Why Does Urinary Incontinence Occur With Pregnancy
Pregnancy and childbirth can cause incontinence in several ways:
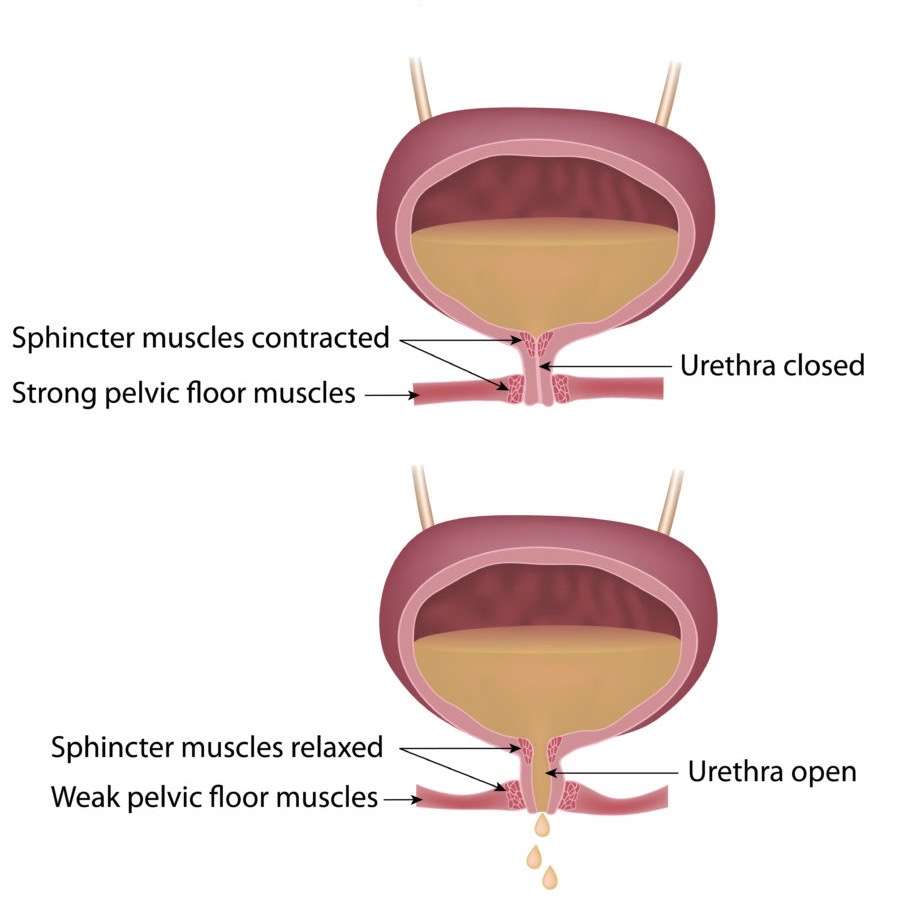
- Your growing baby takes up a lot of room. As the uterus expands, it puts increased pressure on the bladder, urethra, and pelvic floor muscles. This can lead to leakage.
- Changing progesterone levels during pregnancy can weaken the pelvic floor. Increases in this hormone loosen up your ligaments and joints so the belly can expand and so you can deliver. But it can also loosen ligaments in the pelvis that help you hold in urine.
- Childbirth, particularly vaginal delivery, can stretch and weaken the pelvic floor muscles. This can lead to pelvic organ prolapse, in which your bladder, uterus, or rectum droops into the vaginal canal. Prolapse can be associated with urinary incontinence.
- Vaginal delivery also can result in pelvic muscle and nerve injury, which can result in bladder control problems.
If you experience urinary incontinence during pregnancy, you are at higher risk of having a persistent problem after birth. Tell your health care provider about urinary incontinence symptoms as soon as you notice them during pregnancy or at your first postnatal visit.
More than 80% of postpartum women who experience SUI symptoms during pregnancy may continue to experience stress incontinence without treatment.
Related reading:Body after birth: Treating post-pregnancy problems
Peeing Your Pants After Pregnancy Is Preventable
Stress urinary incontinence may be a side effect of giving birth, but several treatment options can help clear it up.
This guide was originally published on Oct. 17, 2019 in NYT Parenting.
About six weeks after giving birth to my daughter, I headed out for a quick run a much-needed break from the new-baby routine and a chance to reconnect with an activity I loved. Ten minutes in, I felt a warm sensation Id never before experienced. It was not the glow of new motherhood. I had peed my running shorts.
More scientifically, Id had my first brush with stress urinary incontinence, the inability to control urine flow while coughing, laughing or exercising. The problem isnt uncommon. Urinary incontinence which encompasses urge incontinence , stress incontinence and a mix of the two is estimated to affect about half of adult women. The overall risk increases with age, but stress incontinence also shows up in younger women, in part because of giving birth.
While the problem sometimes goes away on its own, for some women it lingers. Yet one study showed that only about 25 percent of women affected by incontinence seek care many simply make do by using incontinence pads to catch the leakage. There are, however, both surgical and nonsurgical remedies that can help eliminate messy accidents.
For this guide, I consulted three obstetrician-gynecologists with specialties in urogynecology or pelvic medicine and two physical therapists specializing in pelvic floor therapy.
Drink Plenty Of Water
Drink 6 to 8 glasses of fluid a day unless your doctor advises you otherwise.
Many people with urinary incontinence avoid drinking fluids, as they feel it causes more problems. However, limiting your fluid intake makes incontinence worse, because it reduces your bladder’s capacity.
Not drinking enough fluid can also cause constipation or make it worse.
Find out which are the healthiest drinks.
Recommended Reading: New Treatments For Neurogenic Bladder
Does Childbirth Inevitably Lead To Incontinence
The vast majority of women who give birth do not develop incontinence. In most cases, the damage created by childbirth repairs itself over time as the tissues go through the normal healing process. The majority of women experience no residual effect within just a few months after childbirth. Almost half of all women who have a vaginal delivery show immediate recovery of the nerves’ ability to carry messages to the pelvic muscles, and 60% will have complete resolution within two months. However, in some women, the injured tissue does not recover 100% of pre-labor strength. For them, the likelihood of incontinence and the discomfort of pelvic prolapse developing later in life are more common.
Treating Overactive Bladder And Incontinence Issues
Just because bladder issues are a normal part of pregnancy, you dont have to continue to endure it. Dr. Kohli offers numerous solutions based on the severity of your symptoms.
During your appointment, Dr. Kohli performs a full physical exam to identify the specific cause of your incontinence issues. To treat problems like overactive bladder, he often recommends:
- Medications designed to relax your bladder
- Physical therapy techniques to strengthen your pelvic floor muscles
- Botox® injections to temporarily disable your bladder muscles
- The InterStim system to restore healthy nerve function in the area
In addition to medical interventions for urinary incontinence, Dr. Kohli often makes lifestyle and behavioral recommendations as well. These approaches often include tracking your diet and fluid intake, addressing weight management issues, and undergoing bladder training. For severe incontinence cases, Dr. Kohli could suggest surgery.
To find help for your post-pregnancy overactive bladder and incontinence issues, visit one of our convenient locations in Wellesley or South Weymouth, Massachusetts. Give us a call at Boston Urogyn, send us a message here on our website, or request an appointment using our convenient online feature.
You Might Also Enjoy…
Do The Right Exercises
High-impact exercise and sit-ups put pressure on your pelvic floor muscles and can increase leaks.
To strengthen your pelvic floor to relieve symptoms, replace high-impact exercise, such as jogging and aerobics, with strengthening exercise, such as pilates.
Pilates strengthens your core muscles, which is beneficial for stress incontinence.
Can Childbirth Weaken The Rectum
Likewise, the muscle and connective tissues that hold the rectum in its place under the vagina may be weakened or torn by labor and delivery, which allows the rectum to bulge up into the vagina. The words rectal prolapse or rectocele are often used by doctors to describe these changes in the contour of the vagina. After delivery of a baby, some degree of prolapse is very common. However, in most women these changes heal and resolve within a few months without any treatment. If the problem is severe and does not resolve, some repair might need to be done.
An Extremely Common Condition
Sorry to report this, but postpartum urinary incontinence is quite common. According to the latest research, women who give birth vaginally are more likely to experience these complications afterward. In some cases, issues of urinary incontinence can last up to a year, and smaller percentages of women are still living symptoms after 5 years.
Contributing factors include the fact that the bladder and pelvis muscles are weakened during childbirth. In addition, the uterus will begin to shrink back to its normal size, which causes repeated compressions on the bladder. Rapid changes in hormones also need to be considered as the body attempts to balance its female sex hormones after a child is born. Women over the age of 35 and those who are obese are also at a greater risk for urinary incontinence following childbirth.
All together, these influential factors lead women to face a much higher risk for urinary incontinence. The good news is that most women can recover with the proper precautions and effective treatment options recommended by Dedicated to Women.
What Role Does Forceps Delivery Play In Incontinence
Forceps increases the risk of injury to the nerves and muscles of the pelvis. Forceps are the spoon-shaped metal instruments that are sometimes inserted into the mother’s vagina and placed around the baby’s head at the time of delivery. These instruments are usually used after a long or difficult labor to help deliver a baby. As the doctor pulls on the forceps, they push away the muscles and soft tissues in the pelvis, allowing more room for the baby to come out. The forceps also help the doctor to pull the baby out, especially if there is a tight fit. However, because the instruments are made of metal and take up space of their own, they increase the risk of stretching and tearing the vagina and supporting tissues of the pelvis. They also put more force against the nerves that run inside the pelvis. As a result, more harm can be done to the tissues, possibly resulting in long-term damage and eventual incontinence.
Because there is a risk of complications with forceps to mother or baby, they should probably not be used to deliver a baby unless there is a rapid drop in the baby’s heartbeat, severe bleeding or other emergency that dictates a quick delivery.
How Do I Do Kegel Exercises
Kegel exercises, also called pelvic floor exercises, help strengthen the muscles that support the bladder, uterus and bowels. By strengthening these muscles during pregnancy, you can develop the ability to relax and control the muscles in preparation for labor and birth.
Kegel exercises are highly recommended during the postpartum period to promote the healing of perineal tissues, increase the strength of the pelvic floor muscles and help these muscles return to a healthy state .
To do Kegel exercises, imagine you are trying to stop the flow of urine or trying not to pass gas. When you do this, you are contracting the muscles of the pelvic floor, and are practicing Kegel exercises. While doing these exercises, try not to move your leg, buttock or abdominal muscles. In fact, no one should be able to tell that you are doing Kegel exercises.
Kegel exercises should be done every day. Doing five sets of Kegel exercises a day is recommended. Each time you contract the muscles of the pelvic floor, hold for a slow count of 10 seconds and then relax. Repeat this 15 times for one set of Kegels.
Last reviewed by a Cleveland Clinic medical professional on 06/11/2020.
References
Can Episiotomy Lead To Anal Incontinence
Just before the delivery of the baby’s head, an incision may be made by the doctor in the skin and, sometimes, also in the muscle at the bottom portion of the vagina to allow more room for the baby to deliver. This incision, called episiotomy, is supposed to avoid incidental tearing of the vagina or rectum as the baby delivers. Episiotomy is a recent practice, devised in order to substitute a straight, clean, easy-to-repair surgical incision for the jagged tear that might otherwise occur. Cutting this incision is also intended to shorten labor by giving the baby’s head more room so delivery might be easier and faster. It was thought that faster delivery would decrease the risk of injury to the mother’s bladder, and would be gentler for the baby’s head. However, studies show no evidence that these assumptions are true.
Behind Postpregnancy Problems With Oab
During your pregnancy, you may have developed some minor issues with incontinence, which makes sense given that your growing baby placed more pressure on your urinary tract, namely on your bladder and on your bladder sphincter.
In many cases, these incontinence problems resolve themselves shortly after childbirth, but many women are left with ongoing OAB, which may be caused by:
- A weakened pelvic floor
To put some numbers to the problem, at least 40% of women in the United States have OAB, mainly due to pregnancy and menopause.
How Can Loss Of Bladder Control Due To Pregnancy Or Childbirth Be Prevented
Labor and vaginal delivery have an impact on the pelvic floor muscles and nerves that affect bladder control, so you should discuss your options with your healthcare provider.
Cesarean sections are associated with a lower risk of incontinence or pelvic prolapse than vaginal deliveries, but they may present other risks. Large babies who weigh more than 9 pounds at birth may increase the risk of nerve damage during delivery.
Exercising pelvic floor muscles with Kegel exercises can help prevent bladder control problems.
Bladder control problems might show up months to years after childbirth. Talk to your healthcare team if this happens to you.
How To Treat Urinary Incontinence After Pregnancy
Incontinence is common, nothing to be ashamed of, and completely manageable.
You may have expected a few stretch marks after your pregnancy, but you maybe didnt expect a bit of urinary leakage every time you laugh or cough. Urinary incontinence isnt something many new moms talk aboutjust dealing with the issue is difficult enough, and the embarrassment keeps a lot of women from seeking treatmentbut its quite common.
The physical stresses of pregnancy, labor, and delivery can contribute to the development of urinary incontinence, and for many women, if not treated, can become a chronic condition. Read on for effective treatments for every typeyes, theres more than oneof urinary incontinence.
What Treatments Are Available To Me If My Incontinence Doesnt Go Away After A Year
While kegels and behavioral therapy work well for most men with mild to moderate leaking, they may not be completely effective for some. Luckily, there are still some options for treating bladder leakage after prostate surgery.
Another surgery is sometimes needed when bladder leaks persist for more than a year after surgery. This may consist of having a urethral sling procedure, or an artificial urinary sphincter.
With a urethral sling procedure, a synthetic mesh tape is implanted to support the urethra. Up to an 80% improvement has been seen with this procedure and some men stop leaking completely.
An artificial urinary sphincter is used in patients who have more severe urinary incontinence that is not improving, or for those patients who may have had a lot of damage to the sphincter muscle after prostate surgery. An artificial urinary sphincter is a mechanical ring that helps close the exit from the bladder.
As will all surgeries, these come with pros and cons and potential complications. Be sure to discuss these options with your doctor.
Lifestyle Changes To Reduce Urinary Incontinence
Along with Kegel exercises, there are a few other noninvasive methods to eliminate or reduce the risk of urinary incontinence:
- Lose weight. Excess body weight puts pressure on the bladder. Even a 10% reduction in weight can significantly help with urinary incontinence. Work with your doctor to manage your weight gain during pregnancy, and after the birth of your little one, returning to your pre-pregnancy weight will help relieve the pressure on your bladder and pelvic floor.
- Quit smoking. Smoking has been shown to increase the risk of urinary incontinence as it leads to bladder irritation and chronic coughing.
- Make dietary changes. Some foods and beverages can make incontinence worse. These include caffeine, alcohol, and spicy and acidic foods. This is especially important if you experience urinary frequency and urgency and have trouble making it to the bathroom once you have the urge to urinate. Constipation can worsen symptoms of urine leakage. Stool in the rectum can put pressure on the bladder, urethra, and pelvic floor, so include plenty of higher-fiber foods and fluids in your daily diet.
How To Stop Bladder Leakage After Hysterectomy
Regardless of the cause of your bladder leakage, there are options to improve it considerably in most cases. One approach that can help: Train the muscles that support your bladder. At no time in a woman’s life should she consider urinary incontinence as something normal or what she can expect as she ages.
There are several things you can try to get better bladder control and fix light bladder leakage. Here are a few hints you can easily incorporate into your daily life that will help to correct embarrassing bladder leakage after a hysterectomy.
Where Are The Pelvic Floor Muscles
During initial exam, I often use a clock visual to help women know where their pelvic floor muscles can be palpated. If you lie on your back, imagine the top of the opening of your vagina is 12 oclock and the bottom of the opening is 6 oclock.
The pelvic floor muscles are easiest to palpate at the 5 oclock and 7 oclock positions about even with where your legs meet your hips and approximately 3 to 4 centimeters above the vaginal opening.
These are the same muscles you contract when you try to stop the flow of urine midstream or if you were to tighten your vagina around a tampon. And these are the muscles you contract to do Kegel exercises. These pelvic floor muscle exercises were named after Dr. Arnold Kegel, who described them in the 1940s to help patients strengthen their pelvic floor muscles to treat urinary incontinence.
Your Transverse Abdominals Need Strengthening
Your abs are more than just six-pack muscles. “The transverse abdominis muscle is a major core stabilizer, and in a perfect world, it works together with the pelvic floor muscles,” Crouch says. “Studies show that we see a better, stronger pelvic floor muscle contraction when both these muscles work together.”
That said, “if the deep core muscles are weak, or not firing at the correct time, the pelvic floor muscles may not be working optimally either,” Crouch says.
Fix It
The goal is to build strength and control in your deep core and pelvic floor muscles, so you should perform exercises that engage both. To that end, Crouch recommends movements like glute bridges, glute marches and heel slides.
Does A Long Labor Lead To Incontinence
The modern movement of childbirth education is enormously important in helping to educate women about labor, childbirth, breastfeeding and caring for a newborn. Doctors rarely have time to talk with their patients in any detail about the steps of labor and childbirth, and childbirth educators fill this need well. Many childbirth educators also focus on avoiding medical interventions that interfere with a “natural” birth, especially cesarean section. Lamaze, the Bradley method, and many midwives and doctors encourage women to labor as long as needed and as long as the baby’s health, as monitored by the heartbeat, can tolerate labor. As a result, prolonged labor or prolonged pushing is sometimes encouraged in order to avoid a cesarean section. However, while safe for the baby, it appears that these concepts may not be in the best long-term interest of the mother. We know now that prolonged and difficult labors may lead to permanent nerve damage and weakening of the pelvic muscles and the supporting structures to the uterus, bladder and rectum. This can eventually lead to dropping of the pelvic organs or incontinence.