What Conditions Are Treated With Bcg Treatment
BCG treatment is used to address early-stage bladder cancer. This includes bladder cancers that havent invaded your bladder wall muscle, such as carcinoma in situ bladder cancers and non-muscle invasive bladder cancers . BCG treatment isnt effective against bladder cancer that has metastasized .
Clinical trials are currently underway to explore BCG treatment for fibromyalgia and diabetes. Experts believe that BCG treatment may increase cytokines , which could potentially benefit people with these conditions. More research is needed in these areas, though.
Bcg Effect On Progression
BCG has been consistently shown to decrease the progression rates of NMIBC. A meta-analysis by Sylvester and colleagues outlined the benefits of BCG maintenance in preventing progression of NMIBC although interestingly enough this benefit was limited to CIS only . Another meta-analysis by Bohle and colleagues demonstrated statistically significant superiority of BCG with maintenance course compared to MMC maintenance for reducing the risk of progression in superficial bladder tumours .
Survival Outcomes Of The Model
The expected overall survivals were 9.55 years for the FD group and 9.61 years for the LD group. The estimated mortality in the FD group at 5, 10, and 20 years were 34.23%, 57.51% and 83.14% respectively. The corresponding values in the LD group were 34.11%, 57.17% and 82.61%, respectively. The Markov probability analysis curves, which represented the distribution of patients among Markov states, indicated a higher proportion of the no recurrence state in the LD group . The two survival curves are highly coincident as showed in Fig. .
Fig. 2
Also Check: Signs Of Bladder Infection In Toddler Girl
Bcg Versus Chemotherapy: Which Is Better
Many studies on patients with superficial transitional cell cancer of bladder have shown a lower recurrence rate with BCG as compared to intravesical chemotherapy. A meta-analysis of six trials including 585 patients on BCG versus transurethral resection of tumor alone showed that BCG provides significantly better prophylaxis of tumor recurrence in high-risk superficial TCC over TUR alone. In terms of first recurrence, a 56% reduction in the hazard was attributable to BCG. The greatest benefit was observed in high-risk groups when at least one year of maintenance therapy was used. The overall activity of BCG against papillary disease is twice that of chemotherapy in preventing recurrence. Approximately 30% absolute advantage has been noted with BCG as compared to 15% absolute advantage with chemotherapy in comparison to TUR alone. Similarly in CIS, BCG produces more than 70% complete response rate whereas the results of chemotherapy are usually around 50%.
The current consensus is to employ intravesical chemotherapy in low-to-intermediate risk patients, whereas BCG remains the first-line treatment in high-risk patients as well as in patients with prior chemotherapy failures.
Role Of Bcg In Cancer Progression
It has been proved that BCG decreases the progression of bladder cancer. In a series of 403 patients with CIS, BCG reduced the risk of progression by 35% compared with intravesical chemotherapy. In a randomized trial of 86 patients with high-risk SBC, Herr et al., demonstrated a greater delay in interval progression for BCG patients versus TUR controls. Additionally, the cystectomy rate was significantly decreased for carcinoma in situ patients treated with BCG , as was the time to cystectomy.
Recently published two meta-analyses have addressed the issue of progression in detail. A meta-analysis by Sylvester et al., which included 24 trials, 2658 patients on BCG and 2205 patients without BCG, showed that the rate of progression was 9.8% for the BCG group vs. 13.8% for the non-BCG group with a 27% reduction in relative risk of progression at a median follow-up of 2.5 years. The size of the treatment effect was similar in patients with papillary tumors and in those with CIS and there was no statistically significant difference in treatment effect for either overall survival or death due to bladder cancer.
Both these trials showed risk reduction in progression of disease only on maintenance BCG therapy. Therefore, it was concluded in both the meta-analyses that maintenance therapy, at least for one year is required to achieve reduction in cancer progression.
Read Also: Ways To Strengthen Your Bladder
Is There A Risk Of Bladder Cancer After Bcg Treatment
Like most cancers, bladder cancer can potentially return after treatment. Statistically, cancer will recur in up to 40% of people who receive BCG treatment. Its important to note, however, that even if the cancer comes back, it may not progress.
Low-grade bladder cancer usually doesnt spread to other areas of your body. But people who have low-grade bladder cancer have a higher risk of developing other low-grade cancers throughout their lifetime.
Less often, aggressive bladder cancer can develop after BCG treatment. If this happens, cystectomy is usually recommended.
Phase I Clinical Study
A phase I clinical study of âSCH721015/SCH209702â was initiated in April 2011 . The primary endpoint was safety with secondary endpoints being effective gene transfer and preliminary evidence of clinical activity at 3 months. Seventeen patients with disease recurrence following 2 cycles of BCG were enrolled in the study. Following a single treatment dose, safety was evaluated for 12 weeks and efficacy of gene transfer assessed by measuring urinary IFNα levels. Preliminary drug efficacy was assessed at 3 months.
Overall, the therapy was well tolerated with no dose limiting toxicities. Lower urinary tract symptoms mainly in the form of urgency were noted in 88% of patients, but were well managed with anticholinergics. Effective gene transfer was noted in all patients except those receiving the lowest dose. Detectable levels of IFNa were noted in patientâs urine for up to 10 days. Of the 14 patients treated with effective dosage and confirmed gene transfer , 6 experienced a CR at 3 months with 2 remaining disease-free at 29 and 39 months, respectively .
Also Check: What Is The Best Medicine For Bladder Control
Immunological Hallmarks For Clinical Response To Bcg In Bladder Cancer
- 1Translational Immunology Institute , SingHealth-DukeNUS Academic Medical Centre, Singapore, Singapore
- 2Duke-NUS Medical School, Singapore, Singapore
- 3Division of Pathology, Singapore General Hospital, Singapore, Singapore
- 4Institute of Molecular Cell Biology , Agency of Science, Technology and Research , Singapore, Singapore
- 5Department of Urology, Singapore General Hospital, Singapore, Singapore
Trained Immunity And Bladder Cancer
Trained immunity might also have a role in the effect of intravesical BCG for NMIBC as an anti-tumour mechanism. This role is not well defined data on epigenetic modifications in innate immune cells during intravesical BCG instillations are lacking. However, increased cytokine,, and chemokine, production by innate immune cells during intravesical BCG therapy is well described and might indirectly support a role for trained immunity in the mechanisms of BCG immunotherapy for NMIBC.
Also Check: What Can Cause An Overactive Bladder
Simultaneous Administration With Other Vaccines
BCG vaccine may be administered concomitantly with inactivated vaccines and live vaccines at different injection sites using separate syringes and needles. In a blinded, randomized trial, neonates experienced less pain when the BCG vaccine was administered prior to concurrent intramuscular hepatitis B vaccine. If not given concomitantly, a minimum interval of 4 weeks is recommended between administration of two live parenteral vaccines to reduce or eliminate potential interference from the vaccine given first on the vaccine given later. Live oral and nasal vaccines, like rotavirus vaccine and live attenuated influenza vaccine , may be given concomitantly with, or at any time before or after, live parenteral vaccines, such as BCG vaccine. Refer to Timing of Vaccine Administration in Part 1 for additional general information.
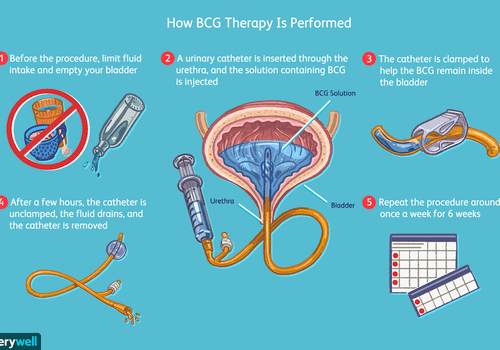
How Is Bcg Given
BCG is injected directly into the bladder using a catheter inserted into the urethra . You will receive this medicine in a clinic or hospital setting.
BCG is usually given once every week for 6 weeks, and then given every 3 to 6 months for up to 2 years. Follow your doctor’s instructions about your specific dosing schedule.
You will need to hold the medicine in your bladder as long as possible up to 2 hours. During that time you will be encouraged to reposition from your left side to right side and also you should lie upon the back and the abdomen, changing these positions every 15 minutes to maximize bladder surface exposure to the agent.
For at least 6 hours after you are treated with BCG, your urine will still contain some of the medication and the bacteria it is made from. To prevent the spread of this bacteria, use a toilet rather than a urinal, and sit on the toilet while urinating.
Before you flush the toilet, disinfect the urine with household bleach in an amount that is approximately equal to how much you have urinated. Pour the bleach into the toilet in which you urinated, let it stand for 15 minutes and then flush.
Your doctor may ask you to drink extra fluids for several hours after your BCG treatment to help flush out your bladder. Follow all instructions.
This medicine can affect the results of certain medical tests. Tell any doctor who treats you that you are using BCG.
Read Also: What Do They Give You For Bladder Infection
How Should I Prepare For Bcg Treatment For Bladder Cancer
Prior to BCG treatment, your healthcare provider will give you a list of specific guidelines to help you prepare. In general, you should avoid caffeinated beverages and diuretics for four hours before your appointment. When you arrive for your procedure, you should pee to ensure that your bladder is empty.
Risk Adjusted Surveillance And Follow

Guideline Statement 32
32. After completion of the initial evaluation and treatment of a patient with NMIBC, a clinician should perform the first surveillance cystoscopy within three to four months.
Discussion
The natural history of NMIBC is often characterized by recurrence, even for solitary, small, low-grade papillary tumors. At the time of first evaluation and treatment, none of the existent risk stratification tools or urinary biomarkers is sufficiently sensitive and specific to predict which patient will have an early tumor recurrence. Therefore, the only reliable way to know in a particular patient whether they are at risk for early recurrence is by cystoscopic visualization of the urothelium at a relatively early interval after the first treatment/resection. In addition, visualization at a relatively early interval allows the treating urologist to verify that the initial resection was complete. The Panel, therefore, felt that the first repeat cystoscopic evaluation should occur three to four months after the initial treatment and evaluation, regardless of the patient’s overall risk.
Guideline Statement 33
33. For a low-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent surveillance cystoscopy six to nine months later, and then annually thereafter surveillance after five years in the absence of recurrence should be based on shared-decision making between the patient and clinician.
Discussion
Discussion
Don’t Miss: What Causes Bladder Pain And Pressure
Intravesical Bcg Dose And Schedule
To obtain the standard dose, the BCG vaccine powdered vial is usually diluted into 50 ml of normal saline. The diluted BCG is then infused into the bladder through a urethral catheter after complete drainage of the bladder. It should be maintained in the bladder for 2 hours. BCG is administered for 2 to 4 weeks after resection to prevent the risk of systemic toxicity . The schedule of intravesical BCG treatment comprises an induction course and a maintenance course .
We have previously shown that in most patients, the maximal peripheral immune response is already observed after 4 weekly BCG instillations. However, patients not previously immunised against mycobacterial antigens may require 6 weekly instillations to achieve a maximum stimulation level . Following the induction course, several studies have reported that additional BCG treatment may decrease recurrence.
Two decades ago, Zlotta et al showed that intravesical BCG instillations induced a transient peripheral immune activation against BCG antigens. Reactivation was observed in most cases after additional BCG courses . This absence of long-lasting immune activation after a single 6-week course of BCG could be related to the increased clinical efficacy observed with BCG maintenance instillations. However, the optimum period of BCG maintenance is still controversial. The Southwest Oncology Group BCG maintenance regimen was a weekly dose for 3 weeks at 3, 6, 12, 18, 24, 30 and 36 months .
Current Alternatives To Bcg
Research on improving NMIBC therapy has mainly focused on rescue patients who do not respond to BCG therapy, since BCG is truly efficacious in the majority of patients for avoiding recurrence and progression episodes. The alternative treatment options include virus and other bacteria different from BCG as vehicles for specific tumor growth inhibition agents or immunostimulatory components, chemotherapeutic agents, new delivery options for current therapies, and systemic immunotherapies that have to be demonstrated to be efficacious in other types of cancers .
Current alternative research for nonmuscle invasive bladder cancer treatment.
Virus-Based Treatments
Bacteria-Based Treatments
Chemotherapeutic Treatments and Improved Delivery
Different strategies can improve the use of chemotherapy for treating NMIBC. The appearance of new agents, the combination of different chemotherapeutic agents, the use of hyperthermia for improving intravesical instillation, or other strategies have been considered for improving the treatment of intermediate- and high-risk NMIBC patients.
The efficacy of intravesical therapies can also be improved through delivery adaptations such as hyperthermia, electromotive drug administration or new devices.
Checkpoint Inhibitors in Nonmuscle-Invasive BC
Recommended Reading: How Long Is Bladder Surgery
Role Of Cystectomy In Nmibc
Guideline Statement 27
27. In a patient with Ta low- or intermediate-risk disease, a clinician should not perform radical cystectomy until bladder-sparing modalities have failed.
Discussion
Low-grade, noninvasive tumors very rarely metastasize, and even large-volume, multifocal cancers can usually be managed with techniques, such as staged resection. Patients with low-grade recurrences can be successfully managed with intravesical chemotherapy 225 or BCG. 177,226,227 In addition, small, multifocal recurrences despite intravesical therapy can usually be treated effectively with office fulguration, repeat TURBT or even surveillance, in select cases. 64-67
Guideline Statement 28
28. In a high-risk patient who is fit for surgery with persistent high-grade T1 disease on repeat resection, or T1 tumors with associated CIS, LVI, or variant histologies, a clinician should consider offering initial radical cystectomy.
Discussion
Guideline Statement 29
29. In a high-risk patient with persistent or recurrent disease within one year following treatment with two induction cycles of BCG or BCG maintenance, a clinician should offer radical cystectomy.
When Is Radiation Therapy Used
Radiation therapy can be used:
- As part of the treatment for some early-stage bladder cancers , after surgery that doesnt remove the whole bladder
- As the main treatment for people with earlier-stage cancers who cant have surgery or chemotherapy
- To try to avoid cystectomy
- As part of treatment for advanced bladder cancer
- To help prevent or treat symptoms caused by advanced bladder cancer
Radiation therapy is often given along with chemotherapy to help the radiation work better. This is called chemoradiation.
Don’t Miss: Prostate Cancer Spread To Bladder Neck
Transcriptomic Signature Of Post Bacillus Calmetteguerin
Figure 3 Post-Bacillus Calmette-Guerin treated tissues show upregulation in genes involved in multiple immune activation pathways. Heatmap showing all differentially expressed genes from matched tissues between Pre and 3M Post-BCG time points . Functional pathways annotated by DAVID pathway enrichment analysis of the genes enriched in Pre or 3M Post-BCG time points . Volcano plot showing DEGs in the Pre and 3M Post-BCG tissues. Genes enriched in Post-BCG time point are colored in blue while genes enriched in Pre time point are colored in red. Selected genes are highlighted. The orange line denotes the p value of 0.05. Representative dot plots showing CD8+CD27+ cells gated from CD3+CD56- T cells of isolated cells from tissues with low and high CXCL9 genes, respectively. Median value for CXCL9 genes was used as the cutoff point for dichotomisation into two groups. Proportion of CD27 expressing CD8 T cells from tissues with low CXCL9 group , and high CXCL9 group , respectively. Graph shows mean with standard deviation. *p< 0.05 by Mann-Whitney U test.
Management Of Bcg Failure
Patients failing to respond to first course of BCG can be considered for a second course of intravesical BCG and a response rate of 30-50% has been seen in this subgroup of patients. However, patients who progress despite BCG, patients with multifocal T1G3 tumors and tumors associated with CIS may be a case for immediate cystectomy.
Salvage regimens using interferon alone and combined with BCG have been employed in such situations. A complete response rate of 15-20% at one year has been seen with interferon- alone. Low-dose BCG combined with interferon- , has shown a one to two year success rate of 50-60%. A multi-institutional study showed a response rate of 42% at a median follow-up of 24 months. Intravesical gemcitabine and taxanes and device-assisted intravesical therapies have been employed in BCG failures but remain largely investigational.
Also Check: Can A Yeast Infection Feel Like A Bladder Infection
What Happens During Treatment
A urinary catheter is inserted through your urethra and into your bladder. Then the BCG solution is injected into the catheter. The catheter is clamped off so the solution stays in your bladder. Some doctors may remove the catheter at this time.
You have to hold the medicine in your bladder. Youll be instructed to lie on your back and to roll from side to side to make sure the solution reaches your entire bladder.
After about two hours, the catheter is unclamped so the fluid can be drained. If the catheter was already removed, youll be asked to empty your bladder at this time.
Search Results And Study Characteristics
Nine eligible reports were identified for qualitative evaluation ,1), but one of them was assessed as a low-quality RCT with unclear randomization method and high risk of incomplete outcome data and selective reporting.15 Authors of this article were contacted for further information but we received no reply, this study was thus discarded. The baseline characteristics of the 8 studies included were presented in Tables Tables11 and and2.2. Two studies were 3-arm trials and the 2 different doses of low-dose BCG arms were combined into a single arm by the method described before.21,22 The 8 studies included 1260 cases in the low-dose and 1199 cases in the standard dose arms. Patient demographics in the included trials are detailed in Table Table33.
Also Check: Unable To Hold Urine When Bladder Is Full