains.
What Else Can Help Prevent Leaking During Sex
Another way to prevent leaking during sex is to keep your bladder reasonably empty during intercourse. Try to avoid drinking fluids for an hour or so before you expect to have intercourse. This will keep the bladder from filling up too quickly once you get into bed. If you empty your bladder just before you begin lovemaking, leaking is much less likely.
Don’t Miss: Best Antibiotic To Treat Bladder Infection
Bladder Pain After Prolapse Surgery
You may feel cramping or pressure in your bladder area after your surgery. It generally settles after a few days, but sometimes it can take up to a few weeks to dissipate.
If you have an abdominal incision, you may also experience pain around the incision as it heals. You can take over-the-counter pain medications to ease the pain.
Free Pelvic Floor Educational Series
Dr. Sarah Duvall, PT, DPT, CPT and the CES Team have helped thousands of women create the strength and stability needed to overcome common and not-so-common pelvic floor issues.
Join us today for this 4-part Pelvic Floor Video Series, absolutely free.
We dont spam or give your information to any third parties. View our Terms of Use and Privacy Policy.
You May Like: How To Prevent Bladder Infections In Cats
What Are Grafts To Repair Prolapse
Grafts are a foreign material used at the time of prolapse surgery to reinforce the repair and a womans own natural tissues in an effort to try and reduce the rate of prolapse recurring.
Prolapse recurrence rates are higher when the prolapse:
- Is a recurrent prolapse
- Is associated with persistence of risk factors for prolapse such as obesity, chronic coughing, constipation and heavy lifting
Grafts can be made of a range of different material such as:
- Biological grafts which are derived from humans or animals
- Most biological grafts are reabsorbed slowly over 6 to 9 months during which time it is hoped that the womans own body produces new support tissue.
Degree Of Bother By Symptoms Is A Key Factor
In older patients, whether and how to treat POP depends on their functional status, the degree to which they are bothered or inconvenienced by the condition, and their personal preference.
If an elderly woman has anatomic POP but lacks bothersome symptoms, the condition rarely requires treatment. Conversely, POP symptoms may cause depression and poor self-image and impair participation in social activities. Associated bladder, bowel or sexual symptoms can also take their toll. And quality of life may be impacted regardless of the stage of prolapse. Vaginal bulge causing discomfort and/or bleeding, difficulty voiding and/or defecating, recurrent urinary tract infections and POP-associated low back pain are all symptoms that may warrant treatment.
Recommended Reading: How Long Is Bladder Removal Surgery
Does Incontinence Make You Less Attractive
Incontinence can undeniably complicate life in an unpleasant way. Many women modify what they wear and how they live as a result. Some tell us they feel less feminine and less independent. However, as we hope readers will learn from this website, there are now many ways to prevent incontinence. The social and physical isolation that incontinence sometimes brings is unnecessary.