What Causes Neurogenic Bladder
Neurogenic bladder can be congenital . Birth defects that can cause neurogenic bladder include:
- Spina bifida : This disorder occurs when the fetus’ spine does not completely develop during the first month of pregnancy. Babies born with myelomeningocele often have paralysis or weakness that affects how the bladder works.
- Sacral agenesis: This is a condition in which parts of the lower spine are missing.
- Cerebral palsy: Cerebral palsy is a group of chronic disorders that weaken a person’s ability to control body movement and posture. These disorders result from injury to the motor areas of the brain. The problem causing cerebral palsy may occur while the infant is still in the womb or after birth. Cerebral palsy is not always found during a child’s first year of life.
Various medical conditions can cause neurogenic bladder, including the following:
- Stroke
- Heavy metal poisoning
Neurogenic Bladder Treatment And Home Remedies
Your care will depend on whatâs causing your symptoms and how serious they are. Thereâs no cure for neurogenic bladder, but you can manage your symptoms and get control.
If you have OAB, you may need to:
- Train your bladder. You can do this by squeezing your pelvic floor muscles during the day or when you need to pee .
- Hold it, if you can. Delayed voiding is when you wait a few minutes to urinate after you feel the urge. The goal is to extend this time to a few hours.
- Pee on a schedule. You might avoid accidents if you urinate at certain times of the day.
- Take medicine. Some medications can relax bladder muscles and stop spasms.
- Keep a healthy weight. Extra body mass can add pressure to your bladder.
- Change your diet. Things like caffeine, alcohol, spicy foods, dairy, artificial sweeteners, chocolate, and citrus fruit can irritate your system.
- Use electrical stimulation. A device under your skin sends electricity to the nerve that controls your bladder. These painless pulses help stop overactive signals that tell your brain to pee.
- Get Botox. Your doctor can inject this neurotoxin into your bladder to temporarily stop it from contracting too much. If you have problems emptying your bladder or have urinary tract infections often, this treatment isn’t an option.
If you have UAB, you may need to:
Columbia University Irving Medical Center: âNeurogenic Bladder.â
Urology Care Foundation: âWhat is Neurogenic Bladder?â
Additional Overactive Bladder Treatment
If making the above lifestyle changes does not work to relieve overactive bladder, a doctor may recommend other treatments, such as:
- Drug treatment: In some cases, a doctor may inject botulinum toxin into the bladder muscle to stop it from contracting as much. Botox can wear off after a period of time, so a person may need to have injections every 612 months.
- Sacral neuromodulation: This treatment stimulates the nerves with electricity, especially the sacral nerve, which relays signals from the spinal cord to the bladder.
- Percutaneous tibial nerve stimulation: During this treatment, a doctor inserts a needle into the tibial nerve, which is in the leg. They then stimulate this nerve with electrical impulses. These impulses travel to the sacral nerve. A person usually needs to receive 12 sessions of this treatment.
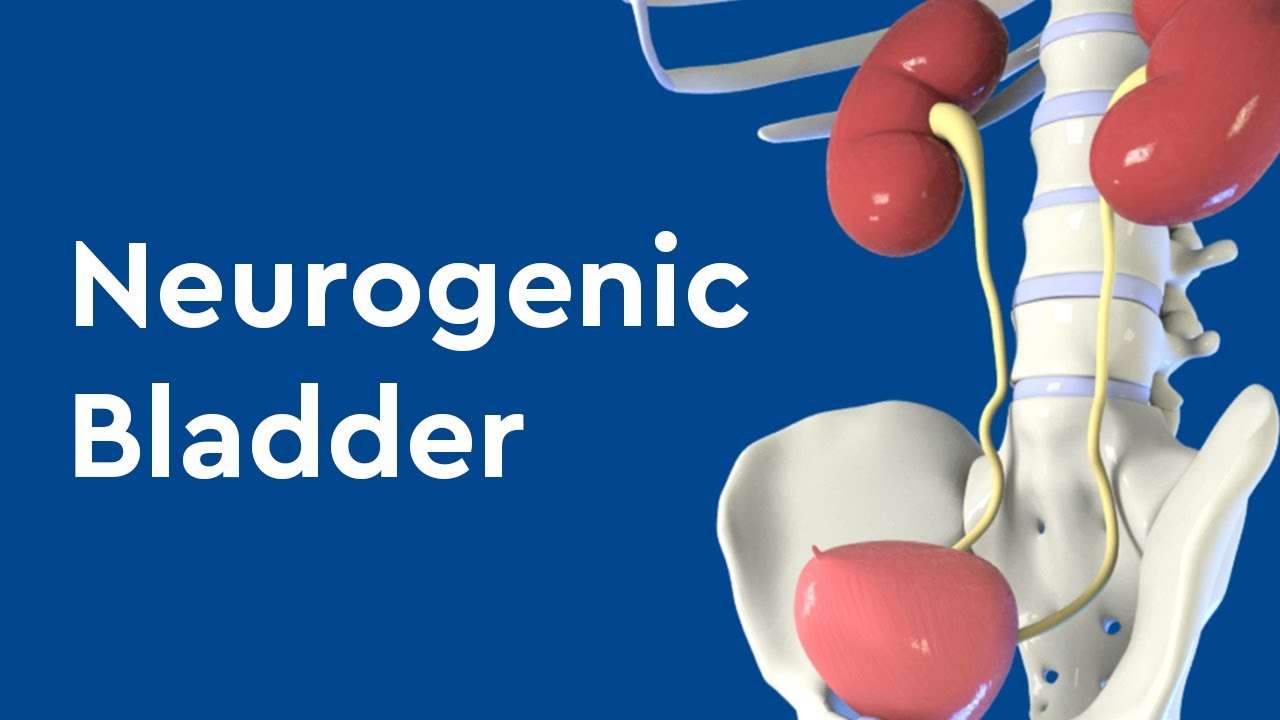
What Is The Bladder
The bladder is a hollow organ located in the pelvis, or lower abdomen. The bladder has two important functions:
- It stores urine.
- It removes urine from the body through a complex communication circuit in the spinal cord and brain.
Urinary incontinence occurs when a person cannot control the flow of urine. The storage of urine can be a problem if the bladder is unable to empty fully or if it begins to empty itself before the person reaches the bathroom . Leakage can occur if the bladder cannot empty , if the sphincter controlling urination doesnt work , or if bladder spasms cause the bladder to shrink before the person reaches the toilet .
How Is Neurogenic Bladder Treated
The main treatments for neurogenic bladder are the following:
- Clean intermittent catheterization : Catheters are thin, flexible tubes that can be inserted through the urethra and into the bladder to drain urine.
- Drugs: Medications are prescribed to improve your bladder function. Specific medications for neurogenic bladder depend on if your bladder is overactive or underactive or both.
- Injections of botulinum A toxin : A doctor injects Botox into the bladder or urinary sphincters.
- Bladder augmentation : This is a surgery in which segments of the intestine are removed and attached to the walls of the bladder. This reduces the bladder’s internal pressure and increases its ability to store urine.
- Ileal conduit: Part of the small bowel is used to make a urine stoma. This stoma drains to a bag attached to the outside of the body.
- Lifestyle changes: These might include avoiding certain foods or drinks that can irritate the bladder. These include certain caffeinated drinks like coffee, carbonated beverages, spicy foods, and citrus fruit. Losing weight can ease stress on the bladder. A behavioral treatment called delayed voiding may help some people with urine control.
Absorbent undergarments, pads, panty shields, panty liners, and adult diapers can help prevent wetness and odors while protecting skin and clothing. Bed pads can protect sheets and mattresses.
Treatment Of Interstitial Cystitis And Neurogenic Bladder With Classical Chinese Acupuncture And Herbal Medicine
Interstitial Cystitis and Neurogenic Bladder have a long history of treatment with Classical Chinese Acupuncture and Herbal Medicine
Neurogenic bladder is a general term for a condition that can be the result of different diseases involving damage, by illness or injury, to the nervous systems ability to adequately control the muscular control of bladder emptying. Bladder emptying is the result of complicated feedback mechanisms between the nerves and muscles, and when this is damaged, by disease, injury, or nervous system dysfunction it effects the critical muscles ability to tighten or relax the sphincter at the base of the urinary bladder.
Neurogenic bladder includes hyperactive or overactive bladder, in which the person has to urinate too often in small amounts, has problems voiding completely, or has complete loss of bladder control.
Underactive bladder, on the other hand, involves the Bladder becoming too full with a consequent leakage of smaller amounts of urine. In underactive bladder the person often suffers from the inability to tell when the bladder is full, from difficulties with the the beginning of urination, from diffulties emptying all the urine from the bladder, and with wholescale urinary retention.
then treatment is very promising, using a combination of dietary, nutrtional, acupuncture, and Chinese herbal medicine therapies.
Interstitial Cystitis
LIVER DEPRESSION with QI STAGNATION
DEPRESSIVE HEAT
SPLEEN EMPTYNESS WITH DAMP
Transurethral Electrical Bladder Stimulation
You Have Already Helped Us Learn:
- Lithium carbonate wasn’t helping ALS patients, and we learned it faster than the clinical trials did. Read about it inNature.
- Insomnia is more commonin fact worsefor people with chronic conditions. Read about it on theblog.
- Interacting with other PatientsLikeMe members improves your health. Read it onhealthaffairs.org.
- The severity of Parkinson’s Disease symptoms changes faster than researchers thought, so clinical trials should be designed differently. Read about it on JMIR.
Urinary Tract Reconstruction Surgery
3.5.1. Augmentation Enterocystoplasty
To improve our ability to make clinical decisions and identify changes in UUTD pre- and post-treatment, we recently introduced two innovations . Evaluating the midterm outcomes using these tools demonstrated conclusively that augmentation enterocystoplasty provides effective and safe UUT protection in patients with moderate and severe upper urinary tract deterioration and renal function impairment resulting from VUR and UUTD .
3.5.2. Tissue-Engineering Bladder Augmentation
Medical Therapy And Devices For Neurogenic Bladder
Besides behavioral therapy, there are medications and devices used to treat neurogenic bladder, including:
- Anticholinergic drugs: Several medications are available that may help people with frequent or urgent urination, or leakage due to neurogenic bladder. Anticholinergic drugs act by relaxing the muscles of the bladder, and decreasing the urgency or leakage due to overactivity or spasms of the bladder. The drugs have many side-effects, such as drowsiness, blurred vision, heart palpitations and facial redness. Patients may need to try several drugs before finding one that works well.
- Antispasmodic drugs: Antispadmodic medications also work by relaxing the muscles of the bladder. This can increase the capacity of the bladder and decrease the need to urinate frequently. These drugs have similar side effects to anticholinergic medications and may interfere with activities that require physical coordination and mental alertness, such as driving or operating heavy machinery.
- Antidepressant drugs: Certain antidepressant drugs can be used to treat bladder problems, although they are not approved by the Food and Drug Administration for these uses. The drugs work by relaxing the muscles of the bladder and can be used to treat frequent urination .
Intravesical Instillation Of Gentamicin Neomycin
The authors stated that this study had several drawbacks. First, in all retrospective analyses, there were inherent limitations. Second, the pooled sample size was not powered to demonstrate the safety or efficacy of long-term modified intravesical oxybutynin therapy in children with NGB. Third, the ideal study would be a prospective, randomized, placebo controlled trial. Challenges and limitations of trial design for pediatric patients with refractory NGB included patient heterogeneity, and the small number of patients in whom traditional urotherapy failed.
Guidelines from the European Association of Urology state that, to reduce detrusor overactivity, antimuscarinics can also be administered intravesically The guidelines state that the efficacy, safety and tolerability of intravesical administration of 0.1% oxybutynin hydrochloride compared to its oral administration for treatment of neurogenic bladder has been demonstrated in a randomized controlled study The guidelines state that this approach may reduce adverse effects because the antimuscarinic drug is metabolised differently and a greater amount is sequestered in the bladder, even more than with electromotive administration.
Neurogenic Bladder Diagnosis & Testing
Since neurogenic bladder involves the nervous system and the bladder, a variety of tests are conducted to determine the status of both. Urodynamic studies are conducted to measure bladder capacity, bladder pressures, urine flows, and bladder emptying.
The skull, spine, and urinary tract may be imaged with x-rays, magnetic resonance imaging , and computed tomography . An electroencephalogram may be taken to ascertain brain activity. EEG reveals activity in neural areas of the brain thought to control bladder function.
Departments
Initial Evaluation Of The Patient With Nlutd
Guideline Statement 1
- Pelvic and vaginal examination in females
- Genital examination and digital rectal exam
- Rectal: tone, masses, reflexes, prostate assessment
- Skin integrity of pelvis, perineum, buttocks, lower back, and lower extremities
- Directed neurological assessment: sensory, motor, spasticity, etc.
- Evaluation of bulbocavernosus, anal, and cremasteric reflexes
- Tone of anal sphincter and voluntary contraction of the anal sphincter and pelvic floor muscles
UA is performed to assess for hematuria, pyuria, glucosuria, proteinuria, and other findings which may prompt further evaluation. Abnormalities should be interpreted in the context of the patients underlying condition, symptoms, and the presence or absence of a urinary catheter. An initial abnormal dipstick UA may prompt a formal microscopic examination of the urine. Additional evaluations in individuals with NLUTD demonstrating an abnormal UA are discussed in relevant sections later in this Guideline.
Ultimately, the initial evaluation is part of the risk stratification process which may or may not lead to further investigations, such as urinary tract imaging or multichannel UDS, in some individuals.
Guideline Statement 3
3. At initial evaluation, patients with NLUTD who spontaneously void should undergo post-void residual measurement.
Discussion
Guideline Statement 4
4. At initial evaluation, optional studies in patients with NLUTD include a voiding/catheterization diary, pad test, and non-invasive uroflow.
Peer Review And Document Approval
An integral part of the guideline development process at the AUA is external peer review. The AUA conducted a thorough peer review process to ensure that the document was reviewed by experts in the diagnosis and management of NLUTD. In addition to reviewers from the AUA PGC, Science and Quality Council, and Board of Directors, the document was reviewed by representatives from SUFU as well as external content experts. Additionally, a call for reviewers was placed on the AUA website from May 26 June 7, 2021 to allow any additional interested parties to request a copy of the document for review. The guideline was also sent to the Urology Care Foundation to open the document further to the patient perspective. The draft guideline document was distributed to 34 peer reviewers. All peer review comments were blinded and sent to the Panel for review. In total, 23 reviewers provided comments, including 3 external reviewers. At the end of the peer review process, a total of 825 comments were received. Following comment discussion, the Panel revised the draft as needed. Once finalized, the guideline was submitted for approval to the AUA PGC, Science and Quality Council, and Board of Directors, as well as the governing bodies of SUFU for final approval.
Treatment For Neurogenic Bladder
Neurogenic bladder is a serious condition, but when it is monitored closely and treated properly patients can experience significant improvements in their quality of life. Our doctors routinely participate in the management of neurogenic bladder with the goal of preserving patients’ kidney function and keeping them dry. Using state of the art equipment and technology, we provide patients with excellent care and monitor them over the long term.
How Is Neurogenic Bladder Diagnosed
A doctor will do an exam and may order several tests of the nervous system and the bladder to diagnose neurogenic bladder: These include:
- Urodynamic studies: These bladder function tests measure how much urine the bladder can hold, the pressure within the bladder, how well urine flows, and how well the bladder empties when it is full. Special sensors may be placed on the skin near the urethra or rectum to see if the muscles and nerves in those parts of the body are working properly.
- Cystoscopy: The doctor may perform this procedure to examine the inside of the bladder and urethra with the use of a small telescope .
- X-rays
What Should You Do If You Are Having Symptoms
It is important to talk with your health care provider and find out what is causing your symptoms. The symptoms of neurogenic bladder may seem like the symptoms of other illnesses and medical problems. Your health care provider can help rule out other issues.
Sometimes neurogenic bladder symptoms can lead to more serious bladder problems. But there are a number of treatments available. You and your health care provider can decide which treatment is best for you.
What Is Neurogenic Bladder
Neurogenic bladder is when a problem in your brain, spinal cord, or central nervous system makes you lose control of your bladder. You may pee too much or too little. You could have symptoms of both overactive bladder and underactive bladder . You may not be able to fully empty it.
Itâs normal to have some stress and anxiety if you canât control when you urinate. Talk to your doctor about whatâs going on as soon as possible so you can start on a treatment to help manage your symptoms.
Autologous Mesenchymal Stem Cells
Mahajan and colleagues stated that neurogenic bladder is a term applied to a mal-functioning urinary bladder due to neurologic dysfunction or insult emanating from internal or external trauma, disease, or injury. These investigators reported on a case of neurogenic bladder following laminectomy procedure and long-standing diabetes mellitus with neuropathy treated with autologous mesenchymal stem cells . In this single-case study, the authors highlighted differentiation potential and paracrine effects of mesenchymal stem cells on bladder function. Moreover, they stated that regular follow-up to monitor progression/improvement of the condition is mandatory and further trials and novel routes of administration are needed to improve the effectiveness of cellular therapy in various conditions.
Behavioral Therapy For Neurogenic Bladder
In some cases, behavioral therapy can help patients regain control of the bladder. This includes:
- Bladder training: This involves sticking to a fixed voiding schedule that is prepared by the patient and their health care provider. The schedule should be followed regardless of whether the patient has an urge to urinate or not. The goal of the training is to increase the volume of fluids the bladder can store, as well as the amount of time between emptying the bladder. The interval between voiding is expanded in 15 to 30 minute growths until the patient is comfortable holding their urine for several hours. Sometimes drinking less fluid will be recommended.
- Biofeedback: Electrodes are placed on the skin and a monitor is positioned to help the patient feel and visualize the activity of their urinary tract and other bodily functions. This technique is often combined with pelvic floor exercises. After several biofeedback sessions, the patient may learn to control the muscles that control urination.
- Pelvic floor muscle exercises: Pelvic floor exercises, also known as Kegel exercises, work to strengthen the muscles and connective tissue that support the pelvic organs so that the individual can better control the flow of urine. With practice, patients learn to relax and contract the muscles that control urination. These exercises can significantly minimize leakage or allow the patient to more completely empty their bladder.