How Many Nights Will I Spend In The Hospital
With endoscopic surgery, you will go home the same day as the procedure.
For open bladder neck reconstruction or urinary diversion, most people will stay in the hospital for 3 to 6 days. Before they leave, they need to be able to:
- Be able to control their pain with oral medications
If you had an epidural, that will be removed before you leave.
Bladder Neck Incision And Urethrotomy
This information is designed to help you, your family and friends prepare for your surgery. It will also help you plan how to take care of yourself in the weeks following discharge from hospital.
A bladder neck incision and a urethrotomy, are operations for men who have a decreased urinary stream and problems passing urine because of a bladder neck stenosis or a urethral stricture.
Scarring can occur within the urethra for various reasons including previous surgery, catheterisation or trauma. Scarring that occurs at the neck of the bladder where it joins the prostate is known as a bladder neck stenosis and scarring within the urethra itself is called a urethral stricture. Both of these forms of scarring cause a narrowing of the urethra, much in the same way a rubber band would if it were placed around the urethra. This narrowing may cause some or all of the following symptoms:
Recommended Reading: Start Of Bladder Infection What To Do
What Causes Bladder Neck Contracture
Trauma to your body causes scar tissue to build up at the site of the trauma.
Scar tissue that builds up in tubes, like the bladder neck and the urethra, makes those tubes narrower than normal, and that can affect how well they work.
Trauma in these areas sometimes happens during complex medical procedures. These procedures include:
You May Like: How Long Is Bladder Surgery
Are There Other Related Conditions To Pelvic Adhesions
The risk of Pelvic Adhesions is increased by endometriosis, not only because of endometrial lesions but also because endometriosis surgery may cause development of scar tissue. Serious pain symptoms are often caused by the presence of Pelvic Adhesions in conjunction with other disorders like endo or irritable bowel syndrome .
Recommended Reading: Reasons For Bladder Control Loss
Management Of Post Rp Bnc With Concomitant Ppi
Post RP BNC is known to be an independent risk factor for PPI . The presence of BNC may mask the severity of the underlying urinary incontinence that is due to sphincteric deficiency . With that in mind, the BNC condition should be aggressively treated in the first instance before embarking on incontinence surgery.
Incontinence surgery should only be planned after stable vesicourethral anastomosis patency has been achieved. The rationale for this is the recurrent nature of BNC that will jeopardise the results of any incontinence surgery repair. Subsequent endoscopic interventions for BNC after incontinence surgery such as insertion of AUS carry a risk of damage to the device .
Staged and synchronous approaches to the treatment of BNC with concomitant PPI have both been reported. There is however a lack of consensus on the duration necessary for the post-surgery stabilization of BNC prior to undertaking any staged incontinence surgery. Most studies on staged intervention reported waiting times ranging from 4 to 12 weeks . Both the staged and synchronous approaches have its advantages and disadvantages .
In our center, a specialized service has been set up for PPI patients since 2004. The aim of the service was to allow easy access to investigations such as video-urodynamics and also a consultant urologist with sub-specialisation interest and training in PPI surgery. From the time of set up, our service has seen a steady rise of both regional and in-house referrals for PPI.
Also Check: My Bladder Is Always Full
The Future In Understanding Pus
Understanding the etiology of PUS may give us direction towards preventative measures. Recently the scar tissue RNA of the bladder neck contracture after RP has been compared with healthy human tissue. Alternations in the expression of molecules at this level were found. Although at its infancy, this insight may lead to further understanding of the pathogenesis of BNC, and will hopefully lead to novel treatment strategies . Other areas of research include regenerative technologies and the utilization of meshed tissue grafting from autologous cells. A recent report of twenty patients whom underwent two endoscopic injections of placental amniotic allograft following bladder neck incision was safe and 80% were recurrence free at 8 months median follow up . Further research will tell if these novel techniques will make a difference to patient care.
Adjuncts To Endoscopic Treatment
There has been an interest in adjuncts in order to improve the long term patency rate of endoscopic treatment. Involving the patient or attempting to modify the stricture pathophysiology are new strategies used to improve recurrence rate following endoscopic treatment.
Self-dilatation and calibration
In selected patients whom are compliant and motivated, one option is to perform intermittent urethral balloon dilatation and regular office review. We have found that the 18 cm Urethral Balloons dilation system useful as this is easiest for patients to traverse the PUS and inflate effectively. Patients are taught to hub the balloon at the meatus in order to ensure effective crossing of the PUS. This is inflated for 10 minutes twice per day followed by cystoscopy at 6 weeks. If at that point annularity of the VUA is seen, another transurethral incision is attempted. If not, the inflation protocol is weaned to once per day for 3 months and gradually stopped. It can occasionally take up to a year to achieve complete control and freedom from balloon dilatation. We have a select number of patients that insist on continuous self-dilatation because of the relief they have experienced and fear of re-stenosis. In those with prostate in-situ, endoscopic management with judicious resection of the urethral stenosis or channel TURP remains is an option if the high risk of severe incontinence is accepted.
Bladder neck pharmacotherapy injection
You May Like: How Deadly Is Bladder Cancer
What Do Doctors Prescribe
Doctors may prescribe pain medications or in certain cases surgery to remove the internal scars or adhesions, however these options dont always suit everyone.
Many medications cause side effects and surgery may not be welcome, natural remedies for internal scar tissue are a simple effective and safe option.
It would be unusual to go through life without getting a scar, Im sure you have had broken skin or cut yourself and your body has produced a scar in response to the injury.
You may have caused internal or external scarring, the result is that your skin looks different and you have a mark to remind you of what happened.
Scars can affect us in physical ways where our appearance isnt what it used to be, scars can affect you in a physiological way if they are noticeable.
Surgery can cause scarring and lesions to form leading to sometimes mild discomfort to sharp pain.
Doctors may tell you that its unfortunate but you will just have to live with the scars.
Luckily there is a natural alternative enzyme that can dissolve internal or external scar tissue naturally.
As you can see throughout life scars will develop either externally or internally and they can literally form anywhere in the body.
Our bodies are good at the first step in tackling inflammation following an infection, trauma or surgery, muscles nerve, bones, connective tissue and blood vessels are all involved in the protective structure of our bodies.
Treatment For Urethral Stricture
Scar tissue can result from numerous factors, but is commonly due to a straddle injury, such as falling off a bike and landing on the crossbar. Other causes leading to urethral stricture include pelvic fractures, catheter insertion, prostate surgery, benign prostate hyperplasia, radiation, a tumor, urinary tract infection, or a sexually transmitted infection .
Men with an enlarged prostate or who have had a recent catheter, one or more STIs, or urethritis due to infection are at higher risk of developing urethral stricture.
Read Also: Can A Ct Scan Miss Bladder Cancer
How Is Contracture Of The Bladder Neck Diagnosed
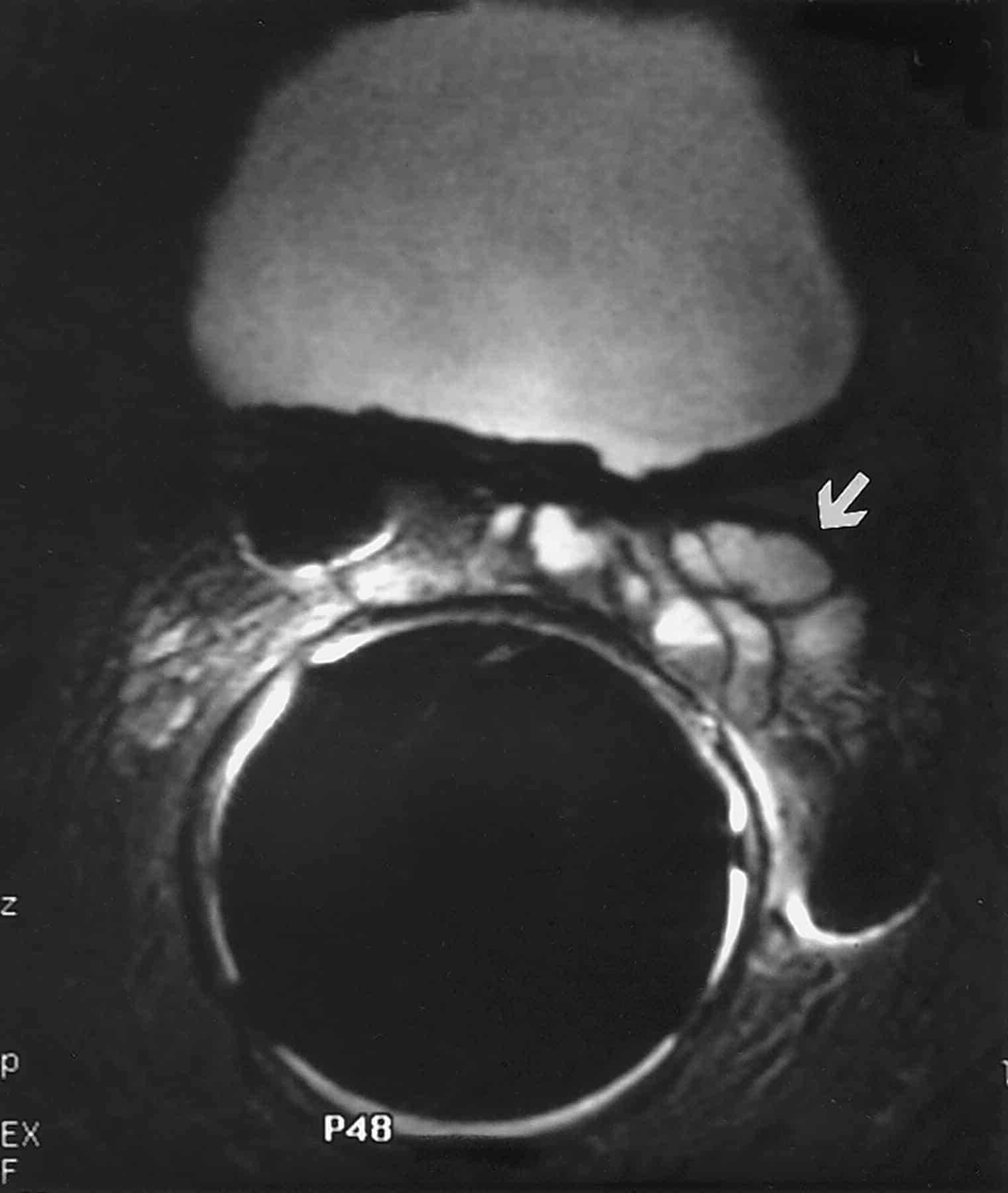
Several tests may be performed to detect whether a bladder neck contracture is present in men who are experiencing symptoms such as urinary retention or incontinence. A urologist may simply look inside with a small telescope in the office called cystoscopy. The cystoscope is a long thin instrument with a small lens and light at one end and an eyepiece at the other. After a local anesthetic is administered, the doctor passes the cystoscope through the urethra into the bladder. A liquid such as sterile water or saline may be used to fill and stretch the bladder to provide a better view. The procedure usually can be completed in two minutes.
Alternatively, an X-ray study called a cystourethrogram may be ordered to detect whether there are any structural problems in the bladder or urethra. The test requires a thin flexible tube called a urinary catheter to be inserted into the bladder through the urethra. A liquid called a contrast material is introduced into the bladder via the catheter so that X-rays may be obtained while the bladder is full. If an X-ray is taken while the patient is urinating, it is called a voiding cystourethrogram.
If a bladder neck contracture is present, there are several treatment options.
Papers Of Particular Interest Published Recently Have Been Highlighted As: Of Importance Of Major Importance
Erickson BA, McAninch JW, Eisenberg ML, Washington SL, Breyer BN. Management for prostate cancer treatment related posterior urethral and bladder neck stenosis with stents. J Urol. 2011 185:198203.
Herschorn S, Elliott S, Coburn M, Wessells H, Zinman L. SIU/ICUD consultation on urethral strictures: posterior urethral stenosis after treatment of prostate cancer. Urology. 2014 83:S5970. This article provides an excellent, comprehensive review of the work-up and management of bladder neck contractures as compiled by some of the leading authorities in the field.
Mucciardi G, Gali A, Inferrera A, Di Benedetto A, Macchione L, Mucciardi M, et al. Longitudinal observational cohort study about detrusor underactivity as a risk factor for bladder neck contracture after retropubic radical prostatectomy: preliminary results. Int Urol Nephrol. 2013 45:7216.
Redshaw JD, Broghammer JA, Smith 3rd TG, Voelzke BB, Erickson BA, McClung CD, et al. Intralesional injection of mitomycin C at transurethral incision of bladder neck contracture may offer limited benefit: TURNS study group. J Urol. 2015 193:58792. This is recent multi-institutional review of MMC injection following TUIBNC showed an overall success rate of 75% with a 7% rate of serious adverse events. This confirms, yet somewhat tempers, the initial enthusiasm associated with using adjunctive antifibrotic agents in this patient population.
Don’t Miss: Can Fibroids Cause Pressure On The Bladder
Top Stories In Urology: Robotic Bladder Neck Reconstruction Of Vesicourethral Anastomotic Stenosis After Radical Prostatectomy
You’ve saved your first item
You can find your saved items on your dashboard, in the “saved” tab.
You’ve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
You’ve subscribed to your first topic alert
What does that mean?
What Are The Symptoms Of Bladder Neck Contracture
Bladder neck contracture can make it hard for you to drain your bladder. This can cause a build-up of urine. Your doctor may refer to this build-up of urine as elevated post-void residual.
Some common symptoms of bladder neck contracture include:
- Painful urination
- Straining or pushing to pee
- Urinary retention
- Urinary tract infection
Also Check: A Catheter Is Kept In The Bladder By
Limitations Of The Study
Our study is a retrospective study and data was collected by sieving through our electronic database and patient’s case notes. The follow up of these patients was rather short. We recognised that most recurrences of BNC occur in the long term. Nevertheless, this paper still provides outcomes for an intermediate follow up period.
Patients with post RP BNC and concomitant PPI poses a challenge to the urologist. The primary goal of treatment is to achieve urethral voiding, better continence outcome and improve quality of life. Aggressive BNI as the initial management for BNC is followed by a period of observation to ascertain vesicourethral anastomosis stability is essential. In our experience, subsequent second stage incontinence surgery with implantation of an AUS or male sling have achieved satisfactory urinary continence outcomes.
Treatments For Bladder Neck Contractures
Bladder neck contractures typically form after a prior treatment for enlarged prostate, particularly laser treatments and button transurethral resection of the prostate.
Another scenario that can cause a bladder neck contracture is when someone has their prostate removed surgically and a scar forms at the site where the bladder is sewn back to the urethra.
The first treatment option in these scenarios is to perform an incision through the stricture, known as a transurethral incision of the bladder neck contracture. Some doctors then inject a small dose of chemotherapy to prevent the scar from returning. To date, there have been no trials to show that this truly makes a difference, but early reports seem promising.
In cases of radiation induced strictures, the success rate decreases with this procedure.
Advanced cases often involve a more aggressive approach. We currently perform anastomosis revision surgery, bladder augmentation surgeries or, if a patient cannot tolerate a large operation, we can place a Foley catheter to aid in bladder drainage.
Also Check: Does Overactive Bladder Go Away
What Medications Will I Need When I Go Home
Pain medications: Most people only need a few days of narcotics after they leave the hospital. These medicines are morphine-based.
Stool softeners: Anesthesia, pain, and pain medications can cause constipation. Stool softeners help keep routine bowel habits. They especially help when you are taking pain medications.
Bladder spasm medications: A Foley catheter can irritate the bladder. This can make the bladder contract and spasm.
Medications can help with this, but they can cause:
- Mental cloudiness
You will need to stop taking a bladder spasm medication 24 hours before your first follow-up visit. This will let the bladder empty well after the catheter is removed.
Antibiotics: Most people only need these at the time of surgery. They will not be given when you leave.
Posterior Urethral Stenosis After Prostate Cancer Treatment: Contemporary Options For Definitive Management
Arman A. Kahokehr, Andrew C. Peterson, Aaron C. Lentz
Division of Urology, , USA
Contributions: Conception and design: All authors Administrative support: All authors Provision of study material or patients: AA Kahokehr, AC Lentz Collection and assembly of data: AA Kahokehr Data analysis and interpretation: All authors Manuscript writing: All authors Final approval of manuscript: All authors.
Correspondence to:
Abstract: Posterior urethral stenosis is an uncommon but challenging problem following prostate cancer therapy. A review of the recent literature on the prevalence of PUS and treatment modalities used in the last decade was performed. A summative narrative of current accepted techniques in management of PUS is presented, and supplement with our own experience and algorithms.
Keywords: Prostate cancer urethra stenosis stricture
Submitted Nov 24, 2017. Accepted for publication Mar 01, 2018.
doi: 10.21037/tau.2018.04.04
Don’t Miss: Depend Adult Bladder Control Pads
Management Of Post Rp Bnc
The ideal management of post RP BNC should follow a step-wise pathway from simple to increasingly complex procedures. Urethral dilatation followed by clean intermittent catheterization has been reported to have success rates ranging from 92 to 100% . In a study by Besarani et al. , a 100% success rate with endoscopic dilatation was reported in 48 post RP patients with BNC. Nine patients required a repeat dilatation and 5 required CIC. These patients all had subsequent stabilization of their BNC without need for further intervention. In patients whom simple dilatation fails, the BNC is treated with various endoscopic treatments that include balloon dilatation and BNI at the 3 and 9 o’clock positions using a Colling’s knife or laser .
In view of the recurrent nature of BNC after treatment, methods to prevent the recurrence of BNC have been advocated. In a paper by Eltahawy et al. , 24 patients with BNC underwent BNI using Holmium laser followed by injection of triamcinolone at the incision sites. Eighty-nine percent of patients had a well-healed and patent vesicourethral anastomosis after a mean follow up of 24 months. In another study by Vanni et al. , a retrospective review was performed on patients with recurrent BNC. Intralesional mitomycin C was injected after urethrotomy. At a median follow up of 12 months, 72% of the patients had a patent bladder neck after 1 procedure, 17% had patency after 2 procedures and 1 patient achieved patency after 4 procedures.
Pain That Comes On Years Later
In some cases, pain from scar tissue is noticeable right away. In others, the pain may come on years later. Sometimes this has to do with nerves that develop after the injury itself heals. Another possibility is that a severe burn or a deep wound can eventually affect underlying bones and joints, leading to subsequent pain at the site of the scar tissue.
For internal damage, the pain may develop as a result of the scar tissue taking place of healthy tissues, such as in the case of lung and liver diseases. As your condition progresses, you may feel pain from a lack of functioning of these body parts, along with other related symptoms.
For example, scar tissue that develops in your lungs can be a result of pulmonary fibrosis. You might experience a painful cough along with shortness of breath, achy joints, and fatigue. Fibrosis or cirrhosis of the liver may not be painful at first, but the scar tissues that accumulate may cause jaundice, fluid retention, and bruising of the skin.
Despite your level of pain, treatments are available for scar tissue and its uncomfortable symptoms and appearance. Talk to your doctor about the following approaches.
Read Also: How Can I Heal My Bladder Naturally
You May Like: Back Pain Causing Bladder Problems