Neoadjuvant Chemotherapy For Bladder Cancer
Seth P. Lerner, MDOncology
Occult distant micrometastasis at the time of radical cystectomy leads predominantly to distant failures in patients with locally advanced muscle-invasive transitional cell carcinoma of the bladder. Cisplatin-based combination chemotherapy enhances survival in patients with metastatic urothelial cancer. Studies evaluating adjuvant chemotherapy have been limited by inadequate statistical power. However, randomized clinical trials have demonstrated a survival benefit for neoadjvuant cisplatin-based combination chemotherapy, which should be considered a standard of care. In addition, neoadjuvant therapy may assist in the rapid development of novel systemic therapy regimens, since pathologic complete remission appears to be a powerful prognostic factor for long-term outcomes. Patients who are either unfit for or refuse radical cystectomy may benefit from neoadjuvant chemotherapy with or without radiation to enable bladder preservation.
Risk Factors for Recurrence Following Radical Cystectomy
A postoperative nomogram was developed by the International Bladder Cancer Nomogram Consortium, based on > 9,000 postoperative patients and including age, sex, time from diagnosis to surgery, pathologic tumor stage and grade, tumor histologic subtype, and regional lymph node status. The predictive accuracy of the nomogram was significantly better than standard staging or standard pathologic subgroupings .
Systemic Chemotherapy for Metastatic Urothelial Cancer
The Current Neoadjuvant Scenario In Uc
Historically, the standard of care for MIBC patients who are eligible has been platinum-based chemotherapy. For patients receiving three cycles of neoadjuvant methotrexate, vinblastine, doxorubicin, and cisplatin in stage T2-T4aN0 muscle-invasive bladder, pathologic complete response , defined as the absence of viable tumor in the resection specimen, has been reported in 38% of cases. Some of the significant adverse events for this chemotherapy regimen were grade 4 granulocytopenia and gastrointestinal toxicity, such as grade 3 nausea or vomiting, stomatitis, diarrhea, or constipation .15
Gemcitabine plus cisplatin the most widely used regimen in neoadjuvant MIBC has not been studied prospectively in the neoadjuvant setting. However, retrospective results for 935 patients across 19 centers for patients with clinical cT2-4aN0M0 showed a pCR of 23.9% for GC, compared with 24.5% for MVAC, with no difference on multivariable analysis for these regimens.16
When Is Chemotherapy Used
Systemic chemo can be used :
- Before surgery to try to shrink a tumor so that it’s easier to remove and to help lower the chance the cancer will come back. Giving chemo before surgery is called neoadjuvant therapy.
- After surgery . This is called adjuvant therapy. The goal of adjuvant therapy is to kill any cancer cells that may remain after other treatments. This can lower the chance that the cancer will come back later.
- In people getting radiation therapy, to help the radiation work better.
- As the main treatment for bladder cancers that have spread to distant parts of the body.
Don’t Miss: Will Z Pack Cure Bladder Infection
Immunotherapy In Advanced Uc
PD-1/PD-L1 inhibitors in UC were first studied in patients with unresectable or metastatic disease. Significant activity was demonstrated for all the previously mentioned drugs.
Pembrolizumab was studied in first-line setting in 370 patients with an overall objective response rate of 24% and complete response of 5%. Subgroup analysis using the PD-L1 combined positive score , defined as the percentage of cells expressing PD-L1 in a tumor biopsy, showed an ORR of 39% in those with CPS> 10%, 20% for CPS between 1% and 10%, and 11% for those with CPS scores below 1%.9
Similarly, Atezolizumab was studied in 486 patients in the second-line setting, showing an overall ORR of 15%, while CR was reported in 5% of patients. Subgroup analysis by the percentage of PD-L1-positive immune cells in the tumor microenvironment IC0 , IC1 , and IC2/3 , showed an ORR of 8%, 10%, and 26% respectively.10
Additionally, in a phase I/II study including 191 patients, Durvalumab showed an ORR of 17.8%. The rate was 27.6% for patients with high PD-L1 expression and 5.1% for those with low or negative PD-L1 expression . CR for Durvalumab was seen in 3.7% of the overall studied population.11
Another immune checkpoint inhibitor , Nivolumab, was assessed in 265 patients in the second-line setting, after platinum-based chemotherapy, showing an overall ORR of 19.6% and CR in 2% of patients. Subgroup analysis by PD-L1 expression 5%, > 1% and < 1% indicated an ORR of 28.4%, 23.8% and 16.1%, respectively.12
Gemcitabine/cisplatin Is Alternative Nac Regimen While Gene Expression And Immunotherapy May Come Into Play
There is plenty of retrospective comparative effectiveness data suggesting that gemcitabine/cisplatin may substitute for MVAC as NAC regimen. However, no robust prospective data exists in the NAC setting. The SWOG 1314 trial, utilizing four cycles of either dose-dense MVAC or gemcitabine/cisplatin , may help us select the proper regimen for an individual patient in the future, since it evaluates the predictive value of a gene expression score generated at the time of transurethral resection of bladder tumor . It is worth noting that dose-dense MVAC given every two weeks has been replacing conventional MVAC due to lower toxicity and shorter duration of chemotherapy this NAC regimen is given for three to four cycles. Gemcitabine/cisplatin is typically given on a 21-day cycle, over three to four cycles .
Interestingly, there are many novel clinical trials, e.g. with neoadjuvant immunotherapy and chemotherapy combination or immunotherapy alone that may generate potentially more treatment options for bladder cancer patients. We designed such a trial, which may open in the near future at Cleveland Clinic.
Additional data suggest the predictive value of DNA repair gene mutations in response to NAC, and clinical trials are being designed to validate prospectively the utility of those findings. Referrals for appropriate clinical trials are critical for the development of new safe and effective therapies.
Recommended Reading: Exercises To Help Bladder Leakage
Surgery And Radiation Therapy
Endoscopic TURBT is the first-line treatment to diagnose, stage, and treat visible tumors. TURBT is not effective for CIS, because the disease is often so diffuse and difficult to visualize that complete surgical removal may not be feasible. It is critically important to surgically remove all nonmuscle-invasive disease prior to beginning intravesical therapy. When a combination of papillary tumor and CIS is present, the papillary tumor is removed before treatment of the CIS is initiated.
The EAU guidelines recommend the use of fluorescence-guided resection, as it is more sensitive than conventional white-light cystoscopy for detection of tumors. The added detection rate with fluorescence-guided cystoscopy is 20% for all tumors and 23% for CIS. The FDA has approved the use of blue-light cystoscopy with 5-aminolevulinic acid in patients suspected or known to have nonmuscle-invasive bladder cancer on the basis of prior cystoscopy.
As many as 20% of patients initially diagnosed with CIS may have unrecognized invasion beyond the lamina propria. Thus, they may not respond to intravesical therapy. These patients are candidates for radical cystectomy or radiation therapy and/or chemotherapy. Radiation therapy with or without chemotherapy is of limited benefit in patients with pure CIS but can be useful in some patients with muscle-invasive transitional cell carcinoma .
Lymph node dissection
Small cell carcinoma
Adenocarcinoma and lymphoma
Squamous cell carcinoma
Which Chemo Drugs Are Used To Treat Bladder Cancer
Chemo drugs may be used alone or in combination, depending on what theyre being used for, a persons overall health, and other factors.
When chemo is given with radiation, the most common drugs used include:
- Cisplatin
When chemo is used without radiation, the most common combinations include:
- Gemcitabine and cisplatin
- Dose-dense methotrexate, vinblastine, doxorubicin , and cisplatin
- Cisplatin, methotrexate, and vinblastine
- Gemcitabine and paclitaxel
For some people, the side effects of getting more than one chemo drug might be too much to handle. For those people, treatment with a single drug, such as gemcitabine or cisplatin, may be an option. Other drugs sometimes used alone for bladder cancer include, docetaxel, paclitaxel, doxorubicin, methotrexate, ifosfamide, and pemetrexed.
Doctors give chemo in cycles, with each period of treatment followed by a rest period to allow the body time to recover. Each cycle typically lasts for a few weeks.
Most bladder cancers are transitional cell cancers, but there are other types as well, including squamous cell carcinoma, adenocarcinoma, and small cell carcinoma. These rare types of bladder cancer may be treated with drugs different from those listed above.
Don’t Miss: Do Probiotics Help With Bladder Infections
Treating Bladder Cancer: Neoadjuvant Vs Adjuvant Therapy
M. Dror Michaelson, MD, PhDOncology
Occult distant micrometastasis at the time of radical cystectomy leads predominantly to distant failures in patients with locally advanced muscle-invasive transitional cell carcinoma of the bladder. Cisplatin-based combination chemotherapy enhances survival in patients with metastatic urothelial cancer. Studies evaluating adjuvant chemotherapy have been limited by inadequate statistical power. However, randomized clinical trials have demonstrated a survival benefit for neoadjvuant cisplatin-based combination chemotherapy, which should be considered a standard of care. In addition, neoadjuvant therapy may assist in the rapid development of novel systemic therapy regimens, since pathologic complete remission appears to be a powerful prognostic factor for long-term outcomes. Patients who are either unfit for or refuse radical cystectomy may benefit from neoadjuvant chemotherapy with or without radiation to enable bladder preservation.
The poor survival after local treatment for TCC, usually due to distant recurrence, has provided impetus for studies of systemic treatment before or after local treatment. Multiple randomized studies have been attempted, some with clear results, but many with either an ambiguous outcome or failure due to lack of accrual. Drs. Sonpavde and Lerner have comprehensively reviewed the clinical trials that have been carried out, particularly for neoadjuvant chemotherapy.
Chemotherapy in TCC
Disclosures:
Data Collection And Analysis
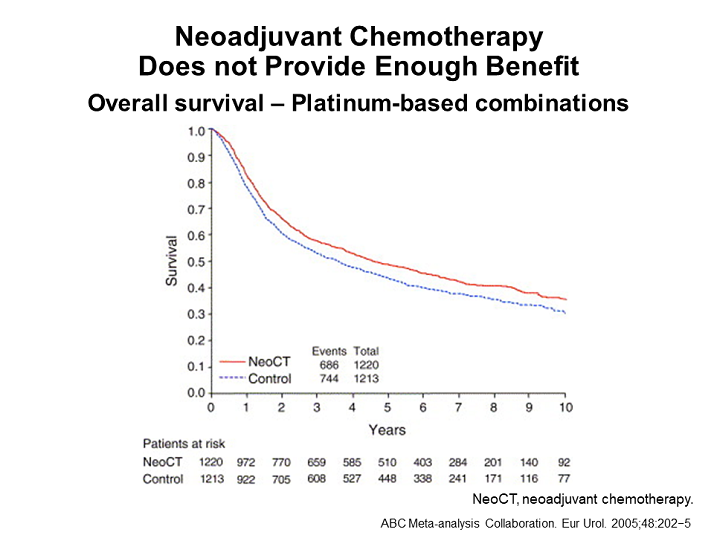
We collected, validated and reanalysed updated data on all randomised patients from all available randomised trials, including 3005 patients from 11 RCTs. For all outcomes, we obtained overall pooled hazard ratios using the fixed effects model. To explore the potential impact of trial design we preplanned analyses that grouped trials by important aspects of their design that might influence the treatment effect. To investigate any differences in effect by predefined patient subgroups we used a stratified logrank analysis on the primary endpoint of survival.
Read Also: Causes Of Recurrent Bladder Infections
How You Have It:
Week 1: You usually have an injection of mitomycin C into your vein on the first day of radiotherapy. You also have a drip of fluorouracil into your bloodstream for 5 days.
Week 4: At the beginning of the 4th week you have the fluorouracil as a drip for 5 days.
You usually have your chemotherapy through a PICC line so you can go home with it. PICC stands for peripherally inserted central catheter. PICC lines are long, plastic tubes that give the drugs directly into a large vein in your chest. You have the tube put in just before your treatment starts and it stays there as long as you need it.
When Is Neoadjuvant Chemotherapy Appropriate With Bladder Cancer Surgery
Bladder cancer is a complex disease that requires an individualized treatment plan, and not everyone is a candidate for chemotherapy. In general, though, chemotherapy may be administered prior to bladder cancer surgery if the cancer is rapidly spreading or has grown into the bladder walls connective tissue. Chemotherapy may also be given following surgery to help destroy any cancer cells that remain.
Recommended Reading: Bladder Leakage Pads For Men
Should We Spare Neoadjuvant Chemotherapy In Low
Günter Niegisch
Department of Urology, Medical Faculty, Heinrich Heine University , Germany
Correspondence to:
Provenance: This is an invited article commissioned by Section Editor Xiao Li .
Submitted Mar 31, 2019. Accepted for publication Apr 16, 2019.
doi: 10.21037/tau.2019.04.04
Table 1
In this context, Lyon et al. validated the M.D. Anderson model with a special focus on the question whether in LR patients NAC could be reliably omitted . In their institutional database, they identified 1,025 low-risk and 906 high-risk patients 104 low-risk and 196 high-risk patients having been treated by neoadjuvant chemotherapy. Of note, patients treated by NC were younger, had fewer comorbidities and a worse clinical stage as compared to patients with immediate radical cystectomy. Further, more lymph-nodes were removed in patients who underwent neoadjuvant chemotherapy.
As expected, high-risk patients undergoing immediate radical cystectomy had both a worse cancer-specific as well as a worse overall survival when compared to low-risk patients undergoing immediate radical cystectomy . Focussing on low-risk patients, a higher likelihood of cancer downstaging was observed in those, who underwent neoadjuvant chemotherapy. Though downstaging resulted in both improved OS and CSS in low-risk patients, administration of neoadjuvant chemotherapy did either improve CSS nor OS in low-risk patients.
Where You Have It
Usually you have the treatment in the outpatient department of a hospital.
Specialist chemotherapy nurses inject your chemotherapy drugs or you may have the drugs through a drip over a longer time. This depends on the type of chemotherapy you have. You usually you can go home after your treatment.
You usually have chemotherapy through a small tube called a cannula. Or you may have it through a central line, the most common type being a PICC line.
Watch this short 3 minute video on what it’s like to have chemotherapy
Read Also: What Is The Treatment For Bladder Cancer Stage 1
Timing Of Nac And Then Rc
In clinical practice there is debate on how much an invasive intervention such as RC should be delayed after NAC in order to maximize the patientâs recovery and ability to tolerate surgery without affecting the oncological outcomes and there is general agreement that RC should be delayed for a period after the last dose of NAC in order to maximize the patientâs blood counts and perhaps ability to tolerate surgery. In this context, RCTs investigating NAC provides more information on the time frame between RC and NAC .
A population based study form the Netherlands including 1,782 patients reported that a delay in RC greater than 3 months was not associated with OS notably 93% of the patients in the cohort underwent RC within 3 months thus limiting the number of patients with delayed treatment. Interestingly this study a separate subgroup analysis was performed for 105 patients who underwent neoadjuvant treatment and again failed to find association between timing to RC and OS . Investigation for the potential causes of delay in RC found that patients who were older than 75 years , treated in a university hospital and being referred from another hospital for RC were less likely to undergo RC within 3 months .
Cmv And Mvac As Standard Nac Regimens
The first of these phase III trials randomized 976 patients with high-grade cT2-T4a N0-NX M0 bladder cancer to receive either CMV chemotherapy for three cycles or no chemotherapy, followed by local therapy with either cystectomy or radiotherapy. Long-term follow-up revealed an OS advantage at 10 years for patients receiving NAC . There was a statistically significant 16 percent reduction in the risk of death for patients receiving CMV prior to local therapy.
Another major trial initiated by SWOG used MVAC as the NAC regimen prior to radical cystectomy. It included 317 patients enrolled from 1987 to 1998 with stage cT2-T4a muscle-invasive bladder cancer who were intended to undergo radical cystectomy. Patients were randomized 1:1 to receive either three cycles of MVAC followed by radical cystectomy or radical cystectomy alone.
Intention-to-treat analysis revealed median OS in the MVAC plus cystectomy group to be 77 months as compared to 46 months in the cystectomy group . More patients in the MVAC plus cystectomy group had pathologic complete response at the time of cystectomy compared to patients who only had cystectomy . Pathologic complete response was associated with 85 percent disease-free status rate at five years.
Muscle-invasive urothelial carcinoma
Read Also: How Do You Fix Overactive Bladder
Side Effects Of Chemotherapy
Chemo drugs attack cells that are dividing quickly, which is why they work against cancer cells. But other cells in the body, such as those in the bone marrow , the lining of the mouth and intestines, and the hair follicles, also divide quickly. These cells are also likely to be affected by chemo, which can lead to side effects.
The side effects of chemo depend on the type and dose of drugs given and how long they are taken. When chemo and radiation are given at the same time, side effects tend to be worse. Common side effects of chemo include:
- Nausea and vomiting
- Constipation
- Increased risk of infections
- Easy bleeding or bruising, even after minor cuts or injuries
- Fatigue
These side effects usually go away over time after treatment ends. There are often ways to lessen these side effects, some can even be prevented. For instance, drugs can be used to help prevent or reduce nausea and vomiting. Ask your health care team about the side effects your chemo drugs may cause and what can be done to prevent and/or treat them.
Some chemo drugs can cause other, less common side effects. For example, drugs like cisplatin, docetaxel, and paclitaxel can damage nerves. This can sometimes lead to symptoms such as pain, burning or tingling, sensitivity to cold or heat, or weakness. This is called peripheral neuropathy.
Neoadjuvant Chemotherapy Use In Bladder Cancer: A Survey Of Current Practice And Opinions
N. G. Cowan
1Department of Urology, Oregon Health and Science University, 3303 SW Bond Avenue, Portland, OR 97239, USA
2Department of Public Health and Preventive Medicine, Oregon Health and Science University, 3303 SW Bond Avenue, Portland, OR 97239, USA
3Department of Urology, University of Wisconsin, Madison, WI 53705, USA
4MSKCC, Department of Surgery, Urology Service, New York, NY 10065, USA
5National Cancer Institute, Medical Oncology Branch and Affiliates, Bethesda, MD 20892, USA
6Department of Urology, University of Washington, Seattle, WA 98195, USA
Academic Editor:
Abstract
1. Introduction
Despite the robust data supporting its use, there has been a relatively low rate of NAC utilization over the past decade, estimated to have increased from approximately 1% to 17% in the USA between 1998 and 2008 . More recent USA data reports a 17% utilization rate at a high-volume tertiary center . Reasons for this underutilization remain to be fully elucidated as few studies in the USA have broadly evaluated why patients are not receiving NAC. We sought to more clearly define these reasons and determine the frequency of NAC utilization by surveying a contemporary cohort of urologic oncologists.
2. Materials and Methods
The survey was sent to all active members of the Society for Urologic Oncology in January 2012. We excluded respondents who identified themselves as medical oncologists or fellows.
3. Results
You May Like: Is Green Tea Good For Bladder Infection