Bladder Cancer Clinical Trials
What about Clinical Trials?
You may hear about clinical trials for your bladder cancer. Clinical trials are research studies that test if a new treatment or procedure is safe and effective.
Through clinical trials, doctors find new ways to improve treatments and the quality of life for people with disease. Trials are available for all stages of cancer. The results of a clinical trial can make a major difference to patients and their families. Please visit our clinical trials research webpage to learn more.
Combination Of Immunotherapy And Cytotoxic Chemotherapy
Neoadjuvant immunotherapy with cytotoxic chemotherapy is being extensively investigated. Conventional chemotherapy can stimulate tumor-specific immune responses either by inducing immunogenic cell death of tumor cells or by engaging immune effector mechanisms . ICD, with several mechanismsincluding exposure of calreticulin to the outer cell surface release of adenosine triphosphate, annexin-1, and high-mobility group box 1 protein autophagy inflammasome activation induction of type 1 interferon signaling, and release of mitochondrial formyl peptidesinduces premortem reticular stress and releases tissue-damage-denoting substances that alert the immune system . Furthermore, conventional chemotherapy can promote the activation of immune effector cells, hamper the functions of immunosuppressive cells, or alter whole-body physiology through the promotion and/or activation of mechanisms that ultimately support immunological competence . These results provide a scientific rationale for the investigation of the combination of chemotherapy and immunotherapy thus, many trials are currently ongoing.
Palliative Or Supportive Care
If your cancer is at an advanced stage and can’t be cured, your medical team should discuss how the cancer will progress and which treatments are available to ease the symptoms.
You can be referred to a palliative care team, who can provide support and practical help, including pain relief.
Page last reviewed: 01 July 2021 Next review due: 01 July 2024
Don’t Miss: Chances Of Surviving Bladder Cancer
Radical Cystectomy And Adherence To Guidelines
Current guidelines in the USA as well as in Europe clearly recommend a radical surgical approach for patients diagnosed with MIBC . Previous studies from the USA investigating the implementation of RC in clinical practice had described low adherence to evidence-based guideline recommendations . Williams et al. described 2016 poor RC results with a share of only 18.9% receiving RC for MIBC . However, the SEER data seem to massively overestimate the share of patients receiving no treatment. Because of this obvious shortcoming we had to waive another planned comparison study of Germany and the USA . For a different aspect, our working group recently compared the German hospital billing database and the Nationwide Inpatient Sample from the USA. We were able to show an increase in the annual numbers of RC treatments in Germany while an annual number of cases in the USA remained stable . In total, the number of RCs in Germany increased by 31% from the years 2006 to 2014 and older patients were the main drivers of growing RC numbers in Germany.
Combination Of Immunotherapy And Other Emerging Agents Or Radiotherapy
NEODURVARIB was a single-arm, phase 2 trial that assessed the impact of neoadjuvant durvalumab plus olaparib in MIBC . Patients received 1500 mg durvalumab every 4 weeks for up to a maximum of 2 months plus 300 mg olaparib for up to 56 days . The primary endpoint was pCR rate, which was 44.5%. One death related to postoperative complications was reported. Grade 34 AEs were detected in only 8.3% of patients. ABATE is an open-label, single-arm study to assess the efficacy and safety of cabozantinib with atezolizumab as neoadjuvant therapy for cT2T4aN0/xM0 advanced UC patients who are either cisplatin-ineligible or decline cisplatin . The primary endpoint is downstaging to non-muscle-invasive disease . This study is ongoing, and results are not yet reported.
Many efforts to find an appropriate partner for CPI therapy in the neoadjuvant setting are underway. There are several trials involving emerging agentsincluding CD73 inhibitor , replication-competent oncolytic adenovirus , and synthetic benzamide-derivative histone deacetylase inhibitor . These studies are currently ongoing, and the results have not yet been reported.
Read Also: Galvanized Pressure Tank Vs Bladder Tank
Other Treatments For Non
Other treatments are being tested for non-muscle-invasive bladder cancer. You may be offered these as part of a clinical trial. These treatments may only be available at some hospitals. If your urologist thinks a clinical trial may be helpful for you, they can refer you to the hospital doing the trial.
Treatments include:
Treating Stage I Bladder Cancer
Stage I bladder cancers have grown into the connective tissue layer of the bladder wall , but have not reached the muscle layer.
Transurethral resection with fulguration is usually the first treatment for these cancers. But it’s done to help determine the extent of the cancer rather than to try to cure it. If no other treatment is given, many people will later get a new bladder cancer, which often will be more advanced. This is more likely to happen if the first cancer is high-grade .
Even if the cancer is found to be low grade , a second TURBT is often recommended several weeks later. If the doctor then feels that all of the cancer has been removed, intravesical BCG or intravesical chemo is usually given. If all of the cancer wasn’t removed, options are intravesical BCG or cystectomy .
If the cancer is high grade, if many tumors are present, or if the tumor is very large when it’s first found, radical cystectomy may be recommended.
For people who arent healthy enough for a cystectomy, radiation therapy might be an option, but the chances for cure are not as good.
You May Like: Bcg Treatment Schedule For Bladder Cancer
Developing A Treatment Plan
In cancer care, different types of doctors often work together to create a patients overall treatment plan that combines different types of treatments.This is called a multidisciplinary team. This team is usually led by a urologist, a doctor who specializes in the genitourinary tract, or a urologic oncologist, a doctor who specializes in treating cancers of the genitourinary tract. Cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, and others.
Treatment options and recommendations depend on several factors, including:
-
The type, stage, and grade of bladder cancer
-
Possible side effects
-
The patients preferences and overall health
Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
The first treatment a person is given for advanced urothelial cancer is called first-line therapy. If that treatment stops working, then a person receives second-line therapy. In some situations, third-line therapy may also be available.
Adjuvant systemic therapy is treatment that is given after radical surgery has been completed. In bladder cancer, adjuvant therapy is usually cisplatin-based chemotherapy or treatment in a clinical trial. Neoadjuvant therapy is treatment that is given before surgery, such as cisplatin-based chemotherapy.
Bladder Cancer Icd 10 Coding:
Icd 10 code for history of bladder cancer is the method of organizing the symptoms and stages of cancer. The initial symptoms of bladder cancer are painful urine, blood in the urine, pain in the lower back. Moreover, you will feel frequent and urgent urination all the time. If you are facing these symptoms, then it is time to consult your doctor immediately.
Bladder cancer classifies into category C67 of ICD-10-CM. These digits identify the location of the tumor, as follows:
- C67.1, Malignant neoplasm of trigone of the bladder.
- C67.2, Malignant neoplasm of the dome of the bladder.
- C67.3, Malignant neoplasm of the lateral wall of the bladder.
- C67.4: Malignant neoplasm of bladder, unspecified.
- C67.5: Malignant neoplasm of bladder neck including internal urethral orifice.
- C67.6: Malignant neoplasm of ureteric orifice.
- C67.7: Malignant neoplasm of the urachus.
- C67.8: Malignant neoplasm of overlapping sites of the bladder.
Recommended Reading: Overactive Bladder Only At Night
Don’t Miss: Blood In Urine Female Bladder Infection
The Role Of Chemotherapy In Treatment Of Organ Confined Muscle
If the bladder cancer has invaded the muscle of the bladder wall, then there is a very high risk that the patient will die of bladder cancer unless with either or radical is done. Although radical cystectomy or radical radiotherapy offers the best chance of cure, unfortunately up to half of these people still go on to die of bladder cancer. This is usually due to the cancer returning in the region of the bladder, existing unsuspected spread to or, more typically, in other parts of the body such as the lymph nodes, lungs, liver or bones. For many cancers this risk of can be reduced or delayed by giving before and/or after surgery or radical radiotherapy. However, these treatments are associated with significant side effects. These side effects may be more problematic in people with other illnesses or people who are generally less fit.
What To Do Before And After Treatment
Talk with your doctors about whether you need to do anything to prepare for treatment and help your recovery. Some things they may suggest are:
Stop smoking If you smoke, aim to quit before starting treatment. If you keep smoking, you may not respond as well to treatment and you may have more treatment-related side effects. Continuing to smoke also increases your risk of cancer returning. For support, see your doctor, call Quitline 13 7848 or visit iCanQuit.
Begin or continue an exercise program Exercise will help build up your strength for treatment and recovery. It can also help you deal with side effects of treatment. Talk to your doctor, exercise physiologist or physiotherapist about the right type of exercise for you.
Improve your diet Aim to eat a balanced diet with a variety of fruit, vegetables, wholegrains and protein. Eating well can improve your strength and you may respond better to treatment.
See a physiotherapist They can teach you exercises to strengthen your pelvic floor muscles, which help control how your bladder and bowel work. These exercises are useful if you have a neobladder, a partial cystectomy or radiation therapy.
When deciding on treatment for muscle-invasive bladder cancer, you may want to discuss your options with a urologist, radiation oncologist and medical oncologist. Ask your GP for referrals.
Recommended Reading: Gene Therapy For Bladder Cancer
Cystoscopy With Cautery Destruction Of The Bladder Tumor
Cystoscopy is an outpatient procedure during which a thin, lighted tube with a camera is passed through the urethra into the bladder, allowing your doctor to see the inside of the bladder.
Most modern cystoscopes are also equipped with channels that permit small instruments to be passed into the bladder. During a cystoscopy, your doctor may use these instruments to remove tissue, stop bleeding with a special electrical device called an electrocautery or even perform laser treatment. If the bladder cancer tumor is small enough, this cautery may be used to remove the cancer.
Treating Stage Ii Bladder Cancer
These cancers have invaded the muscle layer of the bladder wall , but no farther. Transurethral resection is typically the first treatment for these cancers, but it’s done to help determine the extent of the cancer rather than to try to cure it.
When the cancer has invaded the muscle, radical cystectomy is the standard treatment. Lymph nodes near the bladder are often removed as well. If cancer is in only one part of the bladder, a partial cystectomy may be done instead. But this is possible in only a small number of patients.
Radical cystectomy may be the only treatment for people who are not well enough to get chemo. But most doctors prefer to give chemo before surgery because it’s been shown to help patients live longer than surgery alone. When chemo is given first, surgery is delayed. This is not a problem if the chemo shrinks the bladder cancer, but it might be harmful if the tumor continues to grow during chemo.
If cancer is found in nearby lymph nodes, radiation may be needed after surgery. Another option is chemo, but only if it wasn’t given before surgery.
For people who have had surgery, but the features of the tumor show it is at high risk of coming back, the immunotherapy drug, nivolumab, might be offered. When given after surgery, nivolumab is given for up to one year.
For patients who cant have surgery because of other serious health problems, TURBT, radiation, chemotherapy, or some combination of these may be options.
You May Like: Why Do I Have A Bladder Infection
Adjuvant Immunotherapy In Mibc
There are three large-scale, randomized phase 3 trials for adjuvant immunotherapy . The IMvigor 010 study a multicenter, open-label, randomized phase 3 trialevaluates atezolizumab for adjuvant therapy in patients with high-risk muscle-invasive UC . Patients had ypT24a or ypN+ tumors following NAC or pT34a or pN+ tumors if no NAC was administered. Patients not treated with NAC must have been ineligible for or declined cisplatin-based NAC. A total of 807 patients were randomly assigned to receive 1200 mg atezolizumab administered intravenously every 3 weeks for 16 cycles, up to one year, or to observation . A total of 6.6% patients had upper-tract MIUC. The primary endpoint was DFS the trial did not meet its primary endpoint, with a nonsignificant difference in DFS between the atezolizumab group and observation . Atezolizumab was generally tolerable, and had no new safety signals.
Radiotherapy With A Radiosensitiser
Radiotherapy is given by a machine that beams the radiation at the bladder . Sessions are usually given on a daily basis for 5 days a week over the course of 4 to 7 weeks. Each session lasts for about 10 to 15 minutes.
A medicine called a radiosensitiser should also be given alongside radiotherapy for muscle-invasive bladder cancer. This medicine affects the cells of a tumour, to enhance the effect of radiotherapy. It has a much smaller effect on normal tissue.
As well as destroying cancerous cells, radiotherapy can also damage healthy cells, which means it can cause a number of side effects. These include:
- diarrhoea
- tightening of the vagina , which can make having sex painful
- erectile dysfunction
- tiredness
- difficulty passing urine
Most of these side effects should pass a few weeks after your treatment finishes, although there’s a small chance they’ll be permanent.
Having radiotherapy directed at your pelvis usually means you’ll be infertile .
After having radiotherapy for bladder cancer, you should be offered follow-up appointments every 3 months for the first 2 years, then every 6 months for the next 2 years, and every year after that. At these appointments, your bladder will be checked using a cystoscopy.
You may also be offered CT scans of your chest, abdomen and pelvis after 6 months, 1 year and 2 years. A CT scan of your urinary tract may be offered every year for 5 years.
Read Also: What Causes An Overactive Bladder In Males
Specific Coding For Malignant Neoplasm Of Bladder
Non-specific codes like C67 require more digits to indicate the appropriate level of specificity. Consider using any of the following ICD-10 codes with a higher level of specificity when coding for malignant neoplasm of bladder:
- BILLABLE CODE Use C67.0 for Malignant neoplasm of trigone of bladder
- BILLABLE CODE Use C67.1 for Malignant neoplasm of dome of bladder
- BILLABLE CODE Use C67.2 for Malignant neoplasm of lateral wall of bladder
- BILLABLE CODE Use C67.3 for Malignant neoplasm of anterior wall of bladder
- BILLABLE CODE Use C67.4 for Malignant neoplasm of posterior wall of bladder
- BILLABLE CODE Use C67.5 for Malignant neoplasm of bladder neck
- BILLABLE CODE Use C67.6 for Malignant neoplasm of ureteric orifice
- BILLABLE CODE Use C67.7 for Malignant neoplasm of urachus
- BILLABLE CODE Use C67.8 for Malignant neoplasm of overlapping sites of bladder
- BILLABLE CODE Use C67.9 for Malignant neoplasm of bladder, unspecified
Dont Miss: How Long Does It Take Azo Bladder Control To Work
Treating Stage 0 Bladder Cancer
Stage 0 bladder cancer includes non-invasive papillary carcinoma and flat non-invasive carcinoma . In either case, the cancer is only in the inner lining layer of the bladder. It has not invaded the bladder wall.
This early stage of bladder cancer is most often treated with transurethral resection with fulguration followed by intravesical therapy within 24 hours.
Recommended Reading: How To Test For A Bladder Infection At Home
Trimodal Therapy For Stage Ii Or Iii
A select group of people with Stage II or III bladder cancer may be able to be treated with trimodal therapy. This involves 3 modes of treatment:
- TURBT Your doctor will insert a scope into your bladder and use a wire loop to remove the tumor.
- Radiation Given after surgery, daily, for 4 to 6 weeks. Some patients may receive a radiosensitizer. This is a chemotherapy drug that helps make the radiation more effective.
- Systemic Chemotherapy May be given before the TURBT to shrink the tumor.
Trimodal therapy may cause common chemo and radiation side effects. Patients may also have problems with bladder, bowel, and sexual function.
Choosing Between Surgery And Radiotherapy
Your doctor might ask you to choose between surgery to remove your bladder or radiotherapy if both treatments are suitable for you.
But they might not recommend radiotherapy if:
- you have squamous cell bladder cancer
- there is carcinoma in situ in much of the bladder lining as well as invasive cancer
- initial chemotherapy is not working
- the cancer is blocking one or both of the tubes that carry urine into the bladder from the kidneys
Talk to your specialist about the risks and benefits of surgery or radiotherapy for you. They will discuss your treatment options with the multidisciplinary team.
You may need to meet with one or more of the specialists in the team to discuss your options. You make the final decision about which treatment you have.
Also Check: What Medications Are Used For Overactive Bladder
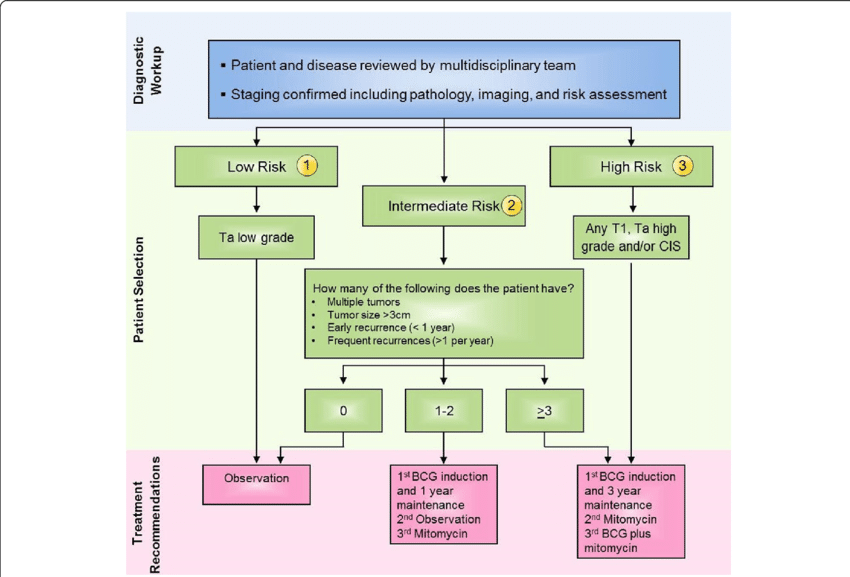
Further Treatment For Non
If you have a low-risk tumour, you will not need any further treatment after surgery.
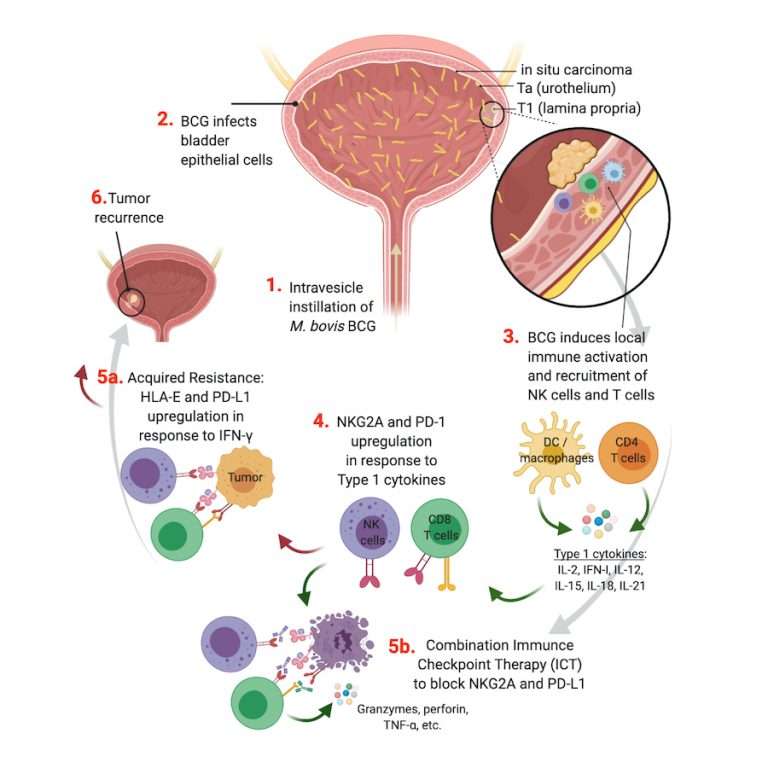
If you have an intermediate or high-risk tumour, you usually need further treatment. Treatment is usually with chemotherapy or an immunotherapy drug called BCG. Both are given directly into the bladder. High-risk bladder cancer is usually treated with BCG.
Occasionally, your specialist may ask you to think about having surgery to remove the bladder. This may happen if you have a very high-risk cancer or a cancer that comes back after BCG treatment. The operation is called a cystectomy.