Other Ways Of Describing Bladder Cancer
In addition to its cell type, bladder cancer may be described as noninvasive, non-muscle-invasive, or muscle-invasive.
-
Noninvasive. Noninvasive bladder cancer includes noninvasive papillary carcinoma and carcinoma in situ . Noninvasive papillary carcinoma is a growth found on a small section of tissue that is easily removed. This is called stage Ta. CIS is cancer that is found only on or near the surface of the bladder, which is called stage Tis. See Stages and Grades for more information.
-
Non-muscle-invasive. Non-muscle-invasive bladder cancer typically has only grown into the lamina propria and not into muscle, also called stage I. Non-muscle-invasive cancer may also be called superficial cancer, although this term is being used less often because it may incorrectly suggest that the cancer is not serious.
-
Muscle-invasive. Muscle-invasive bladder cancer has grown into the muscle of the bladder wall and sometimes into the fatty layers or surrounding tissues or organs outside the bladder.
It is important to note that non-muscle-invasive bladder cancer has the potential of spreading into the bladder muscle or to other parts of the body. Additionally, all cell types of bladder cancer can spread beyond the bladder to other areas of the body through a process known as metastasis.
Patients May Want To Think About Taking Part In A Clinical Trial
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Urethral Cancer Development When Urine Flow Intheurethra Is Preserved
Our previous analysis of 169 male patients who underwent radical cystectomy revealed that 18 experienced subsequent urethral cancer development within five years. Risk factors for urethral cancer by multivariate analysis were: papillary cancers, multiple cancers and cancers arising in the bladder neck, prostatic urethra and prostatic tissue. Conversely, during the same period, we conducted 19 simultaneous urethrectomies with radical cystoprostatectomies in patients at higher risk for urethral recurrence. However, no remarkable histological changes were found in these patients’ urethras when examined by step-sectioning. The variety of cancerous changes observed in the 18 patients with urethral recurrence is in sharp contrast to the simultaneously resected urethras of 19 patients with almost no cancerous changes. However, in our previous series of patients, the risk of diffuse CIS could not be evaluated because, before 1986, our patients with diffuse CIS in the bladder underwent prophylactic urethrectomy at the time of cystectomy. Consequently, we re-analyzed the correlation of diffuse CIS and multifocal bladder cancers with synchronous urethral TCC.
Read Also: Bladder Sling Lawsuit Statute Of Limitations
Transitional Cell Cancer Of The Renal Pelvis And Ureter Is Also Described As Localized Regional Metastatic Or Recurrent:
Localized
The cancer is found only in the kidney.
Regional
The cancer has spread to tissues around the kidney and to nearby lymph nodes and blood vessels in the pelvis.
Metastatic
The cancer has spread to other parts of the body.
Recurrent
The cancer has recurred after it has been treated. The cancer may come back in the renal pelvis, ureter, or other parts of the body, such as the lung, liver, or bone.
How Is Bladder Cancer Diagnosed
General investigations into bladder cancer may show anaemia, especially if haematuria has been significant and prolonged. A raised alkaline phosphatase level may indicate either liver or bone involvement and in some cases the serum calcium may be raised in bone metastases. Abnormal kidney function may indicate that the bladder tumour, whether superficial or deep, is causing some blockage of the ureters where they enter the bladder.
Recommended Reading: Overactive Bladder And Back Pain
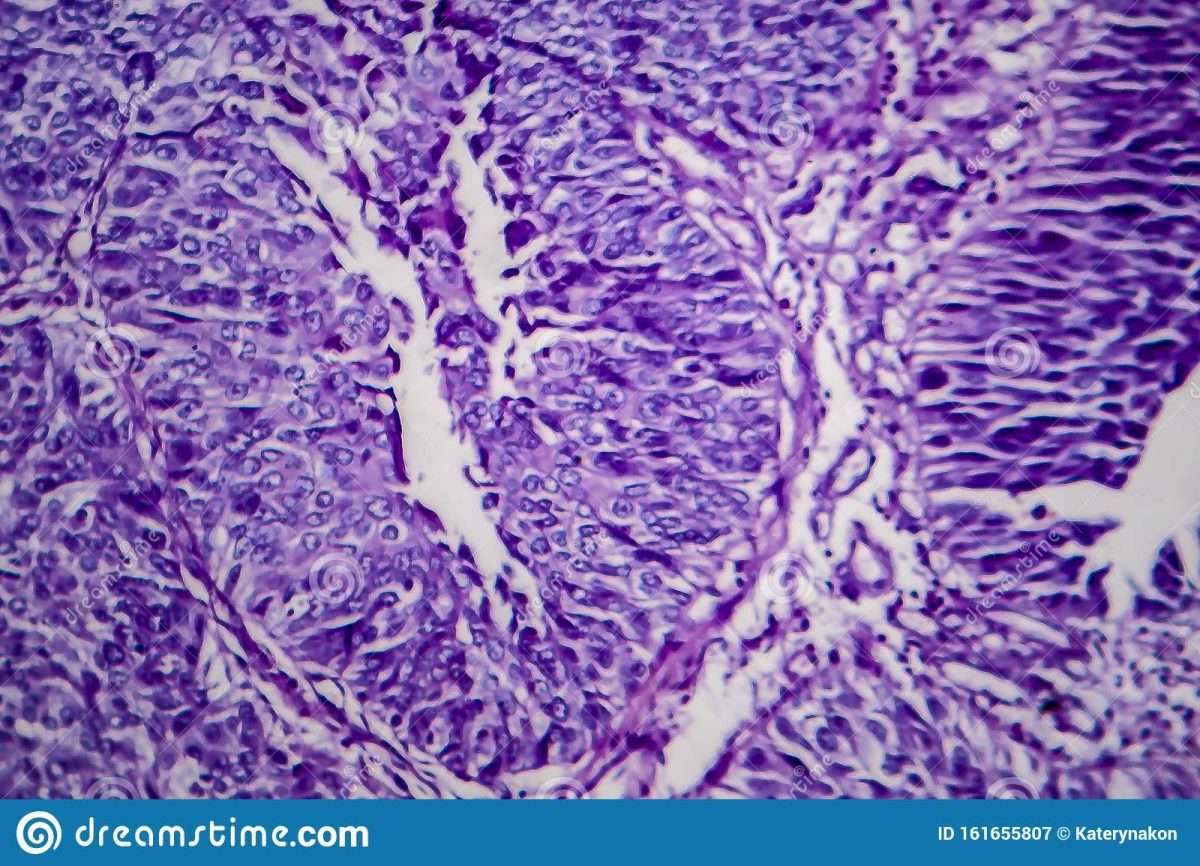
Carcinoma In Situ Of The Bladder
Carcinoma in situ of the bladder was first described in 1952 by Melicow . The diffuse nature of CIS was demonstrated in a subsequent report of 30 cases in which CIS extended from the renal pelvis to the penile urethra . Carcinoma in situ may occur as a primary disease, in association with papillary or solid tumors, or following tumor resection.
Irritative symptoms are common in patients with primary or concurrent CIS . Hematuria also is a frequent presenting feature. Urinary cytology is positive in more than 90% of patients with CIS and is an important diagnostic procedure because cystoscopic findings and even bladder biopsy may be falsely negative.
Clinical Course
The clinical course of CIS is highly variable, but overall, prior to the advent of BCG immunotherapy, 54% of patients progressed to muscle-invasive disease . Extensive, diffuse disease is considered to pose an increased risk for progression, whereas focal disease may exist for years and has a reported incidence of progression as low as 8% .
Focal CIS is the earliest stage in the evolution of invasive bladder cancer, and although its course is often protracted, regression virtually never occurs. Patients with focal disease are optimal candidates for intravesical therapy.
Radiation and Systemic Chemotherapy
Intravesical Chemotherapy
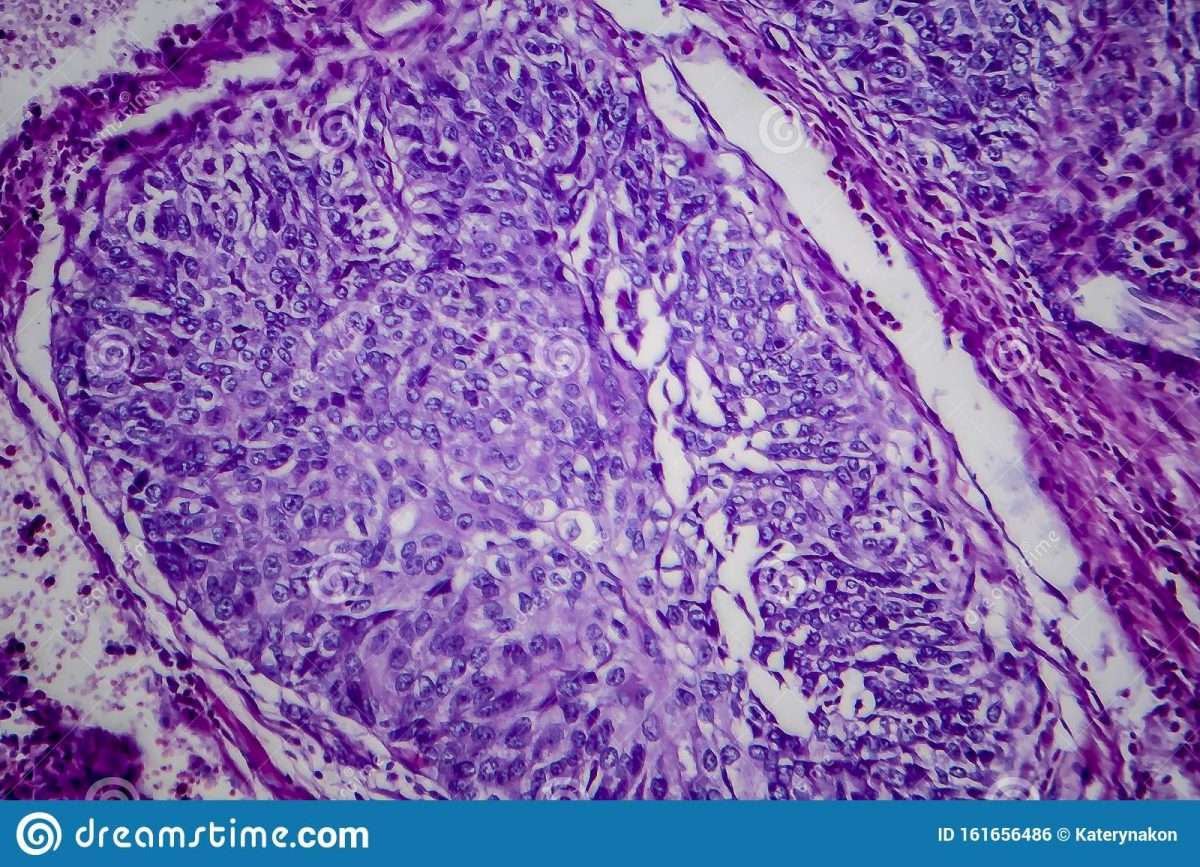
Small Cell Carcinoma Of The Bladder
This aggressive form of the disease begins in small nerve-like cells in the bladder called neuroendocrine cells. Small cell carcinoma makes up about 1 percent of bladder cancers. It is often detected at an advanced stage, after it has spread to other parts of the body. It usually requires a combination of treatments, including chemotherapy, surgery, and radiation therapy.
Read Also: How Can I Strengthen My Bladder
How Is Transitional Cell Carcinoma Of The Kidney Treated
While there are several different types of kidney cancer, transitional cell carcinoma is the most common. In general, treatment for kidney cancer begins with surgery to remove the tumor. However, depending on the size and stage of the tumor, additional treatment may be necessary.
For instance, radiation therapy or chemotherapy may be used to kill any remaining cancer cells. In some cases, immunotherapy may also be recommended. Clinical trials are ongoing to determine the best possible treatments for TCC.
However, with early detection and timely treatment, kidney cancer can be highly treatable. As a result, it is important to be aware of the symptoms and to see a doctor if anything seems unusual.
Cancer May Spread From Where It Began To Other Parts Of The Body
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if transitional cell cancer of the ureter spreads to the lung, the cancer cells in the lung are actually ureter cancer cells. The disease is metastatic cancer of the ureter, not lung cancer.
You May Like: Bladder Leakage Only At Night
Start And Spread Of Bladder Cancer
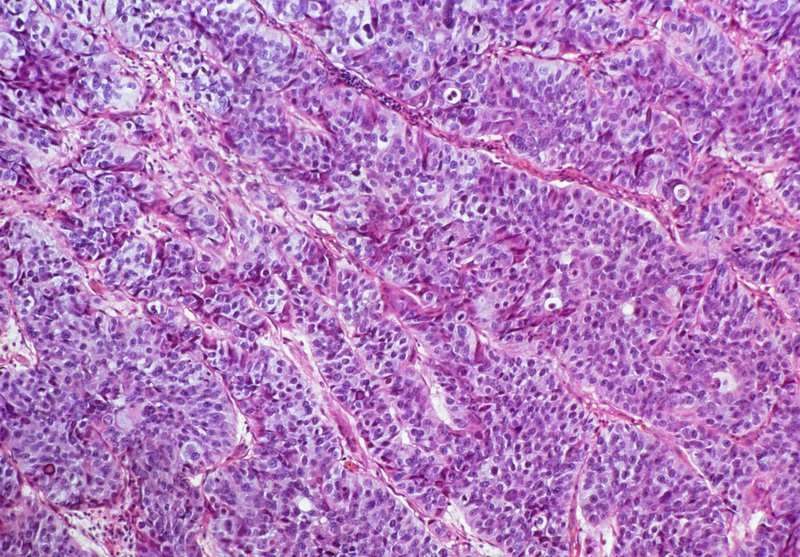
The wall of the bladder has many several layers. Each layer is made up of different kinds of cells .
Most bladder cancers start in the innermost lining of the bladder, which is called the urothelium or transitional epithelium. As the cancer grows into or through the other layers in the bladder wall, it has a higher stage, becomes more advanced, and can be harder to treat.
Over time, the cancer might grow outside the bladder and into nearby structures. It might spread to nearby lymph nodes, or to other parts of the body.
What Are The Stages Of Bladder Cancer
Bladder cancer can be either early stage or invasive .
The stages range from TA to IV . In the earliest stages , the cancer is confined to the lining of the bladder or in the connective tissue just below the lining, but has not invaded into the main muscle wall of the bladder.
Stages II to IV denote invasive cancer:
- In Stage II, cancer has spread to the muscle wall of the bladder.
- In Stage III, the cancer has spread to the fatty tissue outside the bladder muscle.
- In Stage IV, the cancer has metastasized from the bladder to the lymph nodes or to other organs or bones.
A more sophisticated and preferred staging system is known as TNM, which stands for tumor, node involvement and metastases. In this system:
- Invasive bladder tumors can range from T2 all the way to T4 .
- Lymph node involvement ranges from N0 to N3 .
- M0 means that there is no metastasis outside of the pelvis. M1 means that it has metastasized outside of the pelvis.
Read Also: Electrical Stimulation For Bladder Control
Urothelial Carcinoma The Most Common Form Of Bladder Cancer Linked To Smoking
In America, bladder cancer is the fourth most common cancer in males and the ninth most common in females. More than 57,000 males and 18,000 females get bladder cancer in the U.S. every year. Of these, nearly 17,000more than one in fourwill die as a result.
The most common type of bladder cancer is called transitional cell carcinoma . Also known as urothelial carcinoma , TCC arises from the inner lining of the urinary tract, called the transitional urothelium.
This article looks at transitional cell carcinoma, its signs and symptoms, and its causes and risk factors. It also discusses diagnosis, staging, treatment, and prevention.
Transitional Cell Carcinoma In The Kidney
| Aug 05, 2003 â 6:03 pm
My husband had a radical left nephrectomy June 30. The doctors were certain they were treating renal cell carcinoma because of the location of his tumor. Only after the pathology results come back did they realize it was transitional cell. For that he said they should have removed the entire ureter and really examined his bladder. To date, they havenât. They are now going to wait for a few months to check his bladder out until after he has his chemo. Has anyone had or known of a situation like this? He will be doing the MVAC protocol for chemo. I understand this is supposed to be a tough one and will make him really sick, is this true? I dont want to wait if it means we could have a problem.Thanks |
Recommended Reading: Air Bladder To Open Car Door
Prognosis Of Bladder Cancer
Superficial bladder cancer has an extremely good prognosis with a vast majority of people being alive and well after 5 years, with a majority of them being cured. Invasive bladder cancer however is different. If invasive bladder cancer is diagnosed early, the cure rate is still greater than 50% but if the tumour spreads to the regional lymph nodes this reduces survival to less than 50% over 5 years. Distant metastases is a bad sign as it means that the disease has spread and is obviously at a late stage in the tumours development.
The Following Stages Are Used For Transitional Cell Cancer Of The Renal Pelvis And/or Ureter:
Stage 0
In stage 0, abnormalcells are found in tissue lining the inside of the renal pelvis or ureter. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is divided into stages 0a and 0is, depending on the type of tumor:
- Stage 0a is also called noninvasive papillary carcinoma, which may look like long, thin growths that grow out from the tissue lining the inside of the renal pelvis or ureter.
- Stage 0is is also called carcinoma in situ, which is a flat tumor on the tissue lining the inside of the renal pelvis or ureter.
Stage I
In stage I, cancer has formed and has spread from the tissue lining the inside of the renal pelvis or ureter to the connective tissue layer.
Stage II
In stage II, cancer has spread to the muscle layer of the renal pelvis or ureter.
Stage III
In stage III, cancer has spread:
- from the muscle layer of the renal pelvisto fat around the renal pelvis or to tissue in the kidney or
- from the muscle layer of the ureter to fat around the ureter.
Stage IV
Recommended Reading: How To Fix Bladder Leakage Naturally
Principles Of Bcg Immunotherapy
Animal studies and subsequent extensive clinical experience have elucidated several factors of importance in optimizing the response to BCG immunotherapy:
Tumor Burden–Animal studies have demonstrated that the antitumor response to BCG is limited by tumor burden , and therefore, all visible tumor should be resected or fulgurated prior to initiation of BCG treatment.
Lowest Effective Dose–Also, optimal response requires a sufficient number of viable organisms and direct juxtaposition of BCG and tumor cells. Although a sufficient number of colony-forming units is required for response, the dose-response curve for BCG immunotherapy, like most biologic-response modifiers, is bell shaped .Dose reduction has clinical relevance because Morales et al have shown that it significantly decreases the toxicity of intravesical BCG .
Surprisingly, data collected by Pagano and associates have suggested that 75 mg of Pasteur BCG is not only less toxic but also more effective than the standard 150-mg dose . In their randomized trial involving 183 evaluable patients, low-dose Pasteur BCG resulted in a 40% improvement in 5-year disease-free status when compared with standard-dose BCG. A multicenter protocol is currently underway in the United States and Canada to evaluate reduced-dose Connaught BCG.
Signs And Symptoms Of Transitional Cell Cancer Of The Renal Pelvis And Ureter Include Blood In The Urine And Back Pain
These and other signs and symptoms may be caused by transitional cell cancer of the renal pelvis and ureter or by other conditions. There may be no signs or symptoms in the early stages. Signs and symptoms may appear as the tumor grows. Check with your doctor if you have any of the following:
- Blood in the urine.
- A pain in the back that doesn’t go away.
- Extreme tiredness.
- Weight loss with no known reason.
- Painful or frequent urination.
Recommended Reading: Can Endometriosis Affect Your Bladder
Genetic Factors In Pathogenesis
Divergent, yet interconnected and overlapping, molecular pathways are likely responsible for the development of noninvasive and invasive bladder tumors. Somatic mutations in fibroblast growth receptor3 and tumor protein p53 in tumor cells appear to be important early molecular events in the noninvasive and invasive pathways, respectively.
FGFR-3, Ras, and PIK3CA mutations occur with high frequency in noninvasive tumors, leading to upregulation of Akt and mitogen-activated protein kinase . Loss of heterozygosity on chromosome 9 is among the most frequent genetic alterations in bladder tumors and is considered an early event.
Large numbers of genomic changes have been detected using karyotyping and comparative genomic hybridization analysis in urothelial carcinoma. Numerically common are losses of 2q, 5q, 8p, 9p, 10q, 18q, and Y. Gains of 1q, 5p, 8q, and 17q are frequently present, and high-level amplifications can be found however, the target genes in the regions of amplifications have not been conclusively identified.
Alterations in the TP53 gene are noted in approximately 60% of invasive bladder cancers. Progression-free survival is significantly shorter in patients with TP53 mutations and is an independent predictor of death among patients with muscle-invasive bladder cancer.
What Is The Outlook For This Type Of Cancer
The outlook for someone diagnosed with cancer of the renal pelvis and ureter depends on a number of factors that your doctor will discuss with you. In particular, the chance of recovery is dependent on:
- Stage of the cancer. People with advanced stages of the disease will have a lower survival rate, even with treatment.
- Location of the tumor. If the tumor is located beyond the ureter and renal pelvis, the cancer may quickly metastasize to the kidney or other organs, reducing chances for survival.
- Overall kidney health. If there are underlying kidney disorders, the survival rate is lower, even with treatment.
- Cancer recurrence. Cancer recurrences have lower cure and survival rates than initial cancers.
- Metastasis. If the cancer has spread to other organs in the body, the survival rate is lower.
Its important to see your doctor for regular checkups and to let them know about any new symptoms youve developed. This helps your doctor catch potentially serious conditions in the earliest stages.
Also Check: Bladder Infection In Elderly Woman
One Type Of Standard Treatment Is Used:
Surgery
One of the following surgical procedures may be used to treat transitional cell cancer of the renal pelvis and ureter:
- Nephroureterectomy: Surgery to remove the entire kidney, the ureter, and the bladder cuff .
- Segmental resection of the ureter: A surgical procedure to remove the part of the ureter that contains cancer and some of the healthy tissue around it. The ends of the ureter are then reattached. This treatment is used when the cancer is superficial and in the lower third of the ureter only, near the bladder.
Complications Of Bcg Immunotherapy
The mechanism of action of BCG results in symptoms that previously were included in the list of adverse reactions to treatment and may have led to the erroneous conclusion that BCG is poorly tolerated. In fact, serious adverse reactions to BCG are rare, and 95% of patients tolerate BCG well .
Common Adverse Effects
Urinary frequency, mild dysuria, low-grade fever, and malaise lasting for up to 2 days and generally beginning after the third instillation are a consequence of the immune stimulation of BCG, and are associated with inflammatory cell infiltration of the bladder and cytokine and interferon release. These common symptoms respond well to symptomatic treatment with phenazopyridine, anticholinergics, antihistamines, and acetaminophen as needed.
When symptoms last more than 48 hours or do not respond to symptomatic medication, isoniazid can be given this therapy typically resolves symptoms promptly. Isoniazid treatment is continued for several days after resolution of symptoms and can be reinitiated 1 day before subsequent BCG instillations and continued for 3 days.
Major Adverse Effects
Major adverse reactions to BCG are seen in less than 1% of patients but can be life threatening.
You May Like: Cobra Medium Drain Cleaning Bladder