Percutaneous Tibial Nerve Stimulation For Overactive Bladder
Percutaneous tibial nerve stimulation for overactive bladder is a minimally invasive, non-surgical treatment option for overactive bladder that helping to manage symptoms of urge incontinence, urinary frequency and urinary urgency. While PTNS may be used as a primary therapy, your doctor may use pharmacological therapies and pelvic floor muscle training to manage your symptoms of overactive bladder before administering PTNS for optimal results.
Percutaneous tibial nerve stimulation for overactive bladder is more effective and results in far fewer side effects than many OAB medications out there. Almost 80% of patients stop using OAB medicines just a year after starting, with adverse side effects accounting for 17% of discontinuation.
In cases where conservative methods arent working, PTNS is emerging as an effective treatment option for overactive bladder. Whats more, its proven efficacy has been the subject of discussion in a multitude of publications.
Tibial Nerve Stimulator Is Safe Effective And Durable 12
Twenty-six percent of patients with overactive bladder reported continence at 12 months.
A nickel-sized tibial nerve stimulator offers overactive bladder patients with urgency urinary incontinence long-term outcomes comparable to other treatment options, including percutaneous tibial nerve stimulation.
Findings of a study published in Urology1 imply OAB treatment with the investigational eCoin device is safe and achieves a durable response, says the studys lead author, urologist Peter Gilling, MD, of Tauranga Urology Research Ltd, Tauranga, New Zealand.
The decrease in incontinence episodes and the durability of the treatment are as good as any of the other available devices and techniques for refractory urge incontinence. Sixty-five percent of patients were considered responders, which is a very competitive result, Gilling said.
And compared with other neuromodulation techniques, eCoin appears to obviate patient factors that often affect compliance, such as onerous treatment schedules, according to Gilling.
eCoin is a fully implantable device with no leads, transducers, electrodes, or control unit necessary, he said.
Like percutaneous tibial nerve stimulation, eCoin aims to relieve symptoms of overactive bladder syndrome with urgency urinary incontinence by stimulating the tibial nerve.
A urologist implants the battery-powered eCoin subcutaneously in the medial lower leg. The in-office procedure, done under local anesthesia, takes about 20 minutes.
Percutaneous Tibial Nerve Stimulation Risks
Because PTNS is a minimally-invasive procedure, there are few side effects. However, patients may experience:
- Mild discomfort or pain at the insertion site including throbbing pain.
- Redness, inflammation or irritation at or near the insertion site.
- Possible bruising at the insertion site.
- Toe numbness.
- Stomach ache.
Not every patient is a candidate for PTNS. This procedure is not recommended for the following individuals:
- Patients with bleeding disorder, or who are taking blood thinners.
- Pregnant women, or those who may become pregnant during the course of treatment.
- Patients with pacemakers or defibrillators.
- Nerve damage or disorders If patients have diabetic neuropathy or other nerve disorders, they should discuss PTNS with their physician before starting treatment.
If you have overactive bladder symptoms and would like to discuss PTNS, contact Urology Austin to schedule an appointment with one of our urologists.
Related link
Don’t Miss: Best Supplements For Bladder Health
Effectiveness And Safety Of Tibial Nerve Stimulation Versus Anticholinergic Drugs For The Treatment Of Overactive Bladder Syndrome: A Meta
San-Chao Xiong#, Liao Peng#, Xu Hu, Yan-Xiang Shao, Kan Wu, Xiang Li
Department of Urology, Institute of Urology, West China Hospital , , China
Contributions: Conception and design: SC Xiong, L Peng Administrative support: X Li Provision of study materials or patients: SC Xiong, L Peng Collection and assembly of data: YX Shao, L Peng Data analysis and interpretation: SC Xiong, K Wu Manuscript writing: All authors Final approval of manuscript: All authors.
#These authors contributed equally to this work.
Correspondence to:
Background: This meta-analysis aimed to evaluate the efficacy and safety of tibial nerve stimulation and anticholinergic drugs for the treatment of overactive bladder syndrome .
Methods: Qualified studies up to November 3, 2020 were retrieved from PubMed, Embase, the Cochrane Library and Web of Science. Pooled mean differences were calculated to evaluate the improvement of micturition frequency per day, nocturia per night, urinary urgency episodes per day, incontinence episodes per day, and voided volume each time. Odd ratios were used to assess the discontinuation rate.
Results: A total of 6 RCTs including 291 patients were included. Comparing with those receiving ACDs, patients receiving TNS had a significantly better improvement of urge incontinence episodes , but had comparable effect on micturition , nocturia , urgency and voided volume . Moreover, TNS group had a significantly lower discontinuation rate during the trials.
Percutaneous Tibial Nerve Stimulation
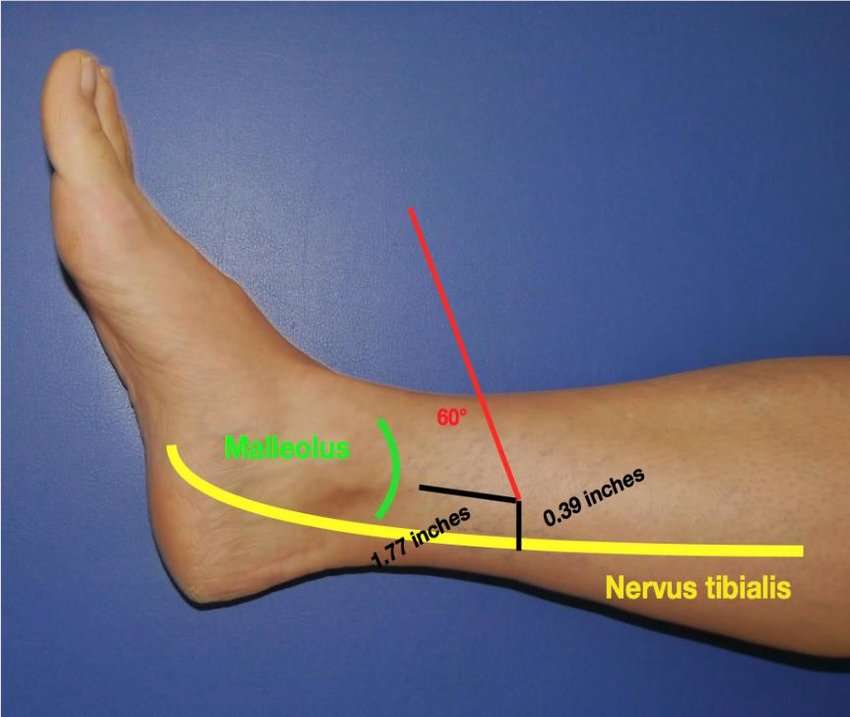
The posterior tibial nerve is stimulated by inserting a 34-gauge needle 45 cephalad to the medial malleolus. Once the current is applied, the flexion of the big toe or the movement of the other toes confirms the correct positioning of the needle electrode. The electrical current is a continuous square wave form with a duration of 200 Us and a frequency of 200 Hz. The intensity of the current is determined by the highest level tolerated by the patient. The stimulation sessions last for 30 min.
Don’t Miss: Treatment Of Overactive Bladder In Males
Efficacy Of Transcutaneous Vs Percutaneous Tibial Nerve Stimulation In Non
ABSTRACT
Background:Material and Methods:Results:
REFERENCES
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association / International Continence Society joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010 21:526. doi: 10.1007/s00192-009-0976-9
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: The Norwegian EPINCONT Study. J Clin Epidemiol. 2000 53:11507. doi: 10.1016/S0895- 435600232-8
García-Sánchez D, Gutiérrez-González A, Pérez- Ortega R, Gastelum-Félix L, Reyes-Gutiérrez M. Frecuencia de la vejiga hiperactiva en médicos generales. Rev Mex Urol. 2014 74:847.
Pratt TS, Suskind AM. Management of Overactive Bladder in Older Women. Curr Urol Rep. 2018 19:92. doi: 10.1007/s11934-018- 0845-5
Alfonso Barrera E, González Nuño M, Tena- Dávila Mata C, Valiente del Pozo A, Gago Blanco H, Usandizaga Elio R. Eficacia de la estimulación percutánea versus transcutánea del nervio tibial posterior en pacientes con vejiga hiperactiva. Rehabilitación. 2014 48:16874. doi: 10.1016/j.rh.2013.11.003
de Wall LL, Heesakkers JP. Effectiveness of percutaneous tibial nerve stimulation in the treatment of overactive bladder syndrome. Res Rep Urol. 2017 9:14557. doi: 10.2147/RRU. S124981
Stoller M. Afferent stimulation for pelvic floor dysfunction. Eur Urol. 1999 35:116.
What Are The Risks
Side effects are minimal but you may experience some pain or numbness. The main limitation of this technique is the need to attend for 12 weekly sessions without interruption. If you miss one session, treatment can be continued. If you miss more than one session, a fresh count will need to start again.
You May Like: Can Cervical Cancer Spread To The Bladder
Tibial Nerve Stimulation For Overactive Bladder Treatment
Tibial nerve stimulation for overactive bladder is a treatment that uses electrical signals to help control bladder contractions. It can reduce the number of times a person feels the urge to urinate and can also help reduce urinary leakage.
OAB is the term experts use to describe urinary symptoms, including urinary incontinence and a frequent, urgent need to empty the bladder.
According to the National Association for Continence, OAB affects an estimated 33 million people in the United States.
Symptoms of OAB include urinary incontinence, urinary frequency, an urgent need to urinate, and waking up to urinate.
This article looks at what TNS for OAB is, who can safely have TNS, and what the potential risks and side effects are.
TNS, or percutaneous TNS , is a nonsurgical procedure that doctors may recommend for OAB.
A 2017 review explains that PTNS derives from acupuncture, which has roots in traditional Chinese medicine.
The TN is located above the ankle and runs up the leg to the sacral nerves, which control the bladder and pelvic floor muscles.
According to the National Institute for Health and Care Excellence , scientists do not know exactly how PTNS acts on the bladder. They believe, however, that PTNS stimulates the posterior TN and the sacral nerve plexus, which can cause a change in a persons bladder activity.
The posterior TN contains nerve fibers that stem from the part of the spine where the nerves to the bladder and pelvic floor are.
Stimulation Protocol And Data Acquisition
The inserted nerve cuff electrode delivered rectangular pulses with a 200 s pulse width to the tibial nerve. The stimulation time was set to 30 min to mimic a typical clinical application,,. The threshold of stimulation intensity was set by observing toe twitches. In previous studies of both cats and rats, TNS with an intensity greater than 2 T was sufficient for inhibiting reflex bladder contractions,. Therefore, we applied TNS intensity between 2 and 3 T to inhibit the bladder. A cystometrogram was performed on the unanesthetized rats by the continuous infusion of body-warm saline at a rate of 0.1 ml/min until inter-contraction intervals stabilized. To determine whether TNS influenced urinary function, we measured the pre- and post-stimulation: bladder capacity , voiding pressure , inter-contraction interval , and voiding volume . CMGs were continuously performed during all experimental procedures using LabChart software and a PowerLab data acquisition system .
Read Also: High Grade Non Invasive Bladder Cancer
Preferences For Oab Treatment: Am I Bad Enough
Regardless of whether it was self-managed or HCP-led, TTNS was strongly favoured as a management approach for OAB symptoms when positive treatment response was reported. There were opinions expressed that TTNS would need to be continued in the long-term to maintain the benefits achieved but this was seen as acceptable by the women in both groups, if symptoms were controlled.
Well they’re portable, they’re lightweight, they don’t use up a lot of energy…. there’s not really anything that would stop me from using it again
Participant 13
I do think that things have improved. I do think that this has helped. Absolutely. I’m keen to see what the next weeks bring in because I think I’m probably converted to-, to usin’ this, thereafter.
Participant 16
Even with sub-optimal treatment response, there was a perception that effects may accumulate over time and continuing for longer may prove beneficial. However, financial considerations were influential for some.
I mean, dont get me wrong, I would use it, because it didnt make me any worse, and it might have made me slightly better. So if I was given the machine, I would use it. But I dont think the improvement is big enough to actually buy one, it didnt show a massive improvement. As I was saying, I dont know if I kept going, if it might have improved me more.
Participant 5
I wouldve kept on it , but it felt.. .. the cost of it was too expensive
Participant 4
Is Percutaneous Tibial Nerve Stimulation For Overactive Bladder Effective
PTNS is an extremely effective, low-risk treatment method that can be carried out in a typical office visit. It provides impressive results within a short duration with fewer adverse effects than medications and other neuromodulation techniques. Numerous studies have revealed that four in five people undergoing this procedure experience major recovery from their overactive bladder symptoms.
However, its imperative to go through 12 weekly sessions before assessing the effect, and top-up sessions may be needed over time. Keep in mind that PTNS is a relatively newer treatment method and its lifelong benefits are not known at this time.
Also Check: Is Pumpkin Seed Oil Good For Overactive Bladder
Tns Vs Other Treatments
Behavioral therapy and medication are the preferred first-line and second-line OAB treatment options, respectively.
PTNS is a safe treatment for OAB. However, people may find it inconvenient to have to visit a doctors office regularly to complete the initial 12-week course of treatment.
When choosing an alternative to TNS, a person should consider:
- any side effects the treatment may cause
- how convenient it is to factor into their daily life
- whether scientific studies have found it to be effective
Micturition Reflex And Neuromodulation Mechanism
The brain networks that regulate continence and micturition are depicted. Urine storage reflexes. . Urine storage reflexes. . Urination reflexes the pontine micturition center .
The neuromodulation method of action in OAB treatment is not understood. However, the therapy appears to modify spinal cord reflexes and brain involvement via afferent signals rather than direct motor stimulation of the detrusor or urethral sphincter. According to the most widely recognized explanation, neuromodulations interrupt or interfere with the afferent nerve input to the sacral spinal cord, limiting detrusor overactivity and resulting in clinical alleviation of urine frequency and urgency . Electrical stimulation of the pelvic nerve, pudendal nerve sensory fibers, or muscular nerve fibers from lower limbs like the posterior tibial nerve can inhibit spinal micturition centers . Fine needles are used to stimulate the Sanyinjiao point , in which is located four fingers’ breadth above the medial malleolus . SP-6 is most likely to be the site of the tibial nerve that has been used to restore energetic harmony .
Don’t Miss: Small Cell Bladder Cancer Treatment
How Frequent Are Ptns Sessions
Peripheral Tibial Nerve Stimulation therapy is usually divided into two phases: induction and maintenance. Patients begin with induction treatment consisting of 12 weekly sessions. Most people begin to see improvement by session 6 but the full 12 sessions may be necessary for many patients to see satisfactory improvement. If the twelve induction treatments have been successful in controlling OAB symptoms, treatment then moves to a maintenance phase, which is less frequent. Treatments are typically every 3-4 weeks, though some patients are able to space these out even more. The maintenance treatments have to be maintained to continue to see the positive effects on bladder symptoms.
What Is Percutaneous Tibial Nerve Stimulation
Percutaneous tibial nerve stimulation is a minimally invasive in-office procedure that is used to treat overactive bladder for men and women. This treatment option requires 12 consecutive treatments in order for patients to experience optimum results. It can also be prescribed as maintenance after the first series of treatments are complete.
Read Also: Can A Prolapsed Bladder Cause Lower Back Pain
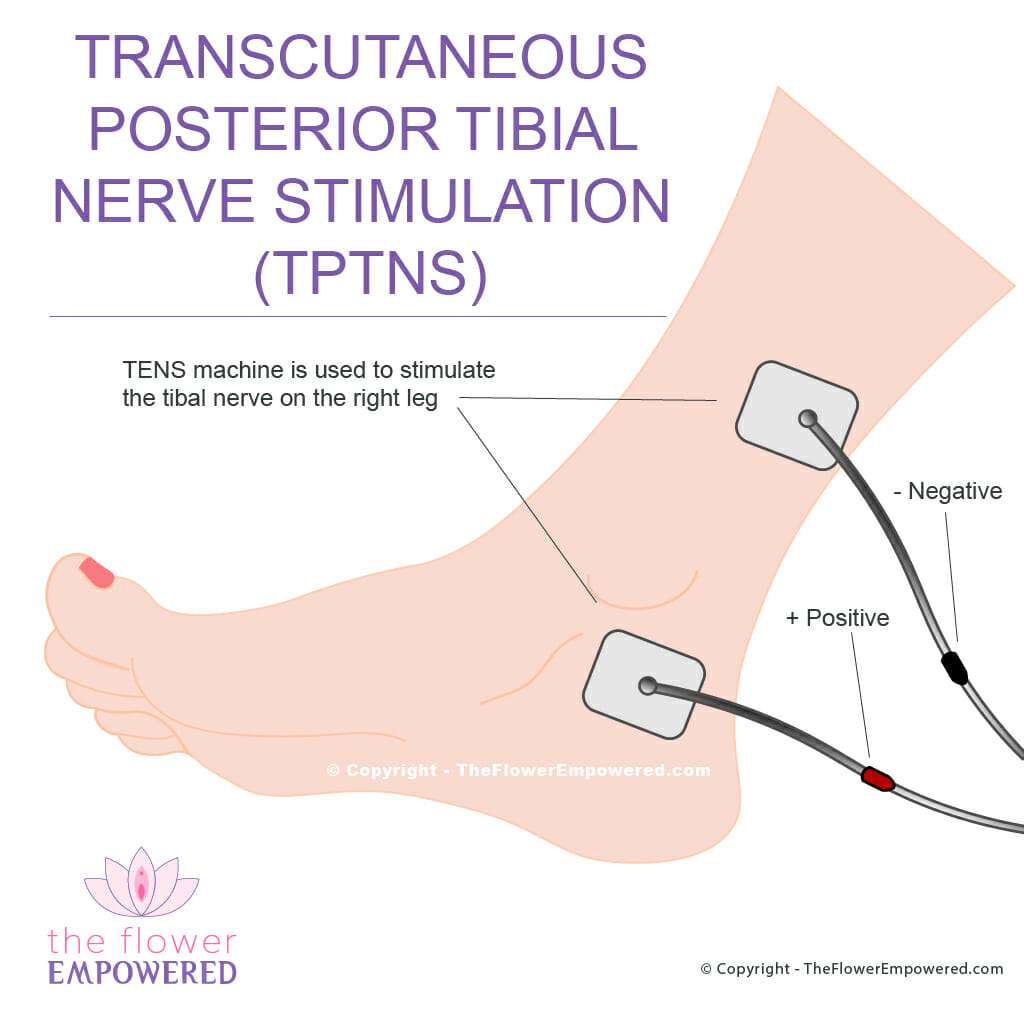
Transcutaneous Tibial Nerve Stimulation
Posterior tibial nerve stimulation is given via two 50 mm×50 mm electrode pads. The live pad is placed posterior and superior to the medial malleolus and the ground pad is placed approximately 10 cm cephalad to this. Continuous stimulation at a pulse width of 200 ls and a frequency of 10 Hz is used. The amplitude was set to produce a sensory stimulus in the ipsilateral foot, at an intensity tolerable to the patient. Stimulation is given for 30 min.
What Does It Feel Like
Since the needle is the size of an acupuncture needle, it is not painful on insertion. We can confirm that the nerve is being stimulated appropriately by observing a toe reflex response. You may feel a tingling sensation across the foot. The intensity is then adjusted so that you only feel a slight tingling and it is not uncomfortable. In fact, many women it find it relaxing to sit for the 30 minutes, undisturbed.
Also Check: Can Hair Dye Cause Bladder Cancer
Posterior Tibial Nerve Stimulation For Overactive Bladder: Mechanism Classification And Management Outlines
Xinqing ZhuDeyong Yang
1Department of Urology, First Affiliated Hospital of Dalian Medical University, Dalian 116021, China
2Department of Oncology, First Affiliated Hospital of Dalian Medical University, Dalian 116021, China
3Department of Urology, Second Affiliated Hospital of Dalian Medical University, Dalian 116021, China
4Department of Pharmacology, Pharmaceutical College, Dalian Medical University, Dalian 116044, China
5Department of Neurology, First Affiliated Hospital, Dalian Medical University, Dalian 116021, China
6Department of Biochemistry, Faculty of Science, Ibb University, Ibb, Yemen
7Healinghands Clinic, Dalian, Liaoning, China
Abstract
1. Introduction
The International Continence Society defined an overactive bladder as a syndrome characterized by urinary urgency, with or without frequency and nocturia, with or without Urgency Urinary Incontinence , in the absence of urinary tract infection or other obvious pathology .
It is a prevalent problem affecting one in every five adults aged over 40 years, with women being impacted more than men . Patients with OAB cost the US healthcare system two and half times as much as equivalent patients without OAB . Despite the detrimental effect on work, daily living, sexual function, and negative impact on the quality of life , OAB patients seeking treatment for their symptoms have been low in recent years because of its invasiveness such as surgery .
2. History of PTNS
4. Neuroanatomy of Posterior Tibial Nerve
Losing Bladder Control Is A Part Of Everyday Life
Throughout the analysis the women repeatedly referred to OAB impacting detrimentally on their lives. They talked about persistently losing control over their bladder across life situations and that living with OAB meant trying to achieve bladder control when symptoms are unpredictable and come with little warning. The loss of control they experienced included physical bladder symptoms of urgency and leakage but they also highlighted the unpredictability of when it might happen and the extent of the leakage as having a major impact across social interactions, relationships and daily activities.
The, not knowing if it will be just a dribble, a spot.. or a.. flood.
Participant 13
I am a member of admin and I’m supposed to take minutes as well and that was affectin’ me because there were times that I have to say, ‘I’m really sorry I need to nip out for a minute’. I mean I would have a table of people waiting for me to come back in again, so that could become quite embarrassing really.
Participant 10
Erm its just you know the bladder leakage. Its just a part of life. It has been for a long, long time.
Participant 7
You May Like: Causes Of Recurrent Bladder Infections
What Is Tibial Nerve Stimulation
Tibial nerve stimulation is a form of neuromodulation. This means that nerve activity is changed through electrical impulses or medication delivered straight to the nerve or a nearby area. It can be used to treat a wide variety of conditions.
To stop overactive bladder symptoms, tibial nerve stimulation targets the lower urinary tract through the posterior tibial nerve. This is a branch of your sciatic nerve that runs from your pelvis down your leg.
During tibial nerve stimulation, an electrode will be put in your lower leg, near your ankle. This electrode will send pulses to your tibial nerve during treatment.
Tibial nerve stimulation is used for overactive bladder when other treatments, such as lifestyle changes, medication, and Botox, dont work or you cant tolerate the side effects.