Nursing Considerations For Electrical Stimulation
Individuals who choose this method of bladder management will have to learn how to use the device. A thorough assessment for appropriateness of the procedure is essential.
Preoperative. The individual’s physical and emotional well-being will be assessed. The ability to manipulate the device and to capture urine, either in a receptacle or on the toilet, will be determined prior to treatment intervention.
Intraoperative. During the surgery, efforts will be made to ensure safety and prevent complications, such as deep vein thrombosis and pressure ulcers.
Postoperative. The focus is on maintenance of homeostasis through adequate hydration and fluid elimination. Timed voiding and fluid regulation will prevent overdistention of the bladder . This practice will afford efficient use of the sacral reflex arc and adequate emptying of the bladder. Bladder contractility will usually recover if further overdistention is prevented through temporary catheterization. The device should not be dropped on a hard surface or in water. Equipment failure and other difficulties, such as fatigue of the detrusor muscle, may arise.
Assistance required. The type of assistance needed will be determined based on the individual’s functional ability, specifically on hand function , and on the ability to transfer independently to a toilet and access the genital area. A caregiver can assist with care.
Blood Pressure Responses To Bladder Distention
In the interventional group, systolic blood pressure responses to bladder distention did not differ following ABRT-scES , nor were there significant changes at follow-up compared to baseline or post-training. Furthermore, the change in systolic blood pressure from pre-fill values to values captured at the point of maximum cystometric capacity during the study indicates that ABRT-scES did not attenuate bladder-distention associated increases in systolic blood pressure . However, concerning the usual care cohort, participants receiving ABRT-scES had significantly lower systolic blood pressure responses to bladder distention post-training compared to those in usual care . ABRT-scES sub-group training effects in relation to bladder outcomes were also evaluated. All pre-training bladder and blood pressure outcome measures between these two sub-groups were similar and there were no significant differences in these measures at pre-training, post-training, or follow-up.
How The Study Was Conducted
The researchers worked with five men who had spinal cord injuries. The men underwent 15 minutes of magnetic stimulation every week from a device thats approved by the U.S. Food and Drug Administration but is experimental when used in bladder rehabilitation.
After four sessions, the men saw a noticeable improvement in their bladder function. All five were able to urinate on their own. One participant was able to stop using his catheter completely and urinate by himself 13 years after his injury.
These improvements lasted for up to four weeks after the magnetic stimulation.
The other four men still had to use the catheter at least once daily, but that was an improvement from their previous frequency of six or more times a day.
The participants bladder capacity also increased, as did the volume of urine they were able to produce voluntarily without a catheter.
Lu says the results are promising and gave the study participants hope.
They were highly encouraged and could not wait until this strategy is available for clinical treatment, he said.
Recommended Reading: Heavy Feeling In Bladder And Frequent Urination
Electrical Stimulation And Posterior Sacral Rhizotomy
Electrical stimulation of the sacral parasympathetic nerves produces bladder contraction. Stimulation of these segmental nerves also activates somatic motor nerves causing sphincter contraction, which might be expected to prevent micturition. However, the smooth muscle of the bladder and the striated muscle of the external sphincter have different rates of contraction and relaxation and can be made to contract alternately by an intermittent pattern of stimulation, producing safe and effective voiding of the neurogenic bladder.
Electrodes are implanted surgically on the sacral nerves or nerve roots in the spinal canal and attached by subcutaneous wires to a stimulator placed under the skin of the abdomen or chest. The stimulator is powered and controlled by radio transmission from a battery-powered remote control operated by the user when voiding is desired.
Many of the complications of the neurogenic bladder are due to hyperreflexia of the detrusor and/or sphincter, and this hyperreflexia can be abolished by posterior sacral rhizotomy. The implant usually is combined with a rhizotomy to reduce reflex incontinence, increase bladder capacity and compliance, protect the upper tracts, and reduce autonomic dysreflexia. However, rhizotomy also abolishes reflex erection, reflex ejaculation, and sacral sensation, if these are present, and can reduce reflex defecation. The rhizotomy is an irreversible procedure.
- Contamination of the device.
- Transient nerve damage .
Circumventing The Problem: Urinary Diversion
Conduit urinary diversion might be a good option for management of neurogenic bladder with decreased compliance and upper tract deterioration or severe urinary incontinence. The ileal conduit was introduced by Bricker and has stood the test of time due to its relatively shorter construction time and the familiarity of urologists with this procedure. The reported outcomes were good to fair in only 50% of patients, with a 25% mortality rate, resulting mainly from urinary tract complications that occurred several years after the procedure and were attributable to recurrent UTIs.126128 However, contemporary studies have reported better results, with rates of preservation of renal function reaching 100%.129,130 However, major long-term complications have been encountered with ileal conduit diversion, including pyocystitis, stomal bleeding and irritation, metabolic acidosis, and urolithiasis. A prospective study in patients with neurogenic bladder dysfunction secondary to SCI or multiple sclerosis reported that cystectomy and ileal conduit urinary diversion improved urinary quality of life by decreasing the limitations and constraints induced by urinary disorders but had no effect on general quality of life.131
You May Like: Hernia Of The Urinary Bladder
What Does My Spinal Cord Have To Do With My Bladder
- Your brain sends and receives signals through your spinal cord. At the lowest part of your spinal cord is an area called the sacral micturition center that has nerves attached to it that go to and from the bladder. These nerves help to signal the brain when the bladder needs to be emptied. They also control the sphincter.
- For example, if you need to hold your urine until a convenient time to empty your bladder, your brain will signal the bladder not to squeeze and the sphincter to tighten so that you can wait. When it is time to release your urine, signals from your brain will then send signals down your spinal cord to squeeze the bladder and relax the sphincter. If an SCI has damaged the spinal cord, the signals from the brain to the bladder do not work correctly and you might not be able to control your urine. You might not be able to stop urine from flowing , or you might not be able to release it .
Grading The Guideline Recommendations
After panel members had drafted their sections of the guideline, each recommendation was graded according to the level of scientific evidence supporting it. The framework used by the methodology team is outlined in Table 1. It should be emphasized that these ratings, like the evidence table ratings, represent the strength of the supporting evidence, not the strength of the recommendation itself. The strength of the recommendation is indicated by the language describing the rationale.
Read Also: Homeopathic Cure For Bladder Infection
Effective Bladder Management Following An Sci
Impaired bladder function as a result of paralysis can be challenging, but there are ways to effectively manage the situation.
The most common is intermittent catheterization which involves inserting a tube connected to a bag to collect urine. This is often used in conjunction with medication, for example with botox injections, to prevent the bladder from leaking when the catheter is not in use.
Indwelling catheterization is more permanent and involves inserting the catheter which is then held in place in the bladder by a small balloon. This can be achieved either through the urethra or directly into the bladder via a small incision below the navel.
Alternatives to catheters are Valsalva and Crede voiding techniques which are appropriate if there is an issue with getting the bladder to squeeze. They both involve manually pressing or massaging the bladder to empty it.
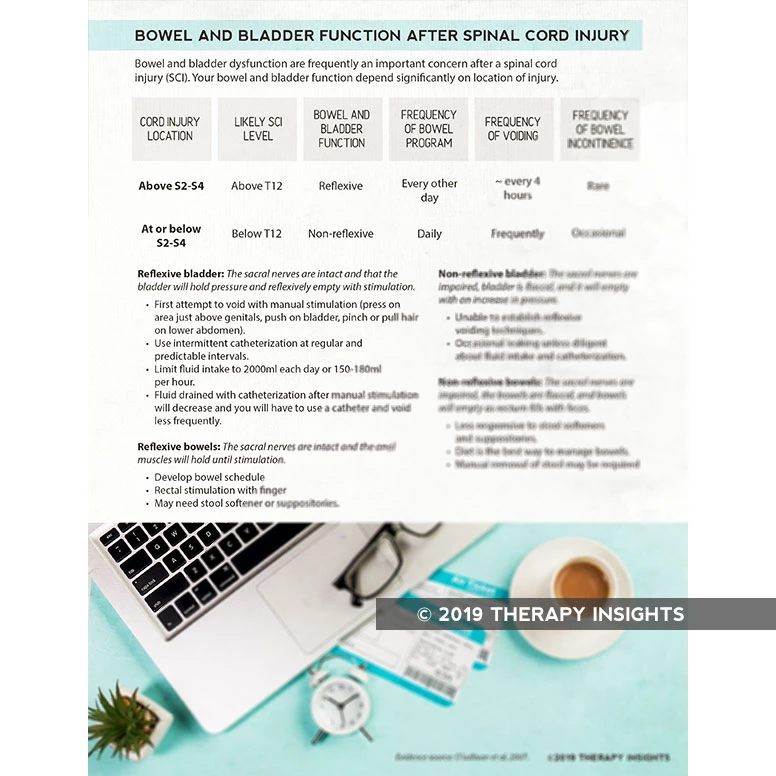
How Spinal Cord Injury Affects Bowel Control
Neurogenic bowel dysfunction refers to the loss of bowel control after an injury to the nervous system, making it common following a spinal cord injury. In those with SCI, it occurs because signals from the brain cant pass through the spinal cord damage and consequently, cannot reach the bowel muscles.
Neurogenic bowel dysfunction can be categorized into 2 general groups based on ones level of injury. Level of injury refers to the bottommost region of the spinal cord where fully intact motor control and sensation exist.
Below, well go over the main distinctions between the two classifications: T12 and above and L1 and below.
Also Check: Medication For A Weak Bladder
Lower Urinary Tract Functionemptying Phase
The emptying phase of bladder function was assessed at the end of filling or when participants indicated a strong desire to void, typically reported as fullness in the lower abdominal region. In total, 4 participants receiving ABRT-scES demonstrated the ability to voluntarily void with intent during this study. One participant was able to partially empty her bladder at all three time points and thus, a uroflow was conducted before catheter placement and filling, and flow was captured during the voiding phase once the participant reached maximum capacity. At post-training, the maximum flow rate during emptying was 2.0 ml/s . Note that the expected value for Qmax in females younger than 40 years of age is > 22.0 ml/s . Another participant partially voided post-training and at follow-up . In two other participants , one voided post-training , and the other at follow-up . All four participants identified distinct sensations of bladder fullness guiding their report of the need to empty and their intent during the void attempt. In the ABRT-scES group, there were no significant changes in total voiding efficiency from pre-training to post-training nor from post-training to follow-up . None of the individuals in the usual care group were able to void voluntarily during testing. Voiding efficiency was also unchanged in the usual care group .
Bladder Management After Spinal Cord Injury
Proper management of neurogenic bladder dysfunction is essential for optimizing quality of life after spinal cord injury.
Management interventions primarily focus on emptying the bladder before it gets too full, however the specifics of a bladder intervention program will depend on the location of the injury.
Catheterization is the most common form of bladder management after SCI. It involves inserting a narrow tube into the body to drain urine from the bladder.
There are two main types of catheterization:
Intermittent catheterization requires using a catheter every 4-6 hours to empty the bladder. If you prefer not to be connected to a catheter all the time, this method is ideal.
Indwelling catheterization involves being connected to a catheter at all times. This method brings higher risk of a UTI, and is typically only used if there is a specific reason the individual cannot perform intermittent catheterization.
Alternative bladder management interventions include:
Depending on your lifestyle and the severity of symptoms, some management interventions will be more ideal than others. Talk to your doctor to see which treatments will be best for you.
You May Like: Bcg Dose For Bladder Cancer
Nursing Considerations For Bladder Augmentation
The success of this bladder management option hinges on both objective and subjective assessments of the individual’s and caretaker’s ability to provide the necessary follow-up care.
Preoperative. The individual and his or her family are assessed to make sure they understand the procedure and the changes in lifestyle that will be necessary. The family’s ability to accommodate these changes is critical if bladder management is going to succeed .
Perioperative. Prior to surgery, the individual will receive bowel cleansing, antibiotics, a low-residue diet, adequate hydration, and confirmation of the site , as determined by the surgeon and by institution procedure and policy. If the individual will have a stoma, a wound and continence therapist or other qualified health-care provider will mark the site, the location of which will depend on body physique , old abdominal scars, hand function, and usual beltline of clothing. The individual will be evaluated both lying down and sitting up in a chair self-care is easier when the individual can see the stoma.
Postoperative. The focus is on maintenance of homeostasis through adequate hydration and fluid elimination.
Assistance required. Adequate hand function and sufficient cognitive ability are needed to insert the catheter and irrigate the augmented bladder, or a caregiver must be available to do so.
Interference with social/sexual function. Body image issues may need to be addressed if an abdominal stoma is created.
Facilitation Of Bladder Emptying

DESD in SCI patients is typically treated with antimuscarinics and catheterization. Other treatment options include external sphincterotomy, urethral stents, and intrasphincteric injection of botulinum toxin.32 Transurethral sphincterotomy might relieve autonomic dysreflexia in SCI patients with lesions above the thoracic 6 level who are unable to perform intermittent catheterization. A study of such patients reported subjective relief of autonomic dysreflexia and significant decreases in blood pressure and post-void residual urine volume for a mean of 5 years following transurethral sphincterotomy.125
Don’t Miss: Clear A Bladder Infection Without Antibiotics
How The Urinary System Works
Removing waste from the body is an important step in maintaining health. The urinary system consists of organs that complete this process. Removal of liquid waste from the body is a major function but also the urinary system is responsible for regulation of blood volume, blood pressure, and the chemical components of the body.
Elimination of liquid waste from the body begins with the kidneys. These are two organs, one on each side of the body at the back and bottom of the ribcage. Kidneys are in constant motion filtering blood. It does not matter what you are doing, the kidneys are filtering blood. The kidneys do slow their work at night due to certain hormones like vasopressin , so you do not have to wake up at night to toilet if you do not have bladder dysfunction.
On a typical day, the kidneys filter about 1,700 liters or about seven cups of blood. The waste collected from blood by the kidneys becomes urine. The kidneys are controlled by the autonomic nervous system which is the part of the nervous system that causes the body to work automatically, or without your conscious control.
The bladder has three openings, two at the top where the ureters enter to deliver urine from the kidneys and one at the base of the bladder for urine excretion. This opening for urine removal is called the urethra. The urethra is about eight inches long in males as it travels the length of the penis. In women, the urethra is about one and a half inches long.
Infections And How To Prevent Them
While urine flow and management are key, there is always the potential for problems such as urinary tract infections in individuals with a spinal cord injury. In the case of dyssynergia, where the valve at the end of the bladder fails to work properly, urine can back up to the kidneys and cause infection.
The problem with some kinds of bladder management techniques is that bacteria can easily be introduced into the urethra from the equipment used. That means there needs to be meticulous attention to hygiene when using devices like catheters. Other ways to prevent urinary tract infections include:
- Drinking plenty of water.
- Drinking cranberry juice which has been shown to prevent bacteria from spreading.
- Taking D-mannose, a sugar found in health food stores which can help reduce bacteria.
You May Like: Does Uti Cause Bladder Leakage
Nursing Considerations For Indwelling Catheters
Individuals who choose indwelling catheterization for bladder management will need education on catheter care as well as routine follow-up to detect potential complications. There are many variations to indwelling catheter technique and care. One example follows:
Catheter selection. The type of catheter to be used will depend on the individual’s needs and condition. Individuals should be asked if they are allergic to latex, though nonlatex catheters are preferred to prevent a latex allergy from developing. Most catheters have 5 ml or 30 ml balloons.
Urethral catheters. For urethral catheters #14Fr16Fr is recommended. The balloon is gently filled with 5 to 10 ml of sterile water. Silicone catheters need to have the full 10 ml placed in their balloons because they are more porous in a drained bladder. Indwelling urethral catheters are replaced every 2 to 4 weeks by the individual or a knowledgeable caregiver. The longer a catheter is left in place the greater risk of catheter encrustation. Therefore in those with a history of catheter encrustation or bladder stones, strong consideration should be given to catheter changes every 1 to 2 weeks.
Clogged catheters. If concretions cause blockage and impede drainage, a silicone catheter can be used, or 30 mls of Renacidin can be instilled daily for 2030 minutes and then allowed to drain to keep the catheter patent.
Personal care. The genital area is cleaned daily with mild soap and water.
Grading Of The Scientific Evidence
OBJECTIVE
The objective of this Metaworks, Inc., project was to provide methodologic support services for the development of clinical practice guidelines by the Consortium for Spinal Cord Medicine, sponsored by the Paralyzed Veterans of America. The main component of the project was to conduct a systematic review of the recent English language literature on bladder management of individuals with spinal cord injuries. The focus of the review was the evaluation of various types of bladder management methods, taking into consideration each one’s advantages/indications, disadvantages/contraindications, impact on prevention of upper tract and lower tract complications, and consequences on social life .
BACKGROUND
Bladder management is a crucial element in improved outcomes for individuals with spinal cord injury. The goal is to maintain and preserve a functional, infection-free genitourinary system by preventing upper and lower tract complications with a management system that is compatible with an injury-free lifestyle. The ultimate goal of therapy is to achieve and maintain adequate bladder drainage with low-pressure urine storage and voiding. There is no gold standard for methods of bladder management, so this review is intended to provide insight into each method and to help individuals with SCI choose the approach that will work best for them.
METHODOLOGY
LITERATURE SEARCH
STUDY SELECTION
Recommended Reading: How Long Does Overactive Bladder Last