Degree Of Bother By Symptoms Is A Key Factor
In older patients, whether and how to treat POP depends on their functional status, the degree to which they are bothered or inconvenienced by the condition, and their personal preference.
If an elderly woman has anatomic POP but lacks bothersome symptoms, the condition rarely requires treatment. Conversely, POP symptoms may cause depression and poor self-image and impair participation in social activities. Associated bladder, bowel or sexual symptoms can also take their toll. And quality of life may be impacted regardless of the stage of prolapse. Vaginal bulge causing discomfort and/or bleeding, difficulty voiding and/or defecating, recurrent urinary tract infections and POP-associated low back pain are all symptoms that may warrant treatment.
How Do I Prepare For My Vaginal Prolapse Surgery
You are an important member of your own healthcare team. The steps you take before surgery can improve your comfort and outcome.
You can prepare for vaginal prolapse surgery by:
-
Answering all questions about your medical history, , and medications. This includes prescriptions, over-the-counter drugs, herbal treatments, and vitamins. It is a good idea to carry a current list of your medical conditions, medications, and allergies at all times.
-
Getting preoperative testing as directed. Testing will vary depending on your age, health, and specific procedure. Preoperative testing may include a , EKG , blood tests, and other tests as needed.
-
If you are overweight, talk to your doctor about losing weight before surgery through a healthy diet and exercise plan.
-
Losing excess weight before the surgery through a healthy diet and exercise plan
-
Not eating or drinking before surgery as directed. Your surgery may be cancelled if you eat or drink too close to the start of surgery because you can choke on stomach contents during anesthesia.
-
Stopping smoking as soon as possible. Even quitting for just a few days can be beneficial and help the healing process.
-
Taking or stopping medications exactly as directed. This may include not taking aspirin, ibuprofen , and blood thinners.
Questions to ask your doctor
It is also a good idea to bring a list of questions to your appointments. Questions can include:
Addition Information About Vaginal Surgery When A Synthetic Or Biologic Graft Is Used
In Australia, in January 2018 the TGA withdrew approval for the used of synthetic and biologic mesh for trans-vaginal prolapse repair. The TGA continues to approve synthetic and biological mesh for prolapse when placed using laparoscopy, robot assisted and through an abdominal incision.
In the USA, the Food and Drug Administration has issued the following safety communication regarding the use of mesh.
The FDA wants to inform you about the complications that can occur when surgical mesh is used to treat Pelvic Organ Prolapse and Stress Urinary Incontinence , and provide you with questions to ask your surgeon before having these procedures. This is part of our commitment to keep healthcare professionals and the public informed about the medical products we regulate.
Background
Pelvic organ prolapse can cause pain or problems with bowel and bladder functions or interfere with sexual activity.
Stress urinary incontinence is a type of incontinence caused by leakage of urine during moments of physical stress.
Talking to your doctor
Recommended Reading: Can T Get Rid Of Bladder Infection
When Can I Go Home After Pelvic Organ Prolapse Surgery
Youll usually need to stay in hospital overnight or for a few days. Most women can go home once their bladder is emptying well.
In rare cases, you may need a catheter for a week or so. Youll still be able to go home, but youll need to come back in a week or two to have the catheter removed.
You wont be able to drive until your doctor agrees, so youll need someone to take you home from hospital.
Any Positive Prolapse Surgery Stories Out There
Jeen44
Hello,
Just wondering if anyone happens to read this who has a positive story about long term recovery from prolapse surgery? There are a lot of scary stories about surgery but I would love to hear from any one who is happy with their surgery and if possible what type of prolapses/procedures they had. I’m planning to have surgery soon and just want to be 100% sure I choose the right procedure. Ive researched for ages and decided to spend the money and go private but it has been like trying to make a decision in the dark- lots of horror stories, conflicting advice from specialists and I dont know of anyone who has had the surgery so I can ask them.
Thank you, any info appreciated!
0 likes, 81 replies
You May Like: Bleeding After Bladder Tumor Removal
Can Kegel Exercises Prevent Leaking During Sex
Kegel exercises can certainly help. Women who learn to do Kegels correctly and do them regularly have less leaking during intercourse. A recent study from Norway found that women who were taught by a physical therapist the correct way of performing Kegels were more likely to have more satisfying sex than a group of women who were not properly taught these exercises. These women had fewer problems with their sex life and less discomfort with intercourse. We encourage you to do Kegel exercises on a regular basis.
Multiple Benefits From A Multidisciplinary Clinic
In our multidisciplinary pelvic health clinic, we screen patients with urinary complaints, symptomatic prolapse and defecatory dysfunction, and provide a combined consultation and evaluation. The ultimate benefit is a comprehensive, patient-centered approach and single, coordinated surgery. In our experience, combined procedures can be offered to patients with the advantages of a single operation and concurrent recovery period without increasing complications or inferior outcomes.
Read Also: Intravesical Chemotherapy For Bladder Cancer
The Pelvic Pro Support Belt For Prolapse Treatment
If you wish to opt out of surgery and would prefer a more natural prolapse treatment option, women from all over the world are finding relief with our Pelvic Pro prolapse support belt. This is a comfortable brace that can be worn under your clothes and stay hidden from anyone noticing. Give our pelvic belt a try before choosing surgery and join other women in finding relief today!
Recovery Time For Bladder Prolapse Surgery
Depending on the type of surgery, you might stay in the hospital for 1 to 3 nights.
Its important to rest for a few weeks after the surgery to allow the area to heal. You will likely have a follow-up appointment with your surgeon a few weeks after the surgery to confirm that its healing well. You may also have additional follow-ups.
You May Like: Different Types Of Bladder Cancer
Should You Have Surgery
If your symptoms are making your life difficult, surgery may be the answer. You need to think about a few things:
Your age. If youâre young, keep in mind that bladder prolapse can happen again. Even if you have surgery now, you may end up needing another operation down the road. If youâre older, any other health issues you have may affect your decision.
Your plans about having children. If you want more children, itâs best to hold off on surgery until you decide your family is complete.
Your general health. Surgery has some risks, such as infection, blood clots, or problems with the anesthetic. If you have a heart condition, diabetes, or breathing difficulties, any of these things could make an operation riskier. So could smoking or obesity.
Also, talk with your doctor about the chances that surgery could cause new problems. You might develop urinary incontinence — urine leaking out without your control. Sex might become uncomfortable, and you might feel pain in your pelvis.
Bladder Prolapse Surgery Success Rate
The success of prolapse surgery depends on many different factors, including:
- how bad your prolapse is,
- what parts of your pelvic floor is affected,
- what type of surgery you get, and
- lifestyle or genetic factors that could increase the risk of another prolapse in the future.
Studies show that about 80 percent of prolapse surgeries are still successful after 10 years. About 10 to 20 percent of women will have some movement or bulging again, but its usually not enough to need another surgery. Only about two to three percent of women will need a repeat prolapse surgery.
Recommended Reading: Fibroid Pressing On Bladder Treatment
Immediately After Surgery For Rectal Prolapse
- Hospital staff will observe and note your temperature, pulse, breathing and blood pressure.
- You will have an intravenous fluid line in your arm to replace fluids in your body.
- You will receive pain-relieving medications. Tell your nurse if you need more pain relief.
- You may have a catheter to drain off urine for the next day or so, or until you can empty your bladder by yourself.
- If you have a vaginal pack, this will be taken out later the same day or the day after surgery.
- You may be in hospital for three to six days following surgery.
- You will need to make follow-up appointments with your doctor.
When Should I Contact A Doctor
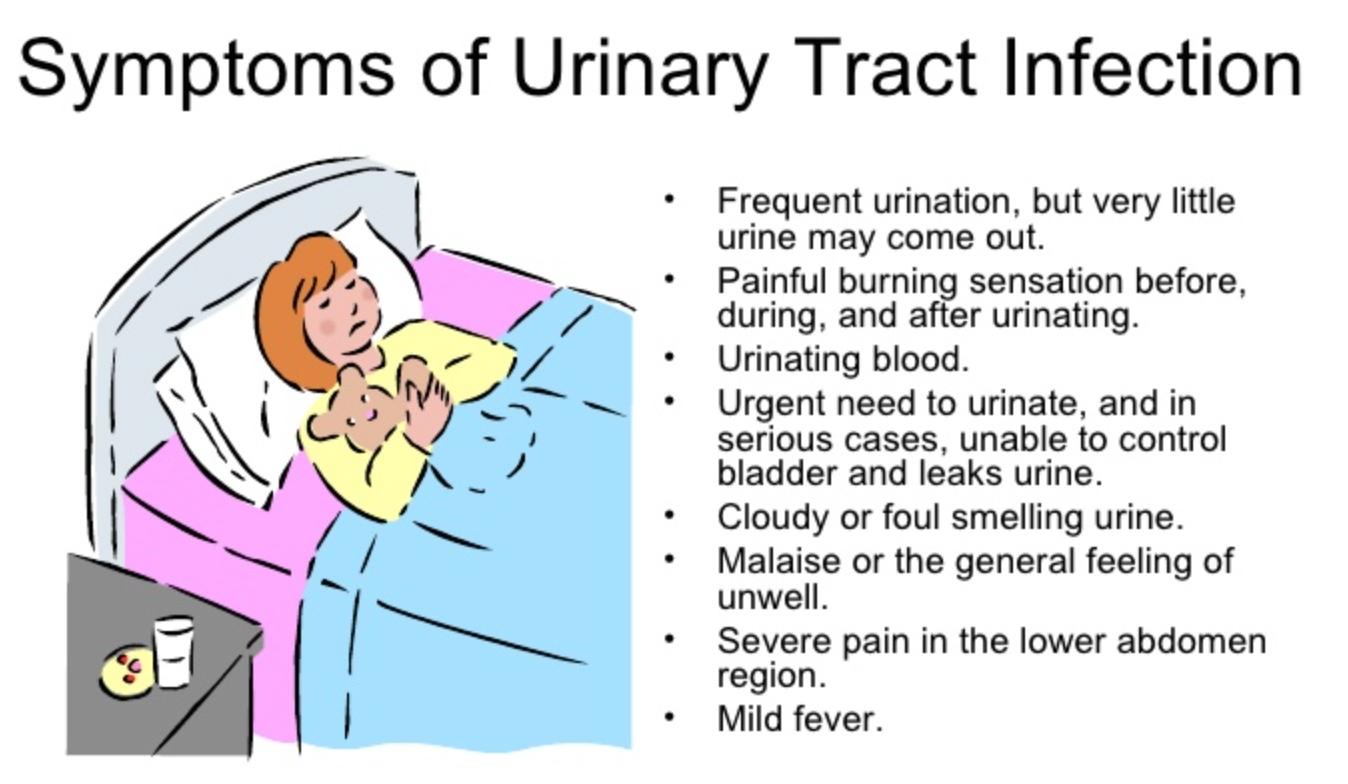
- If you have any concern at all about any condition with your body
- If you have lower back pain or increased pelvic pressure that interferes with your daily activities
- If you have irregular vaginal spotting or bleeding
- If you experience frequent urinary incontinence, urinary tract infections, difficulty urinating, frequent urination or any of the symptoms listed here that interfere with your daily routine
- If sexual intercourse is painful or difficult
You May Like: Bladder Frequent Urination At Night
What To Do If You Have Been Diagnosed With Prolapse
If you have been diagnosed with or think you may have a prolapse, you can find out about the different types of treatments that may be offered to you here, as well as ways of helping yourself. This information should be used in conjunction with support from your GP or health professional to help you find the right course of treatment best suited to your individual needs enabling you to manage your condition and improve your quality of life.
Please use this information carefully and always speak to your GP or health professional, they can explain what is causing your problem and how the different treatments may help you. They will also talk to you about any side effects, these are extra problems that can be caused by the treatment.
Together, you can decide which treatment is the most suitable.
What Is The Recovery Time For Pelvic Reconstructive Surgery How Painful Is Prolapse Surgery What Happens If Prolapse Is Left Untreated
Pelvic floor dysfunction symptoms typically stay or become worse if theyâre not treated. Instead of living with pain and discomfort, you can often improve your everyday life after a visit with your provider. The most common type of pelvic reconstructive surgery is that performed to correct pelvic organ prolapse.
Types of prolapse:
There are two main types of prolapse surgery:
- Transabdominal performed through the abdomen, usually laparoscopic or robotic via small incisions.
Both approaches are considered minimally invasive, have good success rates, and the approach is dependent on the preference of the patient as well as the surgeon. It should be a joint decision.
Avoid constipation by increasing the fiber content in your diet, avoid taking pain medications as much as you can, and use stool softeners. Straining during bowel movements can place undue pressure on your reconstructive surgery before complete healing.
Dont Miss: Homeopathic Medicine For Bladder Weakness
Don’t Miss: Bladder Cancer In Dogs Treatment
What Is Pelvic Organ Prolapse Repair
Pelvic organ prolapse occurs when the pelvic organs push into the vaginal canal due to the weakening of pelvic muscles. These are repaired in several different ways, either conservatively, with non-surgical treatments or with surgery.
Women who experience urinary incontinence often have this procedure to treat symptoms caused by prolapse and stress incontinence, which is treated with a urethral sling.
The type of surgical procedure conducted depends on the amount of prolapse and the location. Specific procedures include:
Who Performs Vaginal Prolapse Surgery
The following specialists perform vaginal prolapse surgery:
-
Obstetrician-gynecologists specialize in womens health and pregnancy.
-
Urologists specialize in diseases and conditions of the urinary tract and the male reproductive organs.
-
Female pelvic medicine and reconstructive surgeons are urologists or gynecologists who have completed specialized training in womens pelvic floor disorders.
Also Check: Bladder Cancer Carcinoma In Situ
Bladder Pain After Prolapse Surgery
You may feel cramping or pressure in your bladder area after your surgery. It generally settles after a few days, but sometimes it can take up to a few weeks to dissipate.
If you have an abdominal incision, you may also experience pain around the incision as it heals. You can take over-the-counter pain medications to ease the pain.
What Are The Side Effects Of Uterine Prolapse Surgery
Bladder or bowel injuries occur in about 2 out of 100 women who have sacrocolpopexy or sacrohysteropexy surgery. Wound infections are possible too. Like in all forms of abdominal surgery, scar tissue may lead to adhesions that cause pain or digestive problems. The use of synthetic meshes is associated with certain risks.
You May Like: Does Baking Soda Help Overactive Bladder
What Is Pelvic Organ Prolapse Surgery
Perhaps youve had a pelvic organ prolapse, and non-surgical treatments arent helping? Or maybe your prolapse is more severe? If so, your surgeon may recommend, pelvic organ prolapse surgery.
This surgery involves lifting the pelvic organs, such as the bladder, bowel and uterus, and stitching the tissues around them to give you more support.
Also Check: Does Beer Help Bladder Infections
What Is Uterine Prolapse Surgery
Uterine prolapse surgery is a major surgery with serious risks and potential complications. You may have less invasive treatment options. Consider getting a second opinion about all of your treatment choices before having uterine prolapse surgery.
Types of uterine prolapse surgery
The types of uterine prolapse surgery include:
-
Ligament suspension lifts the uterus using a mesh material or stitches to attach the uterus or vaginal vault to a strong ligament in the pelvis to support them. This is called a sacrospinous ligament suspension or uterosacral ligament suspension. Sometimes your surgeon lifts the uterus by attaching it to a muscle. This is called an ileococcygeus suspension.
-
Uterine suspension lifts the uterus using a mesh material to attach the uterus to the pelvis. This is called a sacral colpohysteropexy. Another version of the surgery shortens stretched-out ligaments that support the uterus.
Other procedures that may be performed
Procedures can include:
Don’t Miss: How To Empty Bladder With Uti
Make An Appointment With A Urogynecologist
Call 801-2132995 to request an appointment with one of our urogynecologists to discuss your prolapse and find out if prolapse surgery is the right option for you. Physicians can also refer patients to a urogynecologist using our online referral form, or by contacting our office.
You do not need a referral to see a urogynecology specialist at U of U Health, but some insurance plans require that you get a referral from your primary care provider to see a specialist. Contact your insurance carrier with questions.
Prolapse Of The Uterus Bladder Bowel Or Rectum
HERS
The uterus sits between the bladder and the bowel, supporting them in their natural position. The bladder sits in front of the uterus directly above the pubic bone. If you trace with your finger from your navel straight down, the bladder sits slightly to the right just above the pubic bone. The bowel sits behind the uterus. The rectum is behind the bowel.
If the uterus prolapses, it may pull the bladder down from above the pubic bone, and cause it to bulge into the vaginal wall. When the bladder prolapses it is called a cystocele . A cystocele may cause discomfort, incomplete emptying of the bladder during urination, and unwanted leakage when you sneeze, cough, laugh, or move in any way that puts pressure on the bladder.
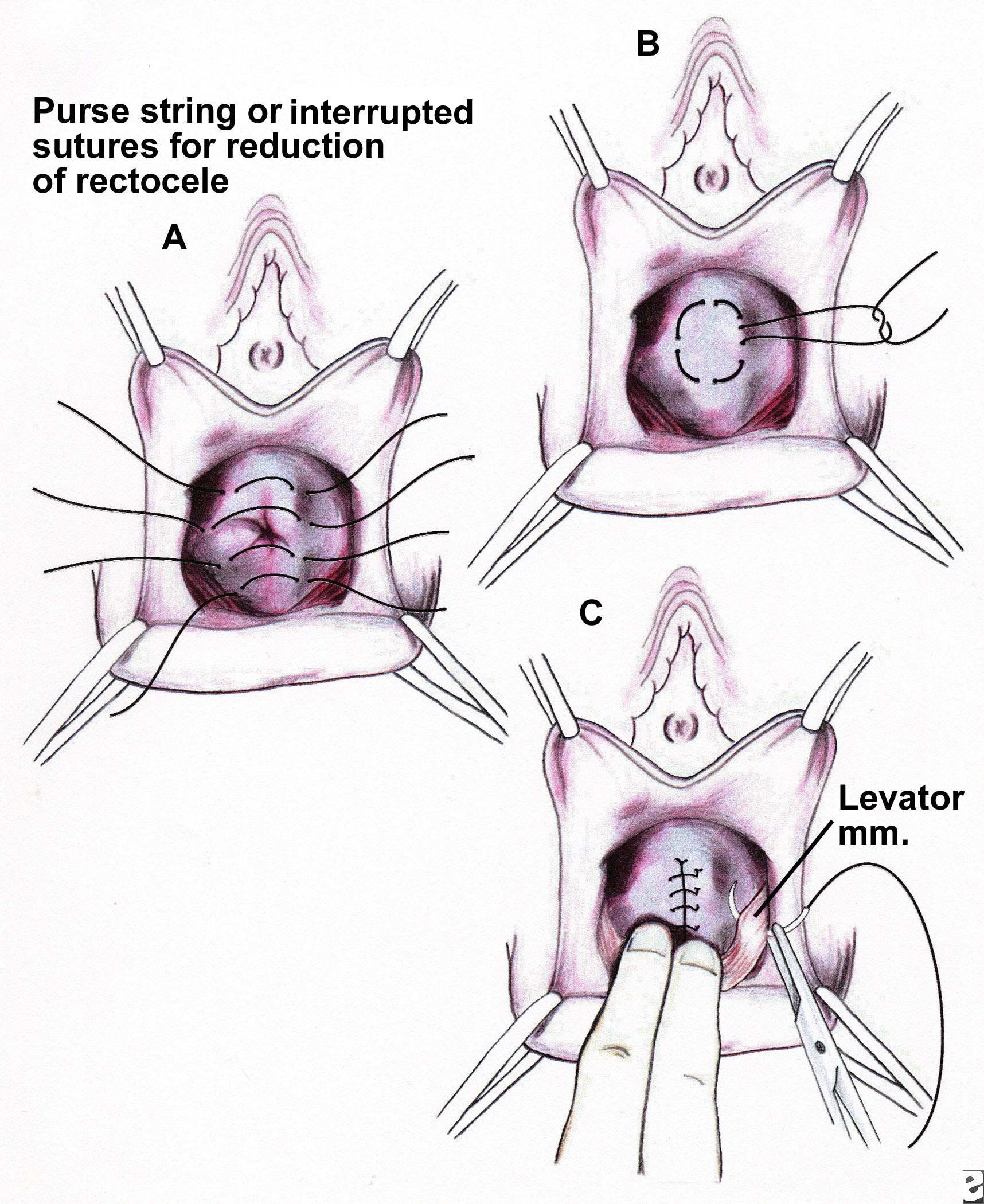
Cystocele and rectocele are benign conditions that can be managed mechanically with a device or with surgery. A hysterectomy is not needed for uterine prolapse, cystocele, or rectocele.
Cystocele and rectocele can occur without uterine prolapse, or they may accompany a second or third-degree prolapse of the uterus.
The bladder is supported by anatomical structures in addition to the structural support it gets from the uterus. The bowel, though, is more dependent on structural support from the uterus. Some women develop bladder prolapse whether or not they undergo hysterectomy, but rectocele is a consequence of hysterectomy for the majority of hysterectomized women. Rectocele is less common in women who have not undergone a hysterectomy.
Also Check: Bladder Cancer Chemotherapy Success Rate
Key Points For Preventing Prolapse After Hysterectomy
There are a number of ways you can reduce your risk of prolapse after hysterectomy.
To reduce your risk of prolapse:
- Speak with your surgeon to better understand the hysterectomy procedure youre undergoing and know your risks
- Manage your general health and lifestyle factors that can influence your risk of prolapse.
Read Also: What Does Overactive Bladder Feel Like
Vaginal Repair For Anterior And Posterior Vaginal Wall Prolapse
The success of prolapse surgery depends on many different factors, including:
- how bad your prolapse is,
- what parts of your pelvic floor is affected,
- what type of surgery you get, and
- lifestyle or genetic factors that could increase the risk of another prolapse in the future.
Studies show that about 80 percent of prolapse surgeries are still successful after 10 years. About 10 to 20 percent of women will have some movement or bulging again, but its usually not enough to need another surgery. Only about two to three percent of women will need a repeat prolapse surgery.
You May Like: What To Do If You Have A Bladder Infection