Radical Cystectomy For Non
There are several reasons to consider immediate RC for selected patientswith NMIBC:
- The staging accuracy for T1 tumours by TURB is low with 27-51% of patients beingupstaged to muscle-invasive tumour at RC .
- Some patients with NMIBC experience disease progression to muscle-invasive disease.
- Patients who experience disease progression to muscle-invasive stage have a worseprognosis than those who present with primary muscle-invasive disease.
The potential benefit of RC must be weighed against its risks, morbidity,and impact on quality of life and discussed with patients, in a shared decision-makingprocess. It is reasonable to propose immediate RC in those patients with NMIBC who are atvery high risk of disease progression .
Early RC is strongly recommended in patients with BCGunresponsive tumours and should be considered in BCG relapsing HG tumours as mentioned above. A delay in RC may lead to decreased disease-specificsurvival .
In patients in whom RC is performed before progression toMIBC, the 5-year DFS rate exceeds 80% .
When Is Chemotherapy Used
Systemic chemo can be used :
- Before surgery to try to shrink a tumor so that it’s easier to remove and to help lower the chance the cancer will come back. Giving chemo before surgery is called neoadjuvant therapy.
- After surgery . This is called adjuvant therapy. The goal of adjuvant therapy is to kill any cancer cells that may remain after other treatments. This can lower the chance that the cancer will come back later.
- In people getting radiation therapy, to help the radiation work better.
- As the main treatment for bladder cancers that have spread to distant parts of the body.
Working With Your Healthcare Provider
It’s important to know which medicines you’re taking. Write down the names of your medicines. Ask your healthcare team how they work and what side effects they might cause.
Talk with your healthcare providers about what side effects to watch for and when to call them. For instance, chemo can make it easier for you to get infections. Make sure you know what number to call with questions. Is there a different number for evenings and weekends?
It may be helpful to keep a diary of your side effects. Write down physical, thinking, and emotional changes. A written list will make it easier for you to remember your questions when you go to appointments. It will also make it easier for you to work with your healthcare team to make a plan to manage your side effects.
Online Medical Reviewer:Online Medical Reviewer:Online Medical Reviewer:Date Last Reviewed:
Recommended Reading: Does Alcohol Cause Bladder Infections
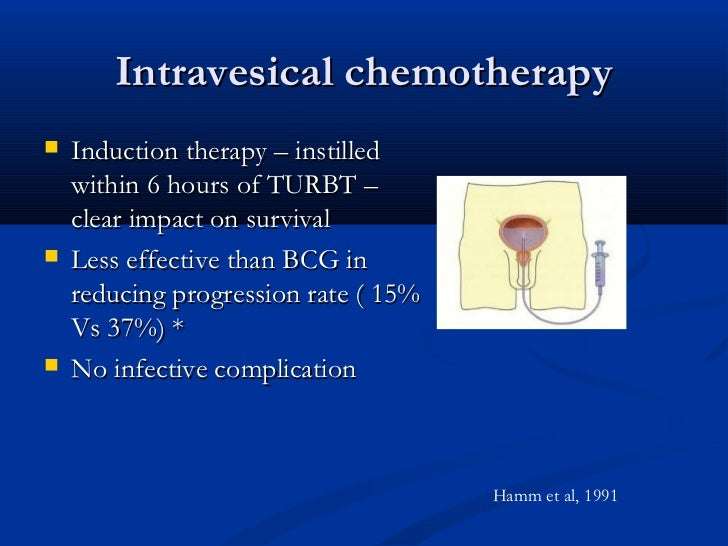
Use Of Intravesical Chemotherapy Based On Clinical Scenario
Immediate post-operative instillation
Transurethral resection of bladder tumor is the mainstay of both diagnosis and treatment of NMIBC, and provides both the stage and the basis of risk stratification. Despite visually complete resection, there is a high rate of recurrence in patients with NMIBC, possibly due to implantation of tumor cells after TURBT or residual but not visible disease. Sylvester et al. performed a comprehensive meta-analysis compiling clinical trials examining almost 1500 patients and found a reduction in recurrence rate from 48.4% to 36.7% in patients receiving immediate instillation of intravesical chemotherapy . MMC, doxorubicin, and epirubicin showed benefit however, epirubicin is not currently available in the United States. This benefit appears to be greatest in solitary, low-volume tumors. Intravesical gemcitabine does not have a role in this setting, as a phase 3 randomized controlled trial performed on over 350 patients did not show benefit as was seen for other agents, when compared to placebo .
Adjuvant instillation of intravesical chemotherapy
Physical Emotional And Social Effects Of Cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel feels during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after an advanced cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, report that they are more satisfied with treatment, and they may live longer.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Before treatment begins, talk with your doctor about the goals of each treatment in the treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative care options.
Also Check: Bladder Infection And Back Pain
Strategy Of The Procedure
The goal of TURB in TaT1 BC is to make the correct diagnosis and completelyremove all visible lesions. It is a crucial procedure in the management of BC. Transurethralresection of the bladder should be performed systematically in individual steps .
The operative steps necessary to achieve a successful TURB includeidentifying the factors required to assign disease risk , clinical stage , adequacy of the resection , and presence of complications . To measure the size of thelargest tumour, one can use the end of cutting loop, which is approximately 1 cm wide as areference. The characteristics of the tumour are described as sessile, nodular, papillary orflat.
Treatment Failure After Intravesical Bcg Immunotherapy
Several categories of BCG failures, broadly defined as any high-gradedisease occurring during or after BCG therapy, have been proposed .Non-muscle-invasive BC may not respond at all or may relapse after initialresponse . Some evidence suggests that patients with BCG relapse have betteroutcomes than BCG refractory patients .
To be able to specify the subgroup of patients where additional BCG isunlikely to provide benefit, the category of BCG unresponsive tumour was defined. FurtherBCG instillations in these patients are associated with an increased risk of progression . The category of BCG unresponsivetumours comprises BCG-refractory and some of BCG-relapsing tumours . The definition was developed in consultation with the FDA, inparticular to promote single-arm trials to provide primary evidence of effectiveness in thissetting .
Non-high-grade recurrence after BCG is not considered as BCG failure.
Table 7.2: Categories of high-grade recurrence during or after BCG
* Patients with low-grade recurrence during or after BCGtreatmentare not considered to be a BCG failure.
** Adequate BCG is defined as the completion of at least 5 of 6doses of an initial induction course plus at least 2 out of 6 doses of a second inductioncourse or 2 out of 3 doses of maintenance therapy.
Also Check: What Is The Treatment For Low Grade Bladder Cancer
Specificaspects Of Treatment Of Carcinoma In Situ
7.2.4.1.Treatment strategy
The detection of concurrent CIS increases the risk of recurrence andprogression of TaT1 tumours . Inthis case further treatment according to the criteria summarised in Sections 7.2.1, 7.2.2,7.3 and 7.4 is mandatory. Carcinoma in situ cannot becured by an endoscopic procedure alone. Histological diagnosis of CIS must be followed byfurther treatment, either intravesical BCG instillations or RC . Tumour-specificsurvival rates after immediate RC for CIS are excellent, but a large proportion of patientsmight be over-treated .
7.2.4.2.Cohort studies on intravesical BCGor chemotherapy
In retrospective evaluations of patients withCIS, a complete response rate of 48% was achieved with intravesical chemotherapy and72-93% with BCG . Up to 50% of complete responders might eventually show recurrence with a risk ofinvasion and/or extravesical recurrence .
7.2.4.3.Prospective randomised trials onintravesical BCG or chemotherapy
Unfortunately, there have been few randomisedtrials in patients with CIS only. A meta-analysis of clinical trials comparingintravesical BCG to intravesical chemotherapy in patients with CIS has shown asignificantly increased response rate after BCG and a reduction of 59% in the odds oftreatment failure with BCG .
7.2.4.4.Treatment of CIS in the prostaticurethra and upper urinary tract
7.2.4.5.Summary of evidence – treatment ofcarcinoma in situ
Study Population And Clinicopathologic Features
After obtaining Institutional Review Board approval, we identified 13 patients aged 18years with Ta, T1, or carcinoma in situ urothelial carcinoma of the bladder, who received salvage intravesical docetaxel after failing 1 or more courses of intravesical BCG.
Clinicopathologic features recorded included age at predocetaxel recurrence, sex, Charlson comorbidity index, smoking status, tumor stage at initial diagnosis and at predocetaxel recurrence, tumor grade at initial diagnosis and at predocetaxel recurrence, characteristics of prior BCG therapy , and time from last treatment to BCG failure. BCG failure was categorized as refractory, unresponsive, relapsing, or intolerant. With regard to docetaxel administration, we recorded initial response after docetaxel induction, utilization of maintenance docetaxel therapy, time to recurrence after docetaxel induction, tumor grade and stage at postdocetaxel recurrence, and clinical management of postdocetaxel recurrence. Docetaxel-related toxicity, categorized according to symptoms, was retrospectively assessed by using a prespecified data collection sheet. Delayed toxicity was considered in patients who presented with symptoms after 2weeks following completion of all 6 cycles of induction therapy.
Read Also: Can Candida Cause Bladder Infection
How Is Chemo Used To Treat Bladder Cancer
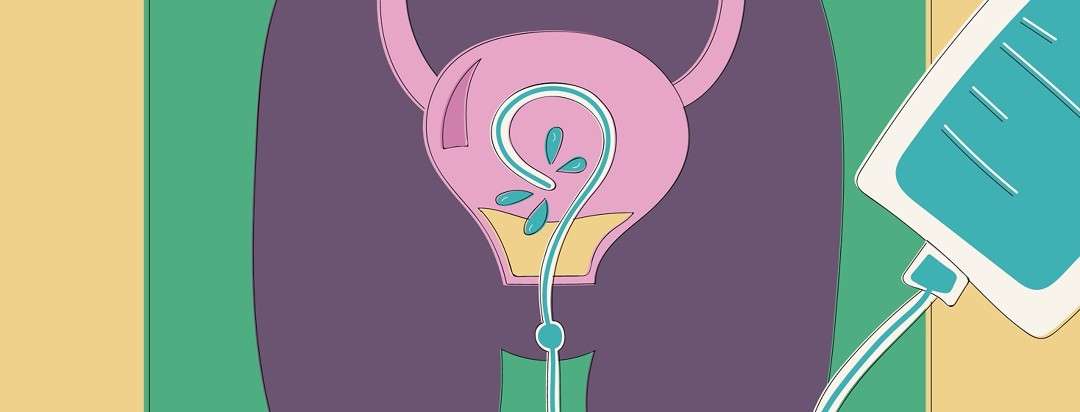
Intravesical chemotherapy is typically used to treat patients with early-stage bladder cancer.1,2 Bladder cancer cells generally start to grow in the urothelium, which is the thin layer of cells that line the inside of the bladder. In early-stage bladder cancer, the cancer cells are only located in the bladder lining and have not grown into the muscle of the bladder wall.
Because it is delivered directly into the bladder, intravesical chemotherapy treatment is only effective against cancer cells located in the bladder lining. This type of treatment does not work against cancer cells that have grown deep into the bladder wall muscle or against cancer cells that are growing outside of the bladder in other organs or tissues.
Prophylactic Intravesical Chemotherapy To Prevent Bladder Tumors After Nephroureterectomy For Primary Upper Urinary Tract Urothelial Carcinomas: A Systematic Review And Meta
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Rent for 48h to view
- Buy Cloud Access for unlimited viewing via different devices
- Synchronizing in the ReadCube Cloud
- Printing and saving restrictions apply
USD 8.50
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Don’t Miss: What Happens When A Bladder Infection Goes Untreated
Detection Of Residual Disease And Tumour Upstaging
The significant risk of residual tumour after initial TURB of TaT1 lesionshas been demonstrated .
A SR analysing data of 8,409 patients with Ta or T1 HG BCdemonstrated a 51% risk of justify persistence and an 8% risk of under-staging in T1tumours. The analysis also showed a high risk of residual disease in Ta tumours, but thisobservation was based only on a limited number of cases. Most of the residual lesions weredetected at the original tumour location .
Another meta-analysis of 3,556 patients with T1 tumoursshowed that the prevalence rate of residual tumours and upstaging to invasive disease afterTURB remained high in a subgroup with detrusor muscle in the resection specimen. In thesubgroup of 1,565 T1 tumours with detrusor muscle present, persistent tumour was found in58% and under-staging occurred in 11% of cases .
Before You Start Chemotherapy
You need to have blood tests to make sure its safe to start treatment. You have these either a few days before or on the day you start treatment. You have blood tests before each round or cycle of treatment.
Before each treatment you need to stop drinking fluids. This stops the urine from diluting the drug in your bladder and will help you hold the urine more easily. Your hospital will tell you when to stop drinking.
Recommended Reading: New Treatments For Neurogenic Bladder
Scoringmodels Using The Who 1973 Classification System
6.1.1.1.The 2006 European Organisation forResearch and Treatment of Cancer scoring model
To be able to predict both the short- and long-term risks of diseaserecurrence and progression in individual patients, the EORTC Genito-Urinary Cancer Grouppublished a scoring system and risk tables based on the WHO 1973 classification in 2006 . The scoring system is based on the six most significantclinical and pathological factors in patients mainly treated by intravesical chemotherapy:
- Number of tumours
- Concurrent CIS
- WHO 1973 tumour grade.
Using the 2006 EORTC scoring model, individual probabilities of recurrenceand progression at one and five years may be calculated.
6.1.1.2.The model for patients with TaG1/G2 tumours treated with chemotherapy
Patients with TaG1/G2 tumours receiving chemotherapy were stratified intothree risk groups for recurrence, taking into account the history of recurrences, history ofintravesical treatment, tumour grade , number of tumours and adjuvant chemotherapy.
6.1.1.3.Club Urologico Español deTratamiento Oncologico scoring model for BCG-treated patients
- gender
- associated CIS
- WHO 1973 tumour grade.
6.1.1.4.The 2016 EORTC scoring model forpatients treated with maintenance BCG
Intravesical Therapy For Bladder Cancer
With intravesical therapy, the doctor puts a liquid drug right into your bladder rather than giving it by mouth or injecting it into your blood. The drug is put in through a soft catheter that’s put into your bladder through your urethra. The drug stays in your bladder for up to 2 hours. This way, the drug can affect the cells lining the inside of your bladder without having major effects on other parts of your body.
Recommended Reading: Does Bladder Cancer Pain Come And Go
Treatment After A Turbt
Intravesical chemotherapy is commonly used after a patient with non-muscle-invasive bladder cancer has had a surgical procedure called transurethral resection of bladder tumor . During this procedure, the surgeon removes cancer cells from the lining of the bladder using a small, thin instrument inserted into the bladder through the urethra. After the procedure, intravesical chemotherapy may be used to help destroy any remaining cancer cells in the bladder lining and to help potentially reduce the chance of the cancer cells growing back . Some patients may only receive a single dose of intravesical chemotherapy, while others may need multiple doses.
Nonmuscle Invasive Bladder Cancer
High-grade or T1 disease:
-
For T1 tumors, TURBT alone is generally not adequate treatment use of intravesical bacillus Calmette-Guerin after TURBT is recommended
Intravesical adjuvant immunotherapy for nonmuscle-invasive bladder cancer :
-
BCG 81 mg or 50 mg in 50 mL sterile saline instilled into the bladder through a catheter and held for 2 h instilled weekly for 6 wk
-
Maintenance therapy: 81 mg intravesically given on days 1, 8, and 15 of months 3, 6, 12, 18, 24, and 36 after initiation
BCG-unresponsive nonmuscle-invasive bladder cancer:
- Pembrolizumab is indicated for treatment of BCG-unresponsive, high-risk NMIBC with carcinoma in situ with or without papillary tumors in patients who are ineligible for, or have elected not to undergo, cystectomy.
- Pembrolizumab 200 mg IV q3wk until disease progression or unacceptable toxicity, or up to 24 months in patients without disease progression
- Valrubicin is indicated for intravesical therapy of BCG-refractory CIS of the urinary bladder in patients for whom immediate cystectomy would be associated with unacceptable morbidity or mortality.
- Valrubicin 800 mg added to 55 mL sterile saline instilled into the bladder through a catheter and held for 2 h instilled weekly for 6 wk
Read Also: What Are The Survival Rates Of Bladder Cancer
When Is Intravesical Chemotherapy Used
Intravesical chemotherapy can be a viable treatment option for patients with early-stage cancer that has not invaded the bladder wall. Unlike traditional chemotherapy that delivers drugs throughout the entire body, this treatment only attacks cancer cells on the lining of the bladder. When appropriate, intravesical chemotherapy is given following minimally invasive transurethral resection surgery to remove small tumors. Patients with late-stage bladder cancers typically rely on a combination of surgery to remove larger amounts of tissue, radiation therapy and traditional chemotherapy.
Quality Assessment And Data Extraction
The quality of all included RCTs was assessed using the risk of bias tool recommended by the Cochrane Collaboration. It consists of the following domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias. The Newcastle-ottawa quality scale was used to assess the quality of retrospective studies. Two reviewers independently evaluated the quality of studies in these domains.
Data extraction was also executed by two reviewers independently. The following information was extracted: first author’s name, year of publication, study period, study design, sample size, clinical protocols, and number of patients who completed the study, age of participants, median follow-up, treatment schedule, and relevant data on outcomes. Disagreements were discussed and consensus was finally achieved.
Read Also: Bladder Exercises For Overactive Bladder
Chemotherapy For Bladder Cancer
Chemotherapy uses anticancer drugs to destroy cancer cells. It is sometimes used to treat bladder cancer. Your healthcare team will consider your personal needs to plan the drugs, doses and schedules of chemotherapy. You may also receive other treatments.
Chemotherapy is given for different reasons. You may have chemotherapy to:
- destroy cancer cells in the body
- shrink a tumour before other treatments such as surgery or radiation therapy
- destroy cancer cells left behind after surgery and reduce the risk that the cancer will come back
- make cancer cells more sensitive to radiation therapy
- relieve pain or control the symptoms of advanced bladder cancer
Chemotherapy for bladder cancer that has not grown into the muscle of the bladder wall is given as intravesical therapy, which means that the drugs are placed directly into the bladder. Chemotherapy may also be a systemic therapy given through a needle into a vein. This means that the drugs travel through the bloodstream to reach and destroy cancer cells all over the body, including those that may have broken away from the primary tumour in the bladder.