Foods To Incorporate If You Have Oab
-
Lean Proteins – fish, chicken breast, turkey, low fat beef and pork are good options. Eggs are also a good source of protein if youre trying to avoid meat.
-
Fiber Rich Foods – these foods are filling and can help prevent constipation, which can put extra pressure on your bladder. Almonds, oats, pears, raspberries lentils and beans are all good options when you want to add more fiber into your diet.
-
Fruits – while some fruits, especially citrus, can irritate the bladder, its still important to incorporate them into your diet. Bananas, apples, grapes, coconut and watermelon are good options for those with overactive bladder.
-
Vegetables – Leafy greens, like kale, lettuce, cucumber, squash, potatoes, broccoli, carrots, celery and bell peppers.
-
Nuts
-
Whole grains, like oats, barley, farro, and quinoa .
You may wish to eliminate all the foods on the do not eat list, then slowly reintroduce them back into your diet one by one to determine which ones your bladder finds irritating.
Types Of Urinary Incontinence
While UI in men is primarily associated with prostate enlargement, women are affected by three major types of urinary incontinence: stress incontinence, urge incontinence, and overactive bladder. Many women have a combination of two or three of these, which is referred to as mixed incontinence. To understand the types of incontinence, and their underlying causes, we must briefly review the bladder and its muscles.
The balloon-like bladder stores urine after delivery from the kidneys . The bladder is surrounded by a muscular wall. Normally, leakage from the bladder is prevented by sphincter muscles that keep the urethra the tube that carries urine from the bladder out of the body shut at either end. When we urinate, the bladder muscle contracts and the two sphincters relax, so that urine is squeezed out through the urethra. Incontinence occurs when the bladder muscle contracts suddenly and inappropriately and/or the sphincters are too weak to hold back the urine.
- Stress Incontinence is typically associated with coughing, laughing, exercise, or other movements that put pressure on the bladder. It commonly occurs as a result of physical changes following pregnancy, childbirth, and menopause that weaken the sphincters.
- Overactive Bladder is a result of the bladder muscle squeezing at the wrong time without warning and too frequently. Symptoms include high urinary frequency urinary urgency and urge incontinence.
Recommended Reading: Causes Of Repeated Bladder Infections
Do Kegel Exercises Help People With Ic
Some bladder retraining programs recommend practicing Kegel exercises as part of bladder retraining. Kegel exercises are very frequently used to treat incontinence but can actually make IC symptoms worse. This is because Kegel exercises are designed to tighten the pelvic floor muscles. But people with IC often have pelvic floor dysfunction , and their pelvic muscles are too tight. For these patients, Kegels can cause further muscle tension and muscle spasms. There are, however, other exercises and stretches that you can do to ease muscle tension and reduce spasms. Ask your healthcare provider for a referral to a physical therapist who treats people with IC and pelvic floor dysfuction.
You May Like: Tens Placement For Bladder Control
Increase The Time Between Trips
Once you’re comfortable with your voiding schedule, extend the amount of time between bathroom trips by 15 minutes. For example, if you’re urinating every hour and 15 minutes, stretch that out to an hour and a half for a week. Once you’re ready, you can shoot for an hour and 45 minutes. The goal is to get to the point where you’re urinating every three hours or so the specific timing is up to you.
What Medications Can I Use For Overactive Bladder

Your doctor may suggest trying behavioral techniques before having you use a medication to treat overactive bladder. However, medications can work very well to return normal function to the bladder. Ask your doctor about the risks and benefits of using the following commonly prescribed medications:
Anticholinergic medications
These medications control muscle spasms in the bladder:
- Oxybutynin , oxybutynin XL , oxybutynin TDDS .
- Tolterodine .
- Mirabegron .
Read Also: Why Does Cranberry Juice Help Bladder Infections
How To Strengthen Your Bladder And Urinate Less Often
This article was medically reviewed by Allison Romero, PT, DPT. Dr. Allison Romero is a Pelvic Health Specialist, Physical Therapist, and the Owner of Reclaim Pelvic Therapy in the San Francisco Bay Area. With over a decade of experience, Allison specializes in comprehensive pelvic physical therapy treatments for pelvic floor dysfunction. She holds a Bachelor of Science in Kinesiology and Exercise Science from Sonoma State University and a Doctor of Physical Therapy from the University of Southern California. Allison is a board certified Physical Therapist in California and is a member of the American Physical Therapy Association-Section on Womens Health and the International Pelvic Pain Society.There are 19 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 963,372 times.
Key Points For Bladder Control
These tips and techniques can help reduce bladder urgency and urinary frequency and help to bladder control training. Its simply a matter of testing which techniques work best for you, particularly when combined with strong pelvic floor muscle contractions.
When incorporated into an effective bladder control training program, these bladder calming strategies and bladder control exercises can help to reduce and overcome bladder control problems.
Important: Bladder problems such as urinary urgency and/or urinary frequency can be caused by or associated with medical problems. If you experience urinary urgency or urinary frequency you are advised to speak with your medical practitioner about your condition before commencing bladder control training.
Also Check: Uncontrollable Bladder After Giving Birth
Will The Type Of Treatment Youre On Affect Your Diet
There are many medications that are available to treat overactive bladder. Most of these medications work by relaxing the bladder muscles to prevent bladder spasms. They can, however, have side effects, and those may in turn affect what you eat and drink.
A common side effect of OAB medications is dry mouth. This may cause you to drink more water than normal, which may then increase your oab symptoms. Keep an eye on how much water youre consuming, and try to take small sips throughout the day to avoid overloading your bladder.
Constipation is another potential side effect of OAB. Constipation places increased pressure on your bladder – a problem in general, but especially when you have overactive bladder. Patients who experience constipation can help relieve this symptom by eating fiber rich foods, such as the ones listed above.
Talk to your doctor about any potential side effects of OAB medications you may be taking or considering.
OAB can be a frustrating condition, and one that can be tricky to treat. Talk to your doctor about the diet changes you can make to improve your symptoms, and incorporate some of the tips above. With a few small tweaks to what you eat, you may soon be on to drier days.
Normal Female Bladder Function
The adult bladder is a hollow organ with a muscular wall. Urine enters the bladder from two ureters which run from the kidney to the bladder. Urine is expelled from the bladder to the exterior via the urethra.
The detrusor muscle of the bladder wall is specifically designed to be able to store urine without increasing bladder pressure. The bladder acts as a reservoir relaxing to receive urine during the filling phase and only contracts to evacuate during the voiding phase.
The urethra acts reciprocally to contract during the filling phase to keep urine in the bladder and relaxing during voiding to allow for micturition. At rest the urethra is closed and the walls coapt against each other to form a seal that acts to keep urine in the bladder. Under situations of increased abdominal pressure contraction of the pelvic floor muscles and muscles around the urethra act to offer increased urethral resistance and maintain continence.
This video explains the pathophysiology of the overactive bladder. Bladder overactivity is a common problem affecting nearly 1 in 7 seven women. The aim of the video is to understand what is happening when the bladder is overactive. When you understand the cause you are more likely to be compliant with the treatments.
Recommended Reading: Does Azo Bladder Control Help With Incontinence
How To Overcome Bladder Weakness
If you want to go about your day worry-free, there are pelvic floor muscle exercises and yoga poses that can help you treat bladder weakness. Studies have shown that these exercises can restore the strength of the weakened muscles in the pelvic floor and bladder, which may disrupt normal urinary function in adults.i To strengthen these muscles, you need to learn how to relax them.ii
In this article, we will show you to how to perform 5 beginner-friendly bladder weakness exercises, including some yoga poses.
Is Bladder Training Right For Me
The decision to try bladder training depends on what’s causing the problem. Bladder control training is typically used to treat urinary incontinence, the involuntary loss of urine. Incontinence is most common in women, especially after childbirth and menopause. Different types of urinary incontinence exist, including:
- Stress incontinence: Sudden pressure on your abdomen causes you to accidentally lose urine.
- Urge incontinence: You feel a sudden, strong urge to go to the bathroom because your bladder contracts even when it’s not full. You may not always be able to reach the toilet in time.
- Mixed incontinence: A combination of stress and urge incontinence.
- Overflow incontinence: A problem emptying the bladder completely that leads to urine leakage.
Bladder retraining may also be used to treat bed-wetting in children.
You May Like: How Long Can A Bladder Infection Last
Why Retrain The Bladder
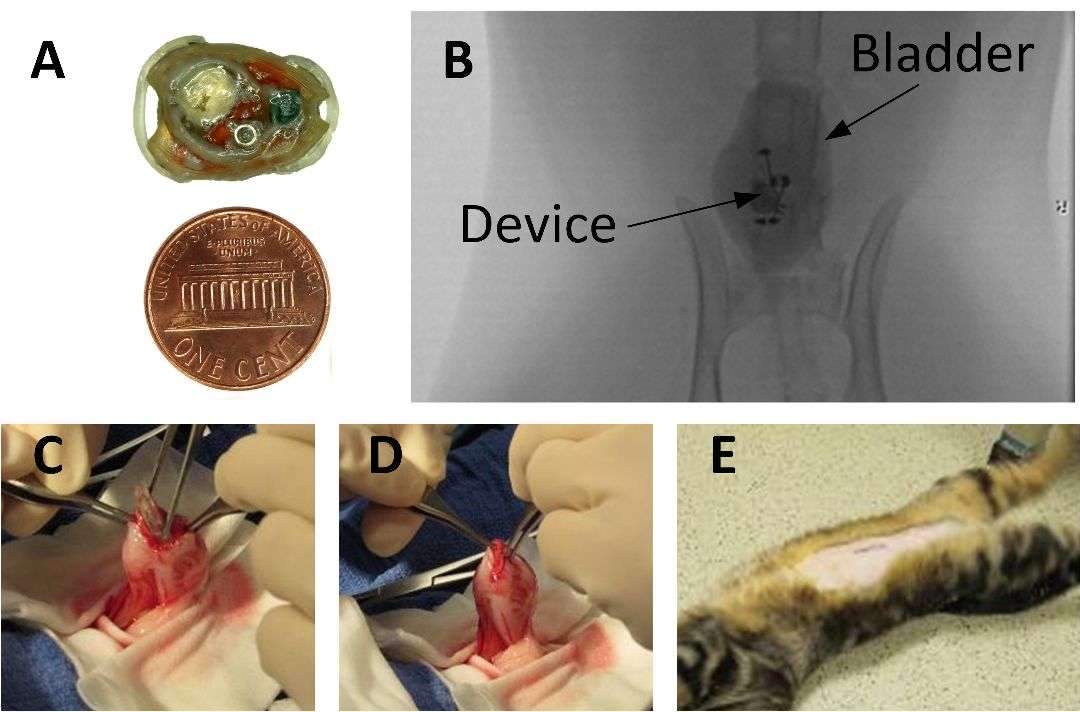
Whenever you experience pain or urgency in the bladder, the normal impulse is to urinate to stop the symptom. This establishes a pattern of frequent voiding, which can be difficult to reverse, even after your pain is controlled. To retrain your bladder, you will follow a series of simple steps to achieve longer and longer periods between urinations. Increasing bladder capacity is the objective, meaning that you will be able to hold more urine in your bladder and will not need to go as often.
Bladder Training Tips To Reduce Bathroom Trips
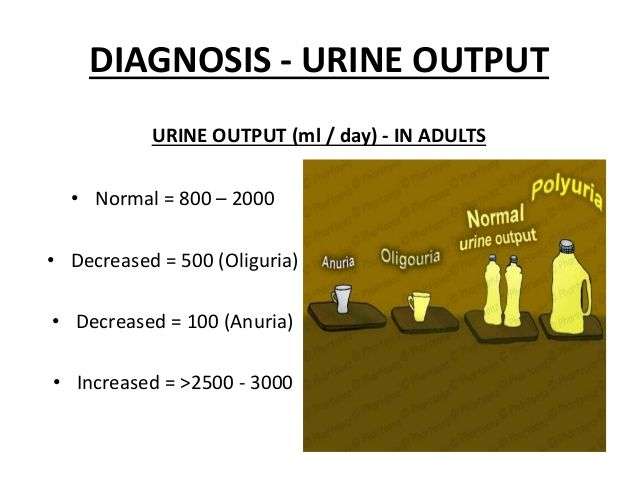
It’s important to go the bathroom when you need to. “Holding it” can actually stretch your bladder, making it difficult to empty it completely. But there’s such a thing as going too often. An overactive bladder contracts abnormally, triggering the urge to urinate too often. This can lead to urge incontinence, which occurs when you suddenly feel a strong urge to urinate but don’t make it to the bathroom in time.The good news is that bladder training can help. Here’s how.
Also Check: Diet After Bladder Cancer Surgery
Bladder Training As A Behavioral Treatment For Children
Sanja Jelic, MD is board-certified in pulmonary disease, sleep medicine, critical care medicine, and internal medicine. She is an assistant professor and attending physician at Columbia University College of Physicians and Surgeons in New York, NY.
Bladder training is a behavioral treatment that may be effective in eliminating bedwetting among children. Bladder training seeks to increase the capacity of the bladder and the strength of the muscles used to retain urine in children and reduce the chance of accidents overnight. Learn how bladder training can be an effective bedwetting treatment in kids who still have problems.
What To Expect From Your Doctor
In terms of an assessment, your nurse or doctor will ask you about your general health and in particular, about your OAB problem. You may be examined orally and internally, and you might be asked to give a urine sample to see if you have any obvious problems.
As part of your treatment programme, you may be asked to keep a bladder diary for roughly 3 days, which typically involves making a record of the time of each time you pass urine and how much urine was passed.
You may also be asked to take a flow test, and in some cases a post-flow ultrasound test. This involves using a special machine which checks whether you completely empty your bladder and also measures how strong your flow is.
Here is a short list of possible questions your doctor may ask and the tests they may ask you to complete:
- An overview of your medical history.
- A physical examination, which could include a rectal exam and a pelvic exam in women.
Also Check: Where Do You Feel Bladder Spasms
Pelvic Floor Exercise Daily Workout
This Physical Therapist guided workout helps you:
- Strengthen your pelvic floor muscles
- Improve bladder control
- Improve bowel control and emptying
- Reduce prolapse symptoms
- Recover after pelvic floor surgery
- Prepare and recover from gynaecological surgery
- Maintain pelvic floor strength during pregnancy
- Recover after pregnancy and childbirth
Mistake : Going Too Often
One more trip to the bathroom before rushing out the door may seem like smart planning, but it can backfire. The danger is that you can end up training the bladder to respond to small volumes, which can lead to overactive bladder symptomsthe sensation of needing to urinate more frequently than is normal, explains Dr. Rickey.
Going too often at night can also be a problem for men who then cant fall back to sleep, says Stanton Honig, MD, director of Male Urology, adding that this condition, called nocturia, can affect quality of life. If this is bothersome to patients, there are treatment for it, says Dr. Honig.
Other problems can also cause increased urinary frequency, such as an infection along the urinary tract. Therefore, if you find that you need to visit the bathroom far more often than you used to, talk to your primary care physician or urologist. You may need a urinalysis to rule out a UTI, as well as to check for blood in the urine , which can happen to a small number of people with an overactive bladder who have a bladder tumor, Dr. Brito says. Blood in the urine is never normal and usually requires further testing to determine its cause, Dr. Brito says.
Read Also: Can A Bladder Infection Turn Into A Kidney Infection
The Bladder Retraining Technique
Before you begin bladder control training, your doctor will probably ask you to keep a diary. In your bathroom diary, you’ll write down every time you have the urge to go, as well as when you leak. Using your diary as a guide, you’ll use the following techniques to help you gain more control over urination.
Schedule bathroom visits. Determine how often you’re going to the bathroom based on your diary entries. Then add about 15 minutes to that time. For example, if you’re going to the bathroom every hour, schedule bathroom visits at every one hour, 15 minutes. Use the bathroom at each scheduled visit, regardless of whether you actually feel the urge to go. Gradually increase the amount of time between bathroom breaks.
Delay urination. When you feel the urge to urinate, hold it for another five minutes or so. Then gradually increase the amount of time by 10 minutes, until you can last for at least three to four hours without having to go to the bathroom. If you’re feeling a strong need to go, try distracting yourself by counting backwards from 100 to one or practicing relaxation techniques such as deep breathing. When you just can’t hold it any longer, use the bathroom, but go again at your next scheduled void time to stay on your bladder retraining schedule.
To improve your success with bladder retraining, you can also try these tips:
Natural Supplements You Can Take At Home
While there have been very few scientific studies on herbal remedies as an option for overactive bladder treatment, some remedies have shown promising results for some people.
Studies from Japan have shown improvements in urgency, leakage and a reduction in night-time urination using a herbal remedy known as Gosha-jinki-gan. Also, the buchu plant from South Africa is thought to nourish the bladder tissue and fights inflammation which can lead to infections and incontinence.
There are also plenty of common herbs that may help with symptoms, including:
- Corn silk
- Capsaicin
- Ganoderma lucidum
Remember to consult your doctor first before adding any of these herbal remedies into your overactive bladder management plan.
Also Check: How Does Botox Help Bladder Control
Contract Your Pelvic Floor Muscles
Research has shown that when the pelvic floor muscles contract, the bladder muscle relaxes.
You can put this research to good use reduce urgency and unwanted leakage. When you notice an inappropriate bladder sensation, try to establish a habit of contracting your pelvic floor muscles. This can work well to assist bladder training, especially when combined with any one or a number of the following bladder control training techniques.
What Causes Overactive Bladder
An overactive bladder can be caused by several things, or even a combination of causes. Some possible causes can include:
- Weak pelvic muscles: Pregnancy and childbirth can cause your pelvic muscles to stretch and weaken. This can cause the bladder to sag out of its normal position. All of these factors can cause leakage.
- Nerve damage: Sometimes signals are sent to the brain and bladder to empty at the wrong time. Trauma and diseases can cause this to happen. These can include:
- Pelvic or back surgery.
- Stroke.
Often, there may be no specific explanation for why this is occurring.
Also Check: Women’s Bladder Leakage Protection