Treatment Options Under Clinical Evaluation For Patients With Any T Any N M1 Disease
Prognosis is poor in patients with stage IV disease and consideration of entry into a clinical trial is appropriate.
Other chemotherapy regimens appear to be active in the treatment of metastatic disease. Chemotherapy agents that have shown activity in metastatic bladder cancer include paclitaxel, docetaxel, ifosfamide, gallium nitrate, and pemetrexed.
Treatment Options For Recurrent Bladder Cancer
Treatment options for patients with recurrent bladder cancer include the following:
Palliative radiation therapy should be considered for patients with symptomatic tumors.
Clinical trials
Recurrent or progressive disease in distant sites or after definitive local therapy has an extremely poor prognosis, and clinical trials should be considered whenever possible.
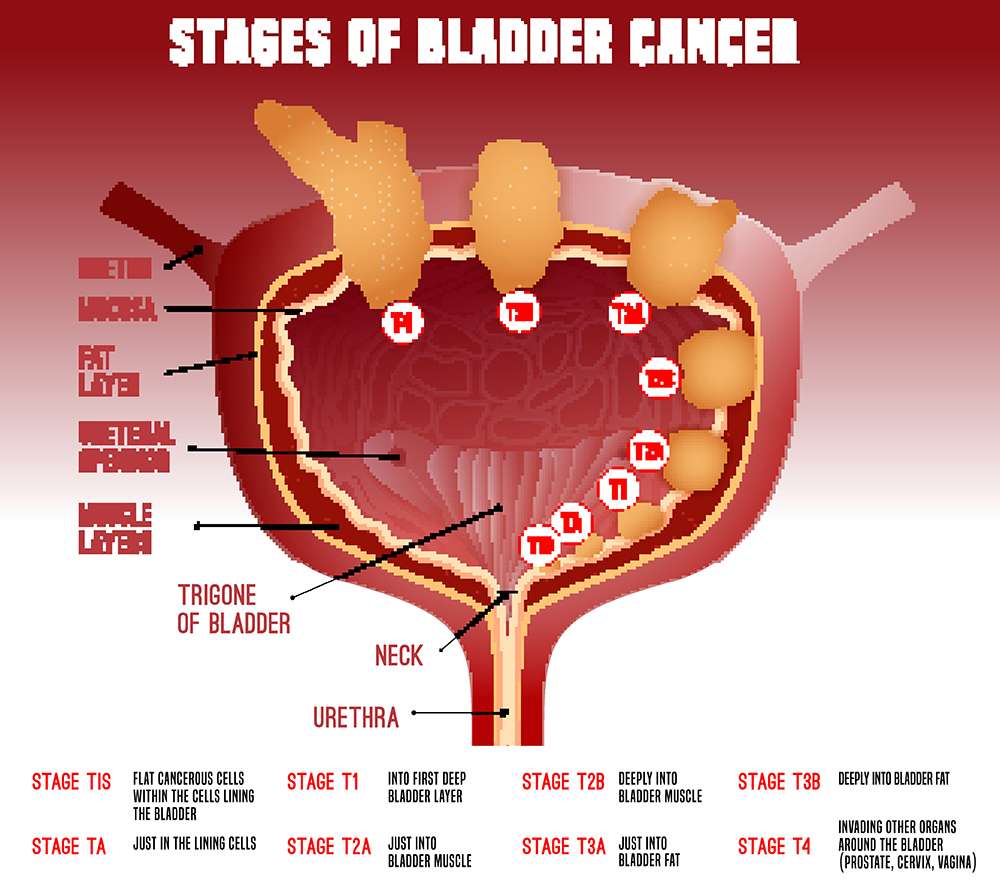
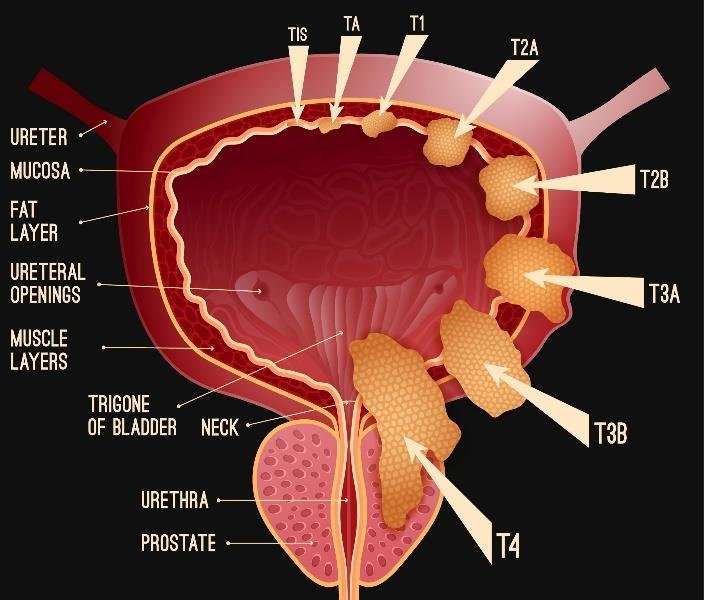
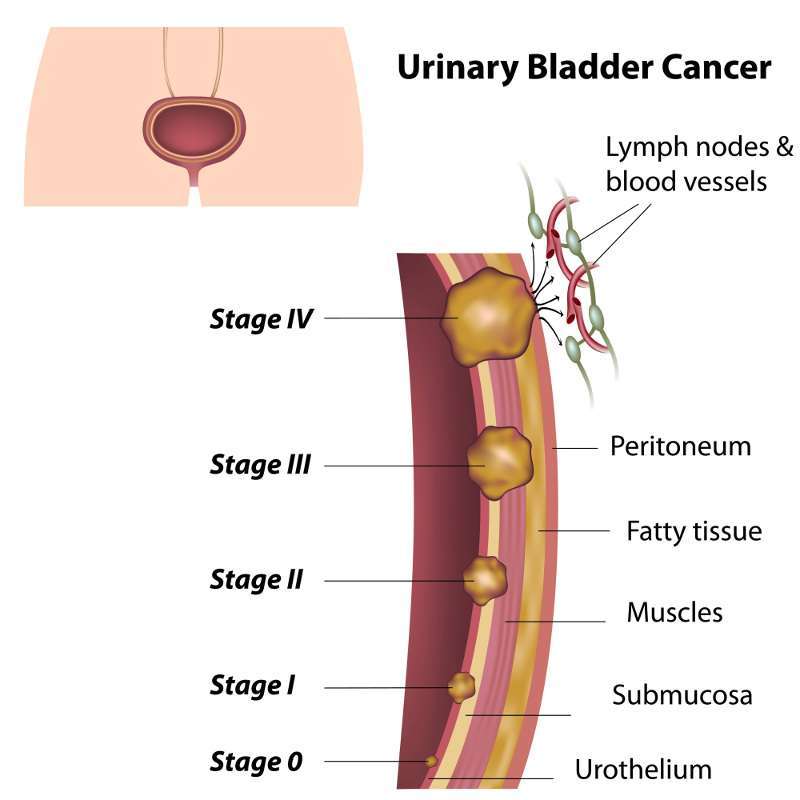
Ajcc Stage Groupings And Tnm Definitions
The American Joint Committee on Cancer has designated staging by TNM classification to define bladder cancer.
| Stage |
|---|
| Poorly differentiated. |
References
Recommended Reading: Bcg Chemo For Bladder Cancer
What Do I Need To Know To Prepare For Bcg Treatment
- Restrict your fluid intake, caffeinated beverages and use of diuretics 4 hours prior to procedure if possible.
-
Do not void for 1 to 2 hours after the procedure, if possible.
After your first urination following the procedure and for six hours afterward, you will be asked to follow these instructions:
-
Sit to void to avoid urine splashing. Do not use public toilets or void outside.
- After each void add 2 cups undiluted bleach to toilet, close the lid and wait 15-20 minutes and then flush the toilet. Repeat with each void for 6 hours.
- Increase fluid intake to dilute the urine. Begin after the first void post procedure.
- If you are sexually active, wear a condom with intercourse throughout the entire treatment course.
- If you have urinary incontinence, immediately wash clothes in clothes washer. Do not wash with other clothes.
- If wearing incontinence pad, pour bleach on pad, allow to soak in, then place in plastic bag and discard in trash.
- Acetaminophen or ibuprofen may be used for fever and body aches.
- You may need antispasmodic medication to help with frequency and urgency.
Bladder Cancer Clinical Trials
What about Clinical Trials?
You may hear about clinical trials for your bladder cancer. Clinical trials are research studies that test if a new treatment or procedure is safe and effective.
Through clinical trials, doctors find new ways to improve treatments and the quality of life for people with disease. Trials are available for all stages of cancer. The results of a clinical trial can make a major difference to patients and their families. Please visit our clinical trials research webpage to learn more.
Also Check: Heavy Feeling In Bladder And Frequent Urination
Prognosis And Survival For Bladder Cancer
If you have bladder cancer, you may have questions about your prognosis. A prognosis is the doctors best estimate of how cancer will affect someone and how it will respond to treatment. Prognosis and survival depend on many factors. Only a doctor familiar with your medical history, the type and stage and other features of the cancer, the treatments chosen and the response to treatment can put all of this information together with survival statistics to arrive at a prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person that the doctor will consider when making a prognosis. A predictive factor influences how a cancer will respond to a certain treatment. Prognostic and predictive factors are often discussed together. They both play a part in deciding on a treatment plan and a prognosis.
The following are prognostic and predictive factors for bladder cancer.
Survival Rates For Bladder Cancer
Survival rates can give you an idea of what percentage of people with the same type and stage of cancer are still alive a certain amount of time after they were diagnosed. They cant tell you how long you will live, but they may help give you a better understanding of how likely it is that your treatment will be successful.
Keep in mind that survival rates are estimates and are often based on previous outcomes of large numbers of people who had a specific cancer, but they cant predict what will happen in any particular persons case. These statistics can be confusing and may lead you to have more questions. Talk with your doctor about how these numbers may apply to you, as he or she is familiar with your situation.
Also Check: Yoga Exercises For Prolapsed Bladder
Standard Treatment Options For Stages Ii And Iii Bladder Cancer
The most common treatments for muscle-invasive bladder cancer are radical cystectomy and radiation therapy. There is no strong evidence from randomized controlled trials to determine whether surgery or radiation therapy is more effective. There is strong evidence that both therapies become more effective when combined with chemotherapy. The treatments with the highest level of evidence supporting their effectiveness are radical cystectomy preceded by multiagent cisplatin-based chemotherapy and radiation therapy with concomitant chemotherapy.
Radical cystectomy
Radical cystectomy is a standard treatment option for stage II and stage III bladder cancer, and its effectiveness at prolonging survival increases if it is preceded by cisplatin-based multiagent chemotherapy. Radical cystectomy is accompanied by pelvic lymph node dissection and includes removal of the bladder, perivesical tissues, prostate, and seminal vesicles in men and removal of the uterus, fallopian tubes, ovaries, anterior vaginal wall, and urethra in women. Studies of outcomes after radical cystectomy report increased survival in patients who had more, rather than fewer, lymph nodes resected whether this represents a therapeutic benefit of resecting additional nodes or stage migration is unknown. There are no randomized controlled trials evaluating the therapeutic benefit of lymph node dissection in this setting.
Evidence :
Evidence :
Segmental cystectomy
What Are Potential Side Effects And Complications Of Bcg Treatment
Benefits of this treatment outweigh risks and side effects.
Common side effects within 24 hours post procedure that do NOT need a phone call to the office include:
- Small amount of blood in urine
- Low grade fever
- Tiredness
- Urinary frequency, urgency and burning with urination
- Muscle or joint achiness
You will be given prescriptions to address the urinary symptoms if needed. You will be able to treat fever with over-the-counter pain/fever medication.
Other less common to rare side effects :
- Skin rash/ eruptions
- Fever greater than 101.3°F
- Nausea/vomiting/anorexia
- Blood in urine with inability to pass urine due to clots
- Urinary tract infection
- Neutropenia
- Tissue necrosis with leakage of fluid
- Pneumonitis
Intravesical BCG is contraindicated with the following conditions:
Last reviewed by a Cleveland Clinic medical professional on 07/23/2018.
References
Recommended Reading: What Medications Cause Overactive Bladder
Active Surveillance For Prostate Cancer Is It Right For You
HomeNews & MediaNewsActive Surveillance for prostate cancer is it right for you?
21 August 2020
If you have low risk prostate cancer, Active Surveillance is increasingly being recommended as a management option for your disease, in order to avoid unnecessary and invasive treatments when it is clinically safe to do so. Estimates suggest about 60% of low risk prostate cancers in Australia are managed with Active Surveillance. If you decide on Active Surveillance to manage your prostate cancer, its important to follow your surveillance protocol, in consultation with your doctor and specialists. This ensures that if your cancer starts to grow, it can be caught and treated before it spreads beyond the prostate. If you miss any tests on Active Surveillance, you increase your risks of unchecked disease progression, which could be harmful.
So, what is Active Surveillance, and is it a good treatment option for you?
How are prostate cancer treatment decisions made?
In deciding how best to treat your prostate cancer, your doctor needs to determine the type of cancer you have and how likely it is to progress to advanced disease.
Cancers that are not likely to grow and spread are considered low-risk prostate cancer, while those that are more likely to progress to advanced disease are considered high-risk prostate cancer. The grade and stage of the cancer helps determine the risk level.
To learn more about prostate cancer grading visit PCFAs website here.
Where Do These Numbers Come From
The American Cancer Society relies on information from the SEER* database, maintained by the National Cancer Institute , to provide survival statistics for different types of cancer.
The SEER database tracks 5-year relative survival rates for bladder cancer in the United States, based on how far the cancer has spread. The SEER database, however, does not group cancers by AJCC TNM stages . Instead, it groups cancers into localized, regional, and distant stages:
- Localized: There is no sign that the cancer has spread outside of the bladder.
- Regional: The cancer has spread from the bladder to nearby structures or lymph nodes.
- Distant: The cancer has spread to distant parts of the body such as the lungs, liver or bones.
You May Like: What Is The Best Medication For Bladder Infection
Carcinogenesis And Risk Factors
Increasing age is the most important risk factor for most cancers. Other risk factors for bladder cancer include the following:
- Use of tobacco, especially cigarettes.
- Family history of bladder cancer.
- HRAS mutation .
- Rb1 mutation.
There is strong evidence linking exposure to carcinogens to bladder cancer. The most common risk factor for bladder cancer in the United States is cigarette smoking. It is estimated that up to half of all bladder cancers are caused by cigarette smoking and that smoking increases a persons risk of bladder cancer two to four times above baseline risk. Smokers with less functional polymorphisms of N-acetyltransferase-2 have a higher risk of bladder cancer than other smokers, presumably because of their reduced ability to detoxify carcinogens.
When Is Brachytherapy Alone The Right Choice
For a patient with disease that is confined to the prostate and not too aggressive, brachytherapy alone is a good option. With the use of sophisticated real-time computer-based planning, we can use brachytherapy to deliver radiation in an extraordinarily precise way, with minimal exposure to the surrounding normal tissues. It is also convenient for the patient as it is done in an outpatient setting and most people are able to get back to work the next day.
But brachytherapy is not right for everyone. For some patients with less-aggressive disease, a watch-and-wait approach would also be very reasonable. At MSK, our philosophy is that when the disease is caught very early meaning a low PSA level, or nonaggressive disease as reflected by a Gleason score of 6 with evidence of cancer in only a few of the biopsy samples and no evidence from the MRI of a significant amount of disease then it would be very appropriate to do active surveillance and hold off on treatment.
You May Like: Where Is Your Bladder Woman
Selecting And Testing Gemcitabine
When Dr. Messing began research on gemcitabine as a possible way to reduce recurrences more than a decade ago, the drug was not widely used for bladder cancer. “We tried to pick an agent that we thought would be safe and effective,” he said.
The researchers decided to compare gemcitabine against placebo rather than mitomycin C, based on studies showing how infrequently patients received some form of chemotherapy following surgery despite guidelines recommending this approach.
“If the new procedure were adopted widely, we could spare patients a lot of suffering from repeated surgeries and save health care costs associated with those surgeries,” Dr. Messing said.
“Now that we have the results of the trial,” he went on, “we hope that patients and physicians will embrace this approach to treatment.”
What Is Bcg Treatment For Non
BCG is an intravesical immunotherapy using a bacteria of Mycobacterium bovis that has been reduced to cause less harm to the body. The bacteria is still kept viable so that it can actively work in the body to kill the cancer cells.
Intravesical is a way in which a medication is put into the bladder. Liquid drugs are put directly into the bladder through a catheter.
BCG is used as a therapy for and protection against bladder cancers that come back after a period of time in patients that have a more aggressive bladder cancer diagnosis. It is currently the most effective treatment.
Recommended Reading: I Feel A Lot Of Pressure On My Bladder
Treating Stage 0 Bladder Cancer
Stage 0 bladder cancer includes non-invasive papillary carcinoma and flat non-invasive carcinoma . In either case, the cancer is only in the inner lining layer of the bladder. It has not invaded the bladder wall.
This early stage of bladder cancer is most often treated with transurethral resection with fulguration followed by intravesical therapy within 24 hours.
Box : Criteria For The Diagnosis Of Prostatic Adenocarcinoma9
-
Major criteria
-
Architectural: infiltrative small glands or cribriform glands too large or irregular to represent highgrade prostatic intraepithelial neoplasia
-
Nuclear atypia: nuclear and nucleolar enlargement
Minor criteria
Nuclear hyperchromasia
Before searching for these criteria, it is important to scan sections of the needle core tissue, at both lowpower and highpower magnification, in order to appreciate the architecture and cytological features of benign glands in the tissue. The arrangement of the benign glands and the nuclear appearances of the lining cells serve as important points of reference for comparison when evaluating atypical glands because there can be substantial variability between individual cases in histological characteristics because of differences in fixation, section thickness and H& E staining.
Figure 6Comedocarcinoma, highgrade Gleason pattern 5, with comedonecrosis.
Figure 8Penetration of smallgland prostatic adenocarcinoma into the seminal vesicle or ejaculatory duct wall. It is difficult to tell, on needle biopsy, whether this is definitely a seminal vesicle or an ejaculatory duct. Seminal vesicle or ejaculatory duct glands are crowded larger glands at lower right.
Figure 9Minimal adenocarcinoma. Compared with staining by haematoxylin and eosin , the 34E12 and p63 immunohistochemical stains highlight the invasion of the malignant glands, which lack basal cells .
You May Like: My Bladder Always Feels Full
What Active Surveillance Means
For many men, prostate cancer never affects their lives, said Christopher L. Runz, DO, attending urologist at University of Maryland Shore Regional Health. Active surveillance means we actively watch the cancer and make sure it stays low-grade, which means the cancer may potentially never spread.
Active surveillance requires regular prostate specific antigen screenings and MRIs, with occasional biopsies. Men who are older and have a shorter life expectancy become candidates for active surveillance when they have a Gleason score of 7 .
Standard Treatment Options For Stage I Bladder Cancer
Patients with stage I bladder tumors are unlikely to die from bladder cancer, but the tendency for new tumor formation is high. In a series of patients with Ta or T1 tumors who were followed for a minimum of 20 years or until death, the risk of bladder recurrence after initial resection was 80%. Of greater concern than recurrence is the risk of progression to muscle-invasive, locally-advanced, or metastatic bladder cancer. While progression is rare for low-grade tumors, it is common among high-grade cancers.
One series of 125 patients with TaG3 cancers followed for 15 to 20 years reported that 39% progressed to more advanced stage disease, while 26% died of urothelial cancer. In comparison, among 23 patients with TaG1 tumors, none died and 5% progressed. Risk factors for recurrence and progression include the following:
- High-grade disease.
TUR with fulguration followed by an immediate postoperative instillation of intravesical chemotherapy
TUR and fulguration are the most common and conservative forms of management. Careful surveillance of subsequent bladder tumor progression is important. Because most bladder cancers recur after TUR, one immediate intravesical instillation of chemotherapy after TUR is widely used. Numerous randomized, controlled trials have evaluated this practice, and a meta-analysis of seven trials reported that a single intravesical treatment with chemotherapy reduced the odds of recurrence by 39% .
TUR with fulguration
Evidence :
You May Like: What To Take When You Have A Bladder Infection
Prognosis And Life Expectancy
In general, papillary urothelial cancers have a better prognosis than other types of bladder cancer. Your specific outlook depends on the stage and grade of your cancer. High-grade cancers can spread. Low-grade papillary cancers are less likely to spread. Papillary cancers can also return after theyve been treated.
Stage Iv Bladder Cancer Treatment
Only a small fraction of patients with stage IV bladder cancer can be cured, and for many patients, the emphasis is on palliation of symptoms. The potential for cure is restricted to patients with stage IV disease with involvement of pelvic organs by direct extension or metastases to regional lymph nodes.
Don’t Miss: Botox Dose For Overactive Bladder
What Is A 5
A relative survival rate compares people with the same type and stage of bladder cancer to people in the overall population. For example, if the 5-year relative survival rate for a specific stage of bladder cancer is 90%, it means that people who have that cancer are, on average, about 90% as likely as people who dont have that cancer to live for at least 5 years after being diagnosed.