Top Things To Look For
Find a doctor who:
-
Is board certified and who specializes in pelvic prolapse surgery
-
Has experience treating patients with your specific condition
-
Practices at a hospital known to have high-quality outcomes in pelvic prolapse surgery or gynecologic surgery in general
-
Accepts your insurance
-
You are comfortable talking with and who fully answers your questions
Here are five steps to finding the best doctor to perform your pelvic prolapse surgery.
Can Kegel Exercises Prevent Leaking During Sex
Kegel exercises can certainly help. Women who learn to do Kegels correctly and do them regularly have less leaking during intercourse. A recent study from Norway found that women who were taught by a physical therapist the correct way of performing Kegels were more likely to have more satisfying sex than a group of women who were not properly taught these exercises. These women had fewer problems with their sex life and less discomfort with intercourse. We encourage you to do Kegel exercises on a regular basis.
Is There A Possibility Of Recurrence After Surgery
The results of a study carried out by then Radcliff John Hospital in Oxford show that 10.8 % of women undergoing pelvic organ prolapse surgery have a second or third operation within the next 11 years. The study followed a group of 2099 women that had surgery for POP between 1995 and 2005. Worth mentioning is that of the women that needed repeat surgery, 61,5% needed surgery in a different area than the site of the original operation.
Read Also: How To Get A Healthy Bladder
Why Is Vaginal Prolapse Surgery Performed
Your doctor may recommend vaginal prolapse surgery to repair or correct weaken or damaged muscles, ligaments and tissues that hold your pelvic organs in place. Problems with this support system, called the pelvic floor, can result in prolapse of the bladder , rectum , bowel , uterus, and vaginal vault . This is common in women who have had children.
Doctors generally recommend vaginal prolapse surgery when your symptoms are severe enough to interfere with your daily life.
Symptoms of vaginal prolapse include:
-
A mass or protrusion from the vagina
-
Difficulty having bowel movements
-
Pelvic or back pressure or pain
-
Urinary problems including stress incontinence or difficulty passing urine
Vaginal prolapse is associated with the following conditions:
-
Prolonged labor or having a large baby
-
Repeated childbirth or having a multiple birth, such as twins or triplets
Your doctor may only consider vaginal prolapse surgery for you if other treatment options that involve less risk of complications have been ineffective. Ask your doctor about all of your treatment options and consider getting a second opinion before deciding on vaginal prolapse surgery.
Side Effects Of Surgery
Your doctor should have an in-depth discussion with you about the risks and benefits of the 4 different types of surgery, including mesh surgery, before you decide together whether one of them could be an option.
Doctors must also keep detailed records about the type of surgery they do, including any complications you get after you have had your surgery.
You should be given a copy of this record.
Possible side effects of all 4 types of surgery, including mesh surgery, include:
- bleeding, which may require a blood transfusion
- damage to the surrounding organs, such as your bladder or bowel
- an infection â you may be given antibiotics to take during and after surgery to reduce the risk
- changes to your sex life, such as discomfort during intercourse â but this should improve over time
- vaginal discharge and bleeding
- experiencing more prolapse symptoms, which may require further surgery
- a blood clot forming in 1 of your veins, such as in your leg â you may be given medicine to help reduce this risk after surgery
If you have any of the following symptoms after your surgery, let your surgeon or a GP know as soon as possible:
- a high temperature
Read Also: What Antibiotic Do You Take For A Bladder Infection
Where Can Someone Get More Information On Prolapsed Bladders
- Urologic conditions that can occur around the time a woman goes through menopause include
- bladder control problems,
- bladder prolapse , and
- urinary tract infections.
Alyce Adams Rn Is The Kegel Queen
Alyce is known as the most sought-after kegel exercise expert around the world, helping women avoid dangerous surgery and regain health and control of their body down there. She is famous for creating the Kegel Success in Minutes a Day Program, the only complete, no-devices, safe-at-home kegel exercise program created and tested by a Registered Nurse.
The Kegel Queen busts the kegel myths that hold women back even if theyve learned from a doctor, physical therapist, or childbirth teacher. With Real Kegels That Really Work, women reverse pelvic prolapse, stop urinary incontinence, and have the most amazing sex of their lives with no annoying and inconvenient kegel devices, no drugs, and no ineffective and dangerous surgery. The Kegel Queen Program has reached over 1,382 women in 19 countries around the world.
Don’t Miss: Why Is My Bladder Constantly Leaking
What Treatment Options Are Available For Prolapse
Treatment options depend on the severity and discomfort of the prolapse. Three main choices exist for the treatment of prolapse:
- Do nothing if your prolapse is not bothersome
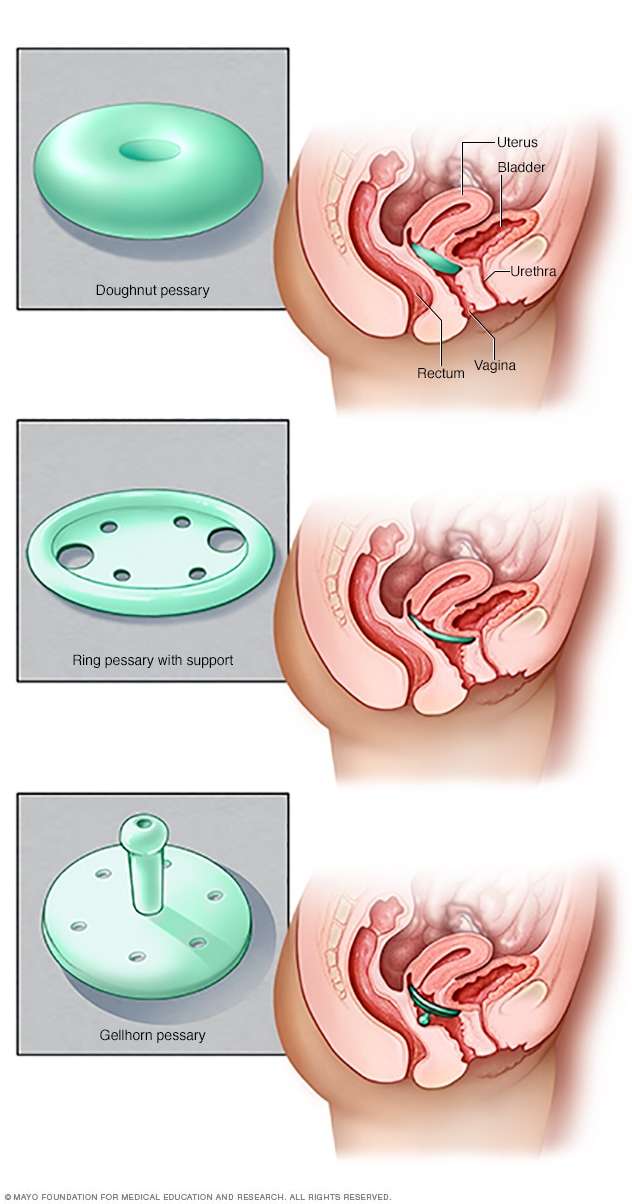
- Wear a pessary, a small plastic or silicone device placed inside the vagina to hold the organs inside your body
- Have surgery
Vaginal Surgeries: In general, vaginal-approach surgeries have a faster recovery time and cause less pain than abdominal surgeries.
Abdominal Surgeries: Abdominal-approach surgeries are performed through a larger abdominal incision, have a longer recovery time and generally cause more discomfort than vaginal surgeries. Sometimes, however, due to the patient’s anatomy or other existing conditions, the only approach can be an abdominal one.
Robotic-assisted Laparoscopic Surgery: Robotically assisted laparoscopic surgery, with the daVinci Robot, is performed through several very small, one-centimeter incisions with the use of a video camera. The advantage of this approach is faster healing time and shorter hospital stays than with a more traditional abdominal approach.
Finding The Right Doctor For Pelvic Prolapse Surgery
If you plan to have pelvic prolapse surgery, youll want a highly qualified experienced doctor to perform the procedure. While obstetrician-gynecologists commonly perform pelvic prolapse surgeries, female pelvic medicine and reconstructive surgeons specialize in these types of surgeries. How do you find the best surgeon for you? Here are important factors to keep in mind.
Read Also: Where Is The Bladder Located
What Is Bladder Prolapse Surgery With Mesh
Bladder prolapse surgery is most commonly performed through the vaginal entrance. They can also do it abdominal but doctors prefer transvaginal as it is easier, faster, and not as invasive. What they aim to do, is to settle the bladder in its original position and mobilize it. For this, they use a surgical mesh that is made of synthetic material or animal tissue.
To reinforce the vaginal wall the surgeon will insert a mesh through an incision in the anterior wall of the vagina. The vaginal wall is straightened and the bladder is then being supported.
Depending on a womans condition and the complexity of the procedure, they do bladder lift surgery with regional, or local anesthesia, or if necessary, under general anesthesia.
A good thing to know about this surgery is that most often, they release women from the hospital the same day after the surgery.
Will You Use Transvaginal Synthetic Mesh
The FDA has issued several documents on the use of reconstructive materials for pelvic floor surgery. The conclusions to date have been that transvaginal placement of these materials are of uncertain effectiveness and are associated with safety risks. In contrast, use of synthetic mesh for sacral colpopexy or for full-length retropubic or transobturator midurethral slings was considered safe and effective.
Make sure to ask your surgeon plans to use transvaginal mesh and in what way. This way you can weigh the benefits against the risks.
Read Also: New Drug For Overactive Bladder
How Do I Prepare For My Vaginal Prolapse Surgery
You are an important member of your own healthcare team. The steps you take before surgery can improve your comfort and outcome.
You can prepare for vaginal prolapse surgery by:
-
Answering all questions about your medical history, , and medications. This includes prescriptions, over-the-counter drugs, herbal treatments, and vitamins. It is a good idea to carry a current list of your medical conditions, medications, and allergies at all times.
-
Getting preoperative testing as directed. Testing will vary depending on your age, health, and specific procedure. Preoperative testing may include a , EKG , blood tests, and other tests as needed.
-
If you are overweight, talk to your doctor about losing weight before surgery through a healthy diet and exercise plan.
-
Losing excess weight before the surgery through a healthy diet and exercise plan
-
Not eating or drinking before surgery as directed. Your surgery may be cancelled if you eat or drink too close to the start of surgery because you can choke on stomach contents during anesthesia.
-
Stopping smoking as soon as possible. Even quitting for just a few days can be beneficial and help the healing process.
-
Taking or stopping medications exactly as directed. This may include not taking aspirin, ibuprofen , and blood thinners.
Questions to ask your doctor
It is also a good idea to bring a list of questions to your appointments. Questions can include:
What Is Pelvic Organ Prolapse
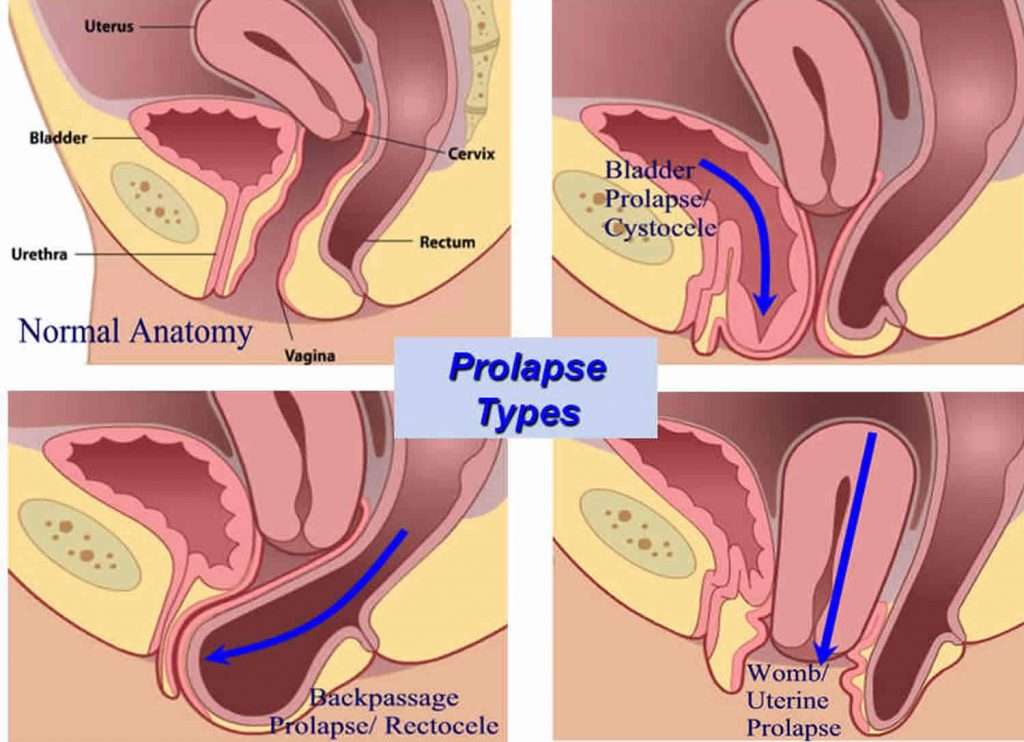
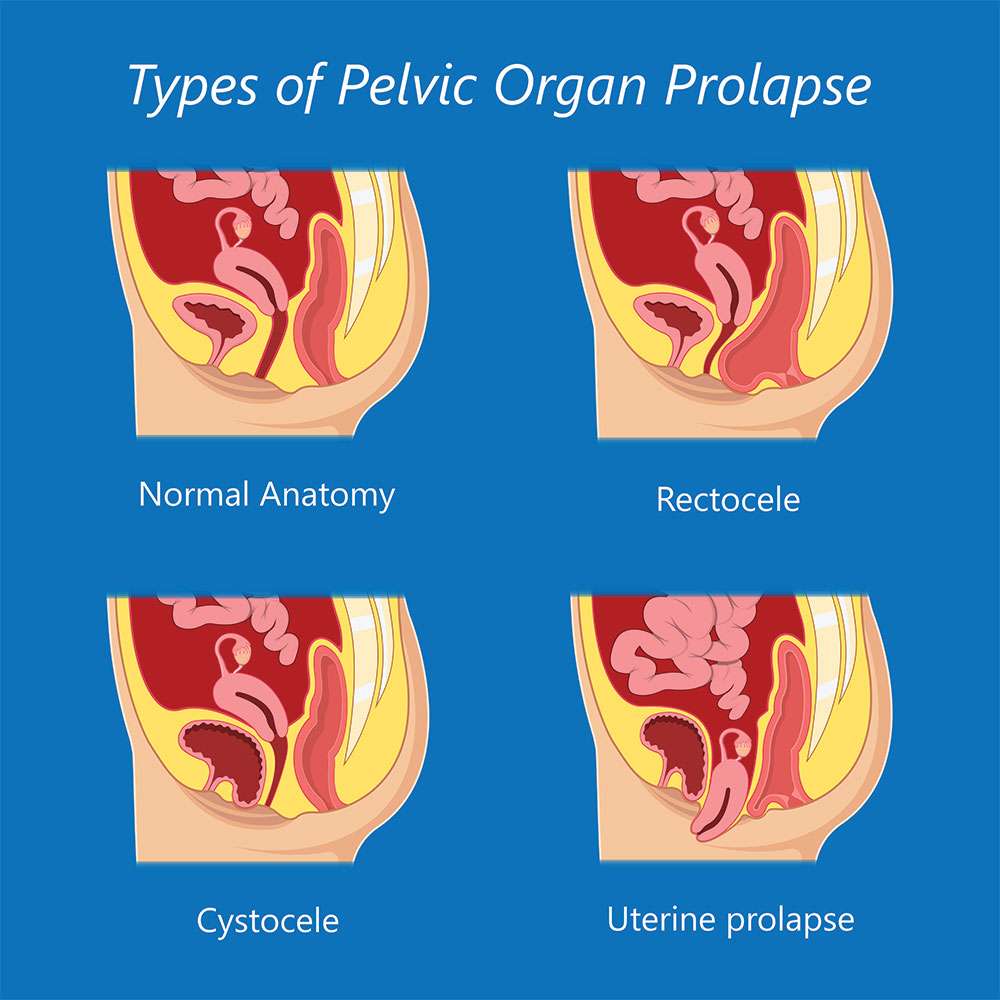
Prolapse is the bulging or dropping of the uterus, rectum or bladder into the vagina. There are several different types of pelvic organ prolapse and it is common to have more than one type at the same time. While prolapse is not considered a life threatening condition, it may cause a great deal of discomfort and distress. The various types are:
- Cystocele – when the bladder falls down into the vagina
- Uterine prolapse – when the womb drops down into the vagina
- Vaginal vault prolapse – when the vagina itself falls down
- Enterocele – when the small bowel pushes against the vagina causing a bulge
- Rectocele – when the rectum falls
Read Also: Why Can I Not Control My Bladder
How Is Vaginal Prolapse Surgery Performed
Your vaginal prolapse surgery will be performed in a hospital or surgery clinic. The procedure varies depending on the type and severity of your vaginal prolapse and other factors. Your doctor will perform vaginal prolapse surgery using one of the following approaches:
Your doctor will advise you on which procedure is best for you and how long you need to stay in the hospital or surgical center based on your diagnosis, age, medical history, general health, and possibly your personal preference. Learn about the different procedures and ask why your surgeon will use a particular type for you. Types of anesthesia that may be used
Your doctor will perform vaginal prolapse surgery using either general anesthesia or regional anesthesia.
What to expect the day of your vaginal prolapse surgery
The day of your surgery, you can generally expect to:
Should You Discuss Sexual Problems With Your Doctor
If many women have problems talking to their partners about sex, isn’t it even more difficult for them to broach the subject with their doctors? To complicate things even further, doctors are often uncomfortable about discussing sex and are rarely well trained to do so. Adding incontinence to a conversation may make both a woman and her doctor even more reluctant to pursue further discussion.
To illustrate what a significant problem this is, interviews with 324 sexually active women found that only 2 women had volunteered information about having incontinence during sex. However, when specifically asked about this symptom, 77 additional women acknowledged that they had incontinence during intercourse.
Patients and doctors need to do a better job communicating about incontinence and sexuality. If your doctor doesn’t ask about incontinence, it is important for you to bring it up if there is a problem. If your doctor seems uncomfortable with the subject, ask for a referral to someone who regularly deals with incontinence. If you are having a problem with incontinence and sexuality, more than likely you will need to bring this up as well. If your doctor is not equipped to discuss this with you, ask for the name of a knowledgeable therapist who can help.
If your doctor doesn’t know such specialists, make an effort to find someone on your own. The important thing is to get what you need. You’re not alone with this problem.
Don’t Miss: What Can You Do For A Bladder Infection
Can The Uterine Prolapse Be Treated Without Hysterectomy
A Resounding YES! Many gynecologists feel the best way to treat a falling uterus is to remove it, with a surgery called a hysterectomy, and then attach the apex of the vagina to healthy portions of the ligaments up inside the body. Other gynecologists, on the other hand, feel that hysterectomy is a major operation and should only be done if there is a condition of the uterus that requires it. Along those lines, there has been some debate among gynecologists regarding the need for hysterectomy to treat uterine prolapse.
This same uterine preserving procedure may also be accomplished though the vagina making a small entry into the abdomen behind the cervix and reattaching the ligaments to the uterus and cervix. This would be called a vaginal-uterosacral hysteropexy and leaves no abdominal scars. We have had excellent experience with this approach as well since 2000 especially if other vaginal procedures are needed at the same time for cystocele, rectocele, or vaginal narrowing.
Should You Have Surgery
If your symptoms are making your life difficult, surgery may be the answer. You need to think about a few things:
Your age. If youâre young, keep in mind that bladder prolapse can happen again. Even if you have surgery now, you may end up needing another operation down the road. If youâre older, any other health issues you have may affect your decision.
Your plans about having children. If you want more children, itâs best to hold off on surgery until you decide your family is complete.
Your general health. Surgery has some risks, such as infection, blood clots, or problems with the anesthetic. If you have a heart condition, diabetes, or breathing difficulties, any of these things could make an operation riskier. So could smoking or obesity.
Also, talk with your doctor about the chances that surgery could cause new problems. You might develop urinary incontinence — urine leaking out without your control. Sex might become uncomfortable, and you might feel pain in your pelvis.
Also Check: Small Cell Bladder Cancer Treatment
What Medications Treat A Prolapsed Bladder
Estrogen replacement therapy may be used to help the body strengthen the muscles in and around the vagina.
- Estrogen replacement therapy may be contraindicated . The ovaries stop producing estrogen naturally after menopause, and the muscles of the vagina may weaken as a result.
- In mild cases of prolapsed bladder, estrogen may be prescribed in an attempt to reverse bladder prolapse symptoms, such as vaginal weakening and incontinence. For more severe degrees of prolapse, estrogen replacement therapy may be used along with other types of treatment.
- Estrogen can be administered orally as a pill or topically as a patch or cream. The cream has very little systemic absorption and has a potent effect locally where it is applied.
- Topical administration has less risk than the oral preparations.
- The application of estrogens to the anterior vagina and urethral area may be very helpful in alleviating urinary symptoms, such as urgency and frequency, even in the face of prolapsed bladder.
How To Fix A Prolapsed Bladder Without Surgery
Kegel exercises, special exercises that strengthen the pelvic floor muscles, can help control urine leakage. Estrogen replacement therapy can also help improve muscle strength. In some cases, inserting a pessary may be enough to support the bladder.
According to the American Urological Association Foundation, the stress on the area during childbirth is a significant cause of women getting a bladder prolapse.
They estimate that one out of three women who gave birth vaginally have a stage 2 pelvic organ prolapse. Stage 2 is when the bladder pushes the vaginal wall within 1 cm of the vaginal opening. Surprisingly, many of these women are not aware of it because they have no bothersome symptoms.
Read Also: Drugs To Treat Bladder Infection
When Should I Contact A Doctor
- If you have any concern at all about any condition with your body
- If you feel a bulge or lump on the outside of your vagina
- If you have lower back pain or increased pelvic pressure that interferes with your daily activities
- If you have irregular vaginal spotting or bleeding
- If you experience frequent urinary incontinence, urinary tract infections, difficulty urinating, frequent urination or any of the symptoms listed here that interfere with your daily routine
- If sexual intercourse is painful or difficult
What Kind Of Doctor Is Best
Start with your primary care doctor. Your doctor may recommend a specialist with certification in Female Pelvic Medicine and Reproductive Surgery , such as a gynecologist, a urologist or a urogynecologist, also known as a urogyn. A urogynecologist is a medical doctor who has completed a residency in obstetrics and gynecology or urology. He or she has received additional training and experience in evaluating and treating conditions that affect the female pelvic organs, as well as the muscles and connective tissue that support them. Common problems treated by a urogynecologist include urinary incontinence or leakage, pelvic organ prolapse and overactive bladder.
You May Like: How To Take Care Of A Bladder Infection At Home