Predictive Factors Of Recurrence
Demographic and epidemiologic characteristics
Although men are three to four times more likely to develop BC, several epidemiologic reports associated female gender with a more advanced disease and worse survival rates . Messer et al. confirmed that female gender, after adjusting to standard clinical and pathologic features, was associated with an increased risk for cancer-specific mortality and disease recurrence compared to male gender in patients undergoing open RC. In other studies, gender was not associated with outcomes in stage-adjusted analyses, whereas pathologic tumor stage remained the most powerful factor influencing the course of disease in both genders .
Elderly patients have more years to compound comorbidities. As such, they are associated with higher mortality after RC . In a retrospective analysis of 605 patients treated with open RC, Horovitz et al. reported that octogenarians had comparable RFS to the younger counterparts . Conversely, an overview of the Bladder Cancer Research Consortium reported that patients aged > 80 years had a significantly greater risk of disease recurrence than patients aged 60 years . However, the retrospective nature of the studies suffered of the selection bias related to the higher use of bladder-sparing techniques in older patients and to the lower use of both NAC and AC.
Clinical characteristics
Histologic patterns
Pathologic patterns, tumor and node stage
What Causes Bladder Cancer
Bladder cancer occurs when cells within the lining of the bladder wall begin to grow in a disordered, uncontrolled way.
Exactly what prompts this disordered growth is not fully known. However, several factors associated with a higher risk of bladder cancer have been identified, including:
- Age – most people diagnosed with bladder cancer are older than 55 years.
- Sex – compared to women, men are 4 times more likely to develop bladder cancer.
- Smoking – smoking is associated with around half of all bladder cancers in men and women.
- Race – in the United States, White Americans have the highest rate of bladder cancer.
- Previous bladder cancer – people who have had bladder cancer may have a recurrence.
- Workplace exposures – certain chemicals in some workplaces may contribute to higher rates of bladder cancer in workers. For example, painters, hairdressers, and truck drivers are at increased risk.
- Arsenic in drinking water.
- Certain types of medication.
Intermediate Risk Early Bladder Cancer
People with intermediate-risk non-muscle-invasive bladder cancer should be offered a course of at least 6 doses of chemotherapy. The liquid is placed directly into your bladder, using a catheter, and kept there for around an hour before being drained away.
You should be offered follow-up appointments at 3, 9 and 18 months, then once every year. At these appointments, your bladder will be checked using a cystoscopy. If your cancer returns within 5 years, you’ll be referred back to a specialist urology team.
Some of the chemotherapy medicine may be left in your urine after treatment, which could severely irritate your skin.
It helps if you sit down to urinate and that you’re careful not to splash yourself or the toilet seat. Always wash the skin around your genitals with soap and water afterwards.
If you’re sexually active, it’s important to use a barrier method of contraception, such as a condom. This is because the medicines may be present in your semen or vaginal fluids, which can cause irritation.
You also shouldn’t try to get pregnant or father a child while having chemotherapy for bladder cancer, as the medicines can increase the risk of having a child with birth defects.
Read Also: Small Cell Bladder Cancer Treatment
Bladder Cancer Recurrence: A Persistent Fear For Patients
- Reactions 0 reactions
One of the hardest parts of living with bladder cancer is dealing with the risk of recurrence. For some, recurrences pop up every few months or years, and the relief of being “cancer-free” is short-lived. For others, bladder cancer is diagnosed, treated, and the person remains in remission but the fear that it could come back looms overhead. For others still, remission has yet to be achieved.
No matter your experience, there are similar worries, milestones, and ways of coping. Our Bladder Cancer In America 2019 survey found the many ways by which bladder cancer recurrences affect our community.
Surveillance After Radical Cystectomy
A group from the University of Texas MD Anderson Cancer Center retrospectively reviewed their postradical cystectomy surveillance protocol for 382 patients and concluded that a stage-specific approach was most appropriate. With a median follow-up of 38 months, 25% of patients experienced recurrences, with a median time to recurrence of 12 months. The 4 most common sites of recurrence were the lung, pelvis, bone, and liver. Seventy-four percent of recurrences were asymptomatic, and 43 of the 72 asymptomatic recurrences were detected with chest radiography or liver function serum tests.
Only 5% of patients with pT1 disease had subsequent metastases, and all were identified with chest radiography or liver function tests. Among 10 patients who were found to have asymptomatic intra-abdominal recurrences based on CT scan findings, 9 had pT3 disease. Patients with pT2 and pT3 disease had recurrence rates of 20% and 40%, respectively. All recurrences in patients with pT2 or pT3 disease occurred within 24 months.
Based on these findings, the group recommended that surveillance should include the following:
-
History
The group recommended scheduling surveillance according to the patients disease stage, as follows:
-
pT1 disease – Annually
-
pT2 disease – Every 6 months for 3 years, then annually
-
pT3 disease – As with pT2 disease, but starting at 3 months, with CT scanning at 6, 12, and 24 months
Recommended Reading: How To Find Out If You Have Bladder Cancer
Comparison Of Recurrence Risk Among Patients With Different Eortc
During the five-year follow-up period, 33 of 94 patients experienced intravesical recurrence, including 3 cases in the low-risk group, 7 cases in the intermediate-risk group, and 23 cases in the high-risk group. In addition, the KaplanMeier analysis demonstrated that the EORTC-GUCG risk scoring system had a significant correlation with RFS, and the high-risk group patients had shorter RFS than the other two groups .
|
Figure 1 Survival curve of RFS in patients at risk for different EORTC-GUCG risk scores. |
How Does Recurrence Of Bladder Cancer Affect Survival Rate
Recurrent bladder cancer is cancer that has returned after initial treatment. Recurrence rates for bladder cancer depend on the stage of the original tumor, with 5-year recurrence rates of approximately 65% in patients with non-invasive or in situ tumors and 73% in patients with slightly more advanced disease at first diagnosis.16
Many patients with non-invasive bladder cancer have recurrences that are typically not life threatening however, the prognosis is generally worse if the disease has spread into deeper layers of the bladder wall or beyond to the lymph nodes or other organs.
You May Like: How To Reduce Bladder Pain
Can Bladder Cancer Be Cured
When detected at an early stage, bladder cancer can usually be treated successfully whereas later-stage cancers may present greater challenges for the patient and their healthcare team. As discussed later, people who have had bladder cancer are at risk for recurrence for the best chance of successfully treating recurrent cancer, early detection is again important.
Doctor Visits And Tests
Your schedule of exams and tests will depend on the stage and grade of the cancer, what treatments youve had, and other factors. Be sure to follow your doctors advice about follow-up tests.
Most experts recommend repeat exams every 3 to 6 months for people who have no signs of cancer after treatment. These are done to see if the cancer is growing back or if there’s a new cancer in the bladder or urinary system. Your follow-up plan might include urine tests, physical exams, imaging tests , and blood tests. These doctor visits and tests will be done less often as time goes by and no new cancers are found.
- If your bladder hasnt been removed, regular cystoscopy exams will also be done every 3 months for at least the first 2 years.
- If you have a urinary diversion, you will be checked for signs of infection and changes in the health of your kidneys. Urine tests, blood tests, and x-rays might be used to do this. Your vitamin B12 will be checked at least once a year because urinary diversions made with your intestine can affect B12 absorption. Your doctor will also talk to you about how well you’re able to control your urine. Tests will be done to look for signs of cancer in other parts of your urinary tract, too.
Some doctors recommend other lab tests as well, such as the urine tumor marker tests discussed in Can Bladder Cancer Be Found Early? Many of these tests can be used to help see if the cancer has come back, but so far none of these can take the place of cystoscopy.
Also Check: Can You Have A Fever With A Bladder Infection
Cost Issues And Follow
Finally there is a cost issue with bladder cancer and follow-up. Leal et al. looked at the economic costs of bladder cancer across the European Union . These were 4.9 billion in 2012, of which health care costs were 2.9 billion , productivity loss 1.1 billion and informal care costs 0.9 billion . Bladder cancer costs represented 5% of total health care cancer costs and 3% of all cancer costs in the EU in 2012. Of note, difference between the least and most expensive country was> tenfold. For follow-up costs, all three fields play a role. Interestingly, Mossanen et al. used a Markow model to specifically evaluate costs of surveillance of NMIBC Their index patient was a compliant 65-year-old male, and they used four health states: no evidence of disease, recurrence, progression/cystectomy and death. The cumulative costs over a 5-year period were USD 52,125, 146,250 and 366,143 for low-, intermediate- and high-risk, respectively. Costs for recurrence were highest in the low-risk group, but still not more than 8% of the total costs of low risk. Progression and subsequent treatment results in much higher costs , even when not frequent in low-risk patients.
In all, there is certainly an opportunity to reduce patient burden and costs in an adapted follow-up strategy with a marker with a high NPV, where the financial benefit obviously depends on the price of the marker. Prospective studies will be necessary to validate these assumptions on national levels.
For Patients With A Urostomy
If you had a radical cystectomy and now have a urostomy, you might worry even about everyday activities at first. You might have to alter some of your daily routines because of changes in how you urinate. Other issues such as having sex might also cause concerns .
Its normal to have worries and concerns when adjusting to such a major change. But its important to know there are health care professionals who are specially trained to help people with their urostomies. They can teach you to take care of your urostomy and help you cope with the changes it brings. You can also ask the American Cancer Society about programs offering information and support in your area. For more information, see our Urostomy Guide.
Read Also: Can Bladder Infection Heal On Its Own
Data Collection And Patient Follow
Data Collection
All patients received routine hematological examination, computed tomography, transabdominal ultrasound, urine cytology or tissue biopsy, cystoscopy prior to surgery in order to diagnose NMIBC, and finally confirmed by postoperative pathology. Pre-operative baseline clinical pathology and laboratory data such as age, gender, body mass index , smoking history, tumor size, pathological T stage, and grade were obtained through electronic medical records in the hospital and reviewed. All histopathology reports were based on the eighth edition of Tumor-Node-Metastasis staging system, and the grade was assessed based on the 2004 WHO grading system.18,19 Tumor size was the sum of the longest diameters of all postoperative pathological specimens. According to the blood test results , the preoperative serum albumin concentration, total cholesterol concentration and total peripheral lymphocyte count of all individuals were used to calculate the CONUT score. Based on the previous study,12 the scoring criteria of CONUT are illustrated in Table 1.
|
Table 1 The Scoring System for the Controlling Nutritional Status Scale |
Follow-Up
Type Of Studies And Quality Of The Evidence

For the analysis of the predictors of recurrence, 313 studies were retrospective, 14 were prospective and 27 were randomized clinical trials . Sample size ranged between 33 and 9064 patients. Most series involved multiple surgeons. For the analysis of recurrence rate, 29 studies were retrospective, 3 were prospective and 16 were RCTs. Sample size ranged between 110 and 9064 patients. Risk of bias evaluation is summarized in Supplementary Table 1.
Recommended Reading: What Kind Of Doctor Does Bladder Prolapse Surgery
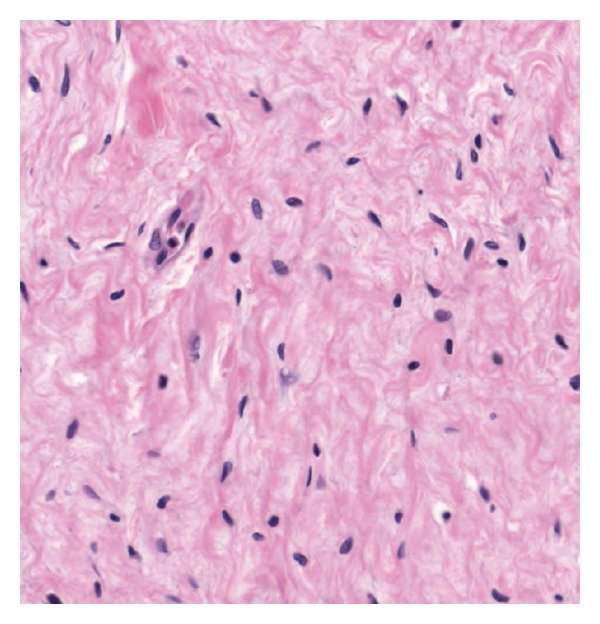
Molecular Biology Of Cis
NMIBC is sub-classified according to histology and degree of tumor invasion. Tumors are either papillary , confined to the mucosa or invading into the lamina propria but not into the muscle . CIS is considered a high-grade cancer due to its degree of cellular dysplasia and aggressive behavior .
A recent characterization of the molecular biology of CIS comes from Hedegaard and colleagues . This multi-institutional trial characterized NMIBC into three molecular subtypes with the goal of identifying which patients with NMIBC would benefit from early RC. Class 1 was mostly composed of low grade urothelial tumors, which expressed early cell cycle genes and mutations in Fibroblast Growth Factor Receptor 3 . Class 2 tumors demonstrated high expression of late cell cycle genes and epithelial-mesenchymal transition associated genes. Class 3 tumors had a higher expression of primitive cytokeratins, which are markers for bladder cancer stem cells. Class 2 tumors had a high prevalence of CIS with a higher risk of progression to MIBC when compared to class 1 and 3 tumors.
Heide and colleagues performed multiregional whole exome sequencing of ten RC samples . The authors found APOBEC mutational signatures active in CIS these appeared to be a source of mutations that persisted as the tumor evolved into invasive cancer. The investigators suggest that they key alterations in invasive cancer are also acquired in CIS as both of these share up to 80% of mutations.
About One Third Had Cancer Recurrence
Of these patients, 548 had bladder cancer recurrence, most of whom experienced recurrence in the first 5 years after their radical cystectomy . Late recurrence occurred in 67 of study patients. The average amount of time to bladder cancer recurrence was 12 months, with 80% of recurrences happening in the first three years. These 548 recurring bladder cancer patients account for about 33% of the study patients who were treated, which is less than the national average of 50% of patients having bladder recurrence.
Also Check: Does Bladder Infection Cause Diarrhea
Management Of Ta T1 And Tis Bladder Cancer
Surgery
Superficial bladder cancer is typically managed with complete transurethral resection of intravesical disease. Careful pathologic examination of the resected tissue is required to exclude invasion of the muscularis propria. Given the high likelihood of disease recurrence or the development of new tumors, patients should undergo urinary cytologic and cystoscopic examinations every 4 to 6 months for 5 years after resection. Persistently abnormal findings on urine cytology after normal findings on cystoscopy should prompt evaluation of the prostatic urethra in men and the upper urinary tract in men and women.81-83 Risk factors for tumor recurrence after transurethral resection include high histologic grade, involvement of the lamina propria , multifocal disease, and the presence of CIS.84 About 15% of noninvasive cases eventually progress to involve the muscularis propria, and most of these are poorly differentiated, sessile, T1 tumors with diffuse CIS.29
Radical cystectomy should be considered for patients with extensive recurrent Ta, T1, or Tis disease that is refractory to intravesical bacillus Calmette-Guérin those with risk factors for progression to muscle invasion and those with severe, irreversible impairment of bladder function due to recurrent disease or prior treatment.
Intravesical Immunotherapy or Chemotherapy
Radiation Therapy
Basir Tareen MD, Samir S. Taneja MD, in, 2010
Relapse Of Pt0 Bladder Cancer Possible After Radical Cystectomy
Despite the favorable prognosis associated with pathologic T0 bladder cancer, relapse can occur, especially among patients with positive lymph nodes, investigators reported at the 22nd annual meeting of the Society of Urologic Oncology.
Using the International Robotic Cystectomy Consortium database, Ahmed Aly Hussein, MD, MS, and colleagues from Roswell Park Comprehensive Cancer Center in New York, New York, identified 471 patients with pT0 bladder cancer or absence of residual tumor at the time of robot-assisted radical cystectomy . Of the cohort, 37% had received neoadjuvant chemotherapy. Positive lymph nodes were found in 5%.
Bladder cancer relapsed in 7% of patients, including 3% with local and 5% with distal recurrence, Dr Husseins team reported. The most common sites of both local and distant recurrences were the pelvis and lungs . No patient had peritoneal recurrence.
At 5 years, recurrence-free, disease-free, and overall survival rates were 88%, 93% and 79%, respectively.
According to a multivariate model, positive lymph node status and reoperation within 30 days significantly increased the risk for recurrence by 10.2- and 7.1-fold, respectively, and all-cause mortality by 4.9- and 3.5-fold, respectively, Dr Husseins team reported. Chronic kidney disease was another risk factor for worse overall survival, and older age was another risk factor for recurrence. Predictors for disease-free survival could not be calculated due to the small number of patients.
Also Check: How Long Should A Bladder Infection Last
Cis Of The Bladder: Significance And Implications For Therapy
Article type: Review Article
Authors: Mirabal, Jorge Riveraa | Taylor, John A.b | Lerner, Seth P.a *
Affiliations: Scott Department of Urology, Baylor College of Medicine, Houston, TX, USA | Department of Urology, University of Kansas Medical Center, Kansas City, KS, USA
Correspondence: Correspondence to: Seth P. Lerner, MD, FACS Professor, Scott Department of Urology Beth and Dave Swalm Chair in Urologic Oncology, Vice-Chair for Faculty Affairs, Director of Urologic Oncology Director of the Multidisciplinary Bladder Cancer Program Co-Editor in Chief Bladder Cancer Baylor College of Medicine Medical Center 7200 Cambridge, MC BCM380 Houston, Texas 77030, USA. Tel.: +1 O 7137986841 E-mail: .
Keywords: Carcinoma in situ, bladder cancer, transitional cell carcinoma, NMIBC, BCG
DOI: 10.3233/BLC-190236
Journal: Bladder Cancer, vol. 5, no. 3, pp. 193-204, 2019
Abstract