Lower Urinary Tract Symptoms
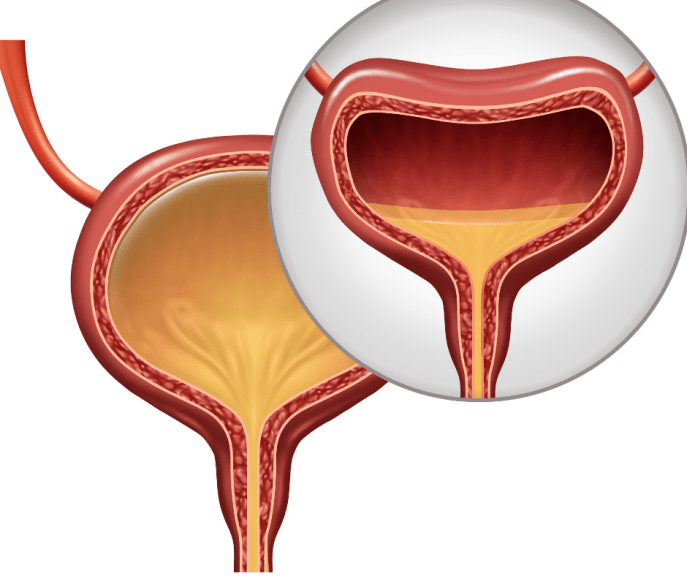
The lower urinary tract includes the bladder and the tube that urine passes through as it leaves the body .
Lower urinary tract symptoms are common as people get older.
They can include:
- problems with storing urine, such as an urgent or frequent need to pass urine or feeling like you need to go again straight after you’ve just been
- problems with passing urine, such as a slow stream of urine, straining to pass urine, or stopping and starting as you pass urine
- problems after you’ve passed urine, such as feeling that you’ve not completely emptied your bladder or passing a few drops of urine after you think you’ve finished
Experiencing LUTS can make urinary incontinence more likely.
Page last reviewed: 07 November 2019 Next review due: 07 November 2022
Overactive Bladder And Urge Urinary Incontinence
You may find yourself hurrying a lot to find a bathroom if you have an overactive bladder.
Overactive bladder is a condition in which the bladder can spasm and cause a sudden, intense and frequent urge to urinate. In some cases, these urges can lead to episodes of involuntary urine leakage, which is called urge urinary incontinence or UUI-wet. Overactive bladder contractions that send you running to the bathroom quite frequently, without any leakage is referred to as UUI-dry.
What Causes an Overactive Bladder?
The bladder is a muscle, and like all muscles it is controlled by nerves. As the bladder fills, the nerves sense the fullness and send a signal to your brain telling you that you need to urinate. Usually, your body responds to this urge to urinate so that youll have enough time to get to the bathroom. When you are at the toilet, your brain will send the message to your bladder that it is now appropriate to urinate. The message sent to the bladder tells the detrusor muscle to contract and expel the urine. When you have OAB, the nerves alert you that you need to urinate, but your ability to inhibit this urge is compromised and then the bladder starts to spasm on its own and push the urine out.
Prevention
Treatment and Management
Medical Reviewer: Karen Sasso, MSN, RN, APN, CCCN
Karen Sasso, MSN, RN, AP
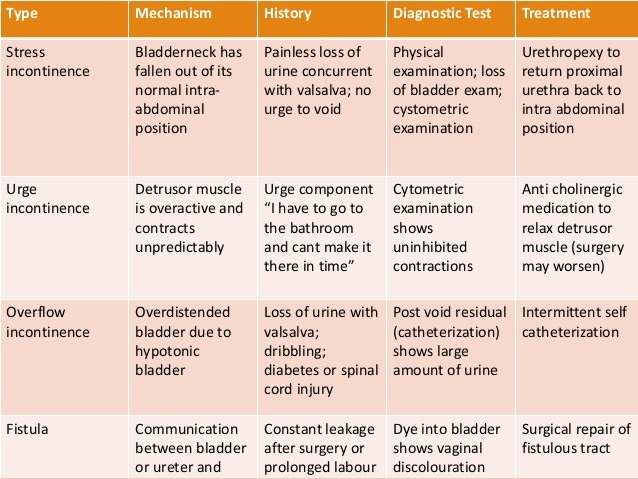
Medical Student Curriculum: Urinary Incontinence
This document was amended in October 2019 to reflect literature that was released since the original publication of this content in May 2013. This document will continue to be periodically updated to reflect the growing body of literature related to this topic.
Keywords: Urinary incontinence, urgency urinary incontinence, stress urinary incontinence, mixed urinary incontinence, overflow urinary incontinence
At the end of medical school, the medical student will be able to:
Read Also: Can Overactive Bladder Start Suddenly
Why Choose The Oab Clinic At Erlanger East
At The OAB Clinic at Erlanger East, we have urologists who are specifically trained the care of men and women with Stress Urinary Incontinence. We have the only urologists in the region who have completed fellowship training that specializes in incontinence. We have the experience, expertise and technology to care for even the most complicated patients, including those who have failed prior attempts at therapy or who have suffered a complication from a prior therapy.
Causes And Risk Factors
Aging
OAB occurs in both men and women. Its possible to have overactive bladder at any point in your life. But, its especially common in older adults. The prevalence of OAB in people younger than 50 years of age is less than 10 percent. After the age of 60, the prevalence increases to 20 to 30 percent.
The following are some of the other most common underlying causes and risk factors associated with OAB symptoms:
Nerve Damage
A healthy, normal functioning bladder holds urine until it gets full and is prompted to empty by nerve signals. However, when nerve damage occurs in the body, the muscles surrounding the urethra can be too loose. This undesirable looseness can cause someone to become incontinent. What can cause nerve damage that can then lead to bladder leakage? Some possibilities include:
- Back or pelvis surgery
- Stroke
Weak pelvic muscles
When a man or womans pelvic floor muscles are weak, bladder control issues can happen. The pelvic floor muscles are like a sling that holds up the uterus and bladder. For women, a pregnancy and childbirth can often lead to a stretching and weakening of the vital pelvic floor muscles. When pelvic floor muscles are compromised for this reason or another, the bladder can then sag out of place. The opening of the urethra also stretches and urine easily leaks out.
Menopause
Extra weight or obesity
Diuretic medications
Read Also: Can Bladder Sling Cause Uti
Wet Overactive Bladder Vs Dry Overactive Bladder: What’s The Difference
Dry type is when you have urgency where you really have to go to the bathroom and its difficult to wait, but you dont leak, and then theres wet type, where you also have the really strong urge but you cant make it to the bathroom in time and do have urine leakage, says Wu.
If you have both of those kinds, its called mixed, she adds.
Besides Prescriptions Or Pills Lifestyle Changes May Help Ease Urinary Incontinence Symptoms
Because stress incontinence is associated with higher BMI, trying to achieve a healthy weight may help improve it, says Faubion. Pelvic floor strengthening exercises are also good for helping with stress incontinence.
Its harder to know how to prevent OAB, says Wu. There does appear to be certain foods and drinks that can exacerbate symptoms caffeinated drinks, so coffee, tea, sodas, alcohol. Sometimes we think spicy or acidic foods can make OAB symptoms worse, and so avoiding or limiting those drinks and foods may help, she says.
Read Also: Hard To Urinate When Bladder Full
Different Problems Different Treatments
We offer customized treatments to address your specific needs. For example, if you have stress incontinence, we might recommend:
- Medication or hormone therapy to treat vaginal atrophy
- Vaginal pessary to support your pelvic floor or bladder
- Physical therapy
- BTL Emsella treatments
However, if you have urge incontinence, we might recommend Botox® injections or nerve stimulation to correct the nerve signals to and from your bladder. Depending on your needs, you might also find that medication to relax the bladder muscle or increase the amount of urine your bladder can hold can help reduce or eliminate your symptoms.
What Causes An Overactive Bladder
Your bladder is controlled by your nerves, as is all the other muscles in your body. In a properly functioning bladder, your nerves will sense when your bladder is full and tell your brain that you need to go to the bathroom. For most people, you will get the signal that your bladder is full you will be able to hold it until you can make it to the bathroom. Once you make it to the bathroom, you can manually signal to your bladder that it is time to release its contents, into the toilet or urinal of course.
The muscles that control your bladder is called the detrusor muscle. This is the part of your bladder that gets the message from your brain about when to release the urine. Those who suffer from the overactive bladder may receive mixed signals. Not only do the nerves tell your brain that your bladder is full, but it also has your brain tell your bladder to release its load….no matter where you happen to be. The detrusor muscle will spasm on its own which is why the condition called an overactive bladder.
The amount of pee that comes out will vary from person to person. Some people suffer from regular bouts of urinary urge incontinence, while others will simply feel the urge but remain dry. The severity can range from a few drops to a full bladder being released.
Read Also: How Can I Heal My Bladder Naturally
Urinary Problems Are Too Common In Midlife Women
When you leave your home to go out shopping or meet up with friends, do you find yourself mentally mapping out where and how fast youll be able to find a bathroom in case you suddenly and urgently need to pee? You may just chalk it up to yet another unpleasant side effect of getting older and, in a way, youd be right.
A new , the journal of The North American Menopause Society , found that women ages 45 to 54 years old are more likely to have overactive bladder syndrome.
The prevalence of overactive bladder increases with age through menopause and beyond its something thats really, really common, says Jennifer Wu, MD, MPH, a researcher and specialist in urinary incontinence and professor at the UNC School of Medicine in Chapel Hill, North Carolina.
RELATED: 12 Ways to Beat Menopausal Belly Fat
Other Types Of Incontinence
Other types of incontinence are relatively uncommon but should be considered as part of the differential diagnosis especially in patients that have not improved with traditional therapies.
- Overflow incontinence occurs due to the inability of the patient to sense a full bladder. Risk factors include bladder injury, radical pelvic surgery, spinal cord or neurologic injury, or the use of certain drugs. Treatment includes physical therapy, neuromodulation, and urinary catheterization.
- Anatomic incontinence typically occurs early in life or after surgical intervention and is due to abnormal anatomy resulting in urinary leakage. These conditions include ectopic ureter, urethral diverticulum, and urinary fistula. Treatment is typically surgery.
- Functional incontinence results from any condition including altered mental state or impaired mobility which prevents the patient from getting to the bathroom in time. Treatment may be a bedside commode or urinary catheterization.
Read Also: Bcg Used In Bladder Cancer
How Is Urinary Incontinence Diagnosed
Your health care provider may use many tools to make a diagnosis:
- A medical history, which includes asking about your symptoms. Your provider may ask you to keep a bladder diary for a few days before your appointment. The bladder diary includes how much and when you drink liquids, when and how much you urinate, and whether you leak urine.
- A physical exam, which can include a rectal exam. Women may also get a pelvic exam.
- Urine and/or blood tests
- Imaging tests
How Is Neurogenic Bladder Diagnosed
A doctor will do an exam and may order several tests of the nervous system and the bladder to diagnose neurogenic bladder: These include:
- Urodynamic studies: These bladder function tests measure how much urine the bladder can hold, the pressure within the bladder, how well urine flows, and how well the bladder empties when it is full. Special sensors may be placed on the skin near the urethra or rectum to see if the muscles and nerves in those parts of the body are working properly.
- Cystoscopy: The doctor may perform this procedure to examine the inside of the bladder and urethra with the use of a small telescope .
- X-rays
Don’t Miss: Types Of Pessaries For Bladder Prolapse
Precautions And Proper Diagnosis
The main symptoms of OAB can also occur in other health conditions like bladder cancer, urinary tract infection and enlarged prostate. Seeing blood in your urine is not a symptom of OAB.
A sudden and frequent need to urinate is common in both OAB and a UTI. How can you tell the difference between these two urinary health issues? Unlike OAB, a UTI also comes with other symptoms such as discomfort while urinating. In addition, OAB symptoms are continuous while UTI symptoms are sudden and may also include a fever.
Overflow incontinence is characterized by the involuntary release of urine from an overfull urinary bladder, often in the absence of any urge to urinate. This condition is not associated with OAB. It typically occurs in people who have a blockage of the bladder outlet, which can occur with benign prostatic hyperplasia, prostate cancer or a narrowing of the urethra. Overflow incontinence can also occur when the muscle responsible for removing urine from the bladder is too weak to empty the bladder in a normal way.
It is very important to see a doctor to ensure a proper diagnosis if you experience any changes in your urine and/or urination habits.
What Causes Neurogenic Bladder
Neurogenic bladder can be congenital . Birth defects that can cause neurogenic bladder include:
- Spina bifida : This disorder occurs when the fetus’ spine does not completely develop during the first month of pregnancy. Babies born with myelomeningocele often have paralysis or weakness that affects how the bladder works.
- Sacral agenesis: This is a condition in which parts of the lower spine are missing.
- Cerebral palsy: Cerebral palsy is a group of chronic disorders that weaken a person’s ability to control body movement and posture. These disorders result from injury to the motor areas of the brain. The problem causing cerebral palsy may occur while the infant is still in the womb or after birth. Cerebral palsy is not always found during a child’s first year of life.
Various medical conditions can cause neurogenic bladder, including the following:
- Stroke
- Heavy metal poisoning
Also Check: Overactive Bladder At Night Causes
Overactive Bladder Treatment Options
Research indicates that most people believe the symptoms of an overactive bladder are an inevitable and normal part of growing older, rather than a treatable medical problem. This couldnt be further from the truth.
In fact, fewer than half of individuals with incontinence actually consult a healthcare provider about their problem. This is unfortunate, since there are many treatments available to combat symptoms of OAB.
Even though it may feel embarrassing to talk about your condition, its important to talk to your doctor about your incontinence symptoms. Watch our short film below about the importance of speaking up about bladder leakage.
NAFC is excited to debut a short film about coming to terms with overactive bladder and incontinence. About just how challenging it can be to admit that there’s a problem. And also about how facing up to that reality can be an important first step towards drier days. Watch this short video about OAB, and about how not speaking up can create more problems than staying silent.
Risk Factors Linked To Overactive Bladder Other Urinary Problems
- The study found a significant association of OAB in women aged 45 to 54 years and postmenopausal status.
- Stress urinary incontinence symptoms were shown to increase as a result of a high body mass index and the number of times a woman has given birth.
- Other factors studied, including smoking status, history of diabetes, hysterectomy, and the use of hormone therapy , were not found to be associated with urinary incontinence.
Recommended Reading: Where Is Your Bladder Woman
What Are The Treatments For Urinary Incontinence
Treatment depends on the type and cause of your UI. You may need a combination of treatments. Your provider may first suggest self-care treatments, including:
- Lifestyle changes to reduce leaks:
- Drinking the right amount of liquid at the right time
- Being physically active
- Staying at a healthy weigh
- Avoiding constipation
- Not smoking
If these treatments do not work, your provider may suggest other options such as:
- Medicines, which can be used to
- Relax the bladder muscles, to help prevent bladder spasms
- Block nerve signals that cause urinary frequency and urgency
- In men, shrink the prostate and improve urine flow
What Is Urinary Urge Incontinence
Urinary incontinence is the actual act of losing control of your bladder. This can result in accidents or simply small amounts of moisture leaked from your genitals. Unlike OAB, which is a condition, urinary urge incontinence is a symptom caused by another condition. There are many different causes for Urinary incontinence such as due to drinking too much, a side effect of medication, or even because of a lingering urinary tract infection.
Read Also: Best Over The Counter Medication For Bladder Infection
Depression Anxiety Attention Deficit Disorder And Oab
It is probably too simplistic to view OAB with urge UI as just a myogenic or afferent disorder. Certain individuals seem predisposed to OAB. Circumstantial evidence suggests individuals with depression, anxiety, and attention deficit disorder may experience symptoms of OAB more often than the general population. Wolfe and colleagues suggested that depression, anxiety, feeding disturbances, pain, irritable bowel syndrome, fibromyalgia, and changes in voiding are associated with disturbances in brain circuits using specific neurotransmitters, in particular serotonin . Fibromyalgia and irritable bowel syndrome are conditions seen more often in patients with IC than the general population, and these conditions are associated with OAB and possibly with depression, which provides a potential link with 5-HT metabolism. Perhaps the strongest evidence for diminished 5-HT function in depressed patients is the remarkable efficacy of selective serotonin uptake inhibitors in this group of patients. In addition, neuropharmacologic evidence indicates that some forms of depression are associated with abnormalities in the promoter for the serotonin transporter gene.,