Risk Stratification Based On Clinical And Pathological Parameters
summarizes the available predictive models to predict recurrence and progression in patients with NMIBC. The most important risk factor for progression is grade, not stage, because patients with high-grade tumors progress with similar frequency regardless of whether they were invasive or non-invasive . Millan-Rodriguez et al. evaluated a cohort of 1529 primary NMIBC patients treated with transurethral resection and random bladder biopsy and identified prognostic factors for recurrence, progression and disease-specific mortality . Multivariate analysis demonstrated that the main prognostic factors of recurrence were multiplicity, tumor size > 3 cm, presence of CIS and treatment with bacillus CalmetteGuerin . The prognostic factors for progression were grade 3 disease, multiplicity, tumor size > 3 cm, CIS and treatment with BCG. Furthermore, the prognostic factors for mortality were presence of grade 3 disease and CIS.
Standard Treatment Options For Stage I Bladder Cancer
Patients with stage I bladder tumors are unlikely to die from bladder cancer, but the tendency for new tumor formation is high. In a series of patients with Ta or T1 tumors who were followed for a minimum of 20 years or until death, the risk of bladder recurrence after initial resection was 80%. Of greater concern than recurrence is the risk of progression to muscle-invasive, locally-advanced, or metastatic bladder cancer. While progression is rare for low-grade tumors, it is common among high-grade cancers.
One series of 125 patients with TaG3 cancers followed for 15 to 20 years reported that 39% progressed to more advanced stage disease, while 26% died of urothelial cancer. In comparison, among 23 patients with TaG1 tumors, none died and 5% progressed. Risk factors for recurrence and progression include the following:
- High-grade disease.
TUR with fulguration followed by an immediate postoperative instillation of intravesical chemotherapy
TUR and fulguration are the most common and conservative forms of management. Careful surveillance of subsequent bladder tumor progression is important. Because most bladder cancers recur after TUR, one immediate intravesical instillation of chemotherapy after TUR is widely used. Numerous randomized, controlled trials have evaluated this practice, and a meta-analysis of seven trials reported that a single intravesical treatment with chemotherapy reduced the odds of recurrence by 39% .
TUR with fulguration
Evidence :
Patient Stratification Into Risk Groups
To be able to facilitate treatment recommendations, the Guidelines Panelrecommends the stratification of patients into risk groups based on their probability ofprogression to muscle-invasive disease. The new risk group definitions provided in these EAUGuidelines are based on an IPD meta-analysis in primary patients and the calculation oftheir progression scores as presented in Sections 4.5 and6.1.2) .
For calculation of the risk group in individual patients,either one, or both, of the WHO 1973 and WHO 2004/2016 classification systems may be used.The probability of progression at 5 years varies from less than 1% to more than 40% betweenthe risk groups.
For factors where IPD were not collected such as variant histology, LVI,primary CIS and CIS in the prostatic urethra, literature data have been used to classifypatients into risk groups.
The clinical compositions of the new EAU NMIBC prognostic factor riskgroups based on the WHO 2004/2016 or WHO 1973 classification systems are provided in Table6.1. Apps for the web , iOS and Android are being developed to facilitate determining a patients risk groupin daily clinical practice. The individual probability of diseaseprogression at 1, 5 and 10 years for the new EAU NMIBC risk groups is presented in Table6.2.
Read Also: Naturvet Bladder Support Plus Cranberry
Summary Of Evidence And Guidelines Forstratification Of Non
|
Summary of evidence |
|
|
The EAU NMIBC 2021 scoring model and risk tablespredict the short- and long-term risks of disease progression in individualpatients with primary NMIBC using either the WHO 1973 or the WHO 2004/2016classification system . |
|
|
The 2006 EORTC scoring model and risk tables predictthe short- and long-term risks of disease recurrence and progression inindividual patients with NMIBC using the WHO 1973 classification system . |
|
|
Patients with TaG1/G2 tumours receiving chemotherapyhave been further stratified into three risk groups for recurrence, taking intoaccount the history of recurrences, history of intravesical treatment, tumourgrade , number of tumours and adjuvant chemotherapy . |
2a-b |
|
In patients treated with 5 to 6 months of BCG, theCUETO scoring model predicts the short- and long-term risks of diseaserecurrence and progression using the WHO 1973 classification system . |
|
|
In patients receiving at least 1 year of BCGmaintenance prior recurrence rate and number of tumours are the most importantprognostic factors for disease recurrence. Stage and grade are the mostimportant prognostic factors for disease progression and disease-specificsurvival patient age and grade are the most important prognosticfactors for overall survival . |
Summary Of Evidence And Guidelines Fortransurethral Resection Of The Bladder Biopsies And Pathology Report
|
Summary of evidence |
|
|
Transurethral resection of the bladder tumour followed by pathology investigation of the obtained specimen is an essentialstep in the management of NMIBC. |
|
|
The absence of detrusor muscle in the specimen isassociated with a significantly higher risk of residual disease and tumourunder-staging . |
|
|
In patients with a history of small Ta LG/G1 tumours,fulguration of small papillary recurrences on an outpatient basis is feasibleand safe. |
|
|
A second TURB can detect residual tumours and tumourunder-staging, increase recurrence-free survival, improve outcomes after BCGtreatment and provide prognostic information. |
Also Check: Best Supplement For Overactive Bladder
Treatment For Hg T1 Bladder Cancer With Pt0 Histology At Second Tur
TURBT followed by intravesical BCG therapy provides lower incidences of recurrence and progression than those obtained by TURBT alone . Sylvester et al. performed a meta-analysis on the efficacy of intravesical BCG therapy. They evaluated 24 trials involving a total of 4863 patients and concluded that intravesical BCG significantly reduces the risk of progression after TURBT in NMIBC patients who receive maintenance treatment. Since T1 bladder cancer is considered to be high-risk cancer regardless of the pathological findings for the second TUR specimen , various guidelines recommend full-dose intravesical BCG for 13 years except in the case of immediate cystectomy. Alternatively, mitomycin C is also recommended by the National Comprehensive Cancer Network guidelines . This is based on a meta-analysis that showed no statistically significant difference between BCG and MMC for progression and survival .
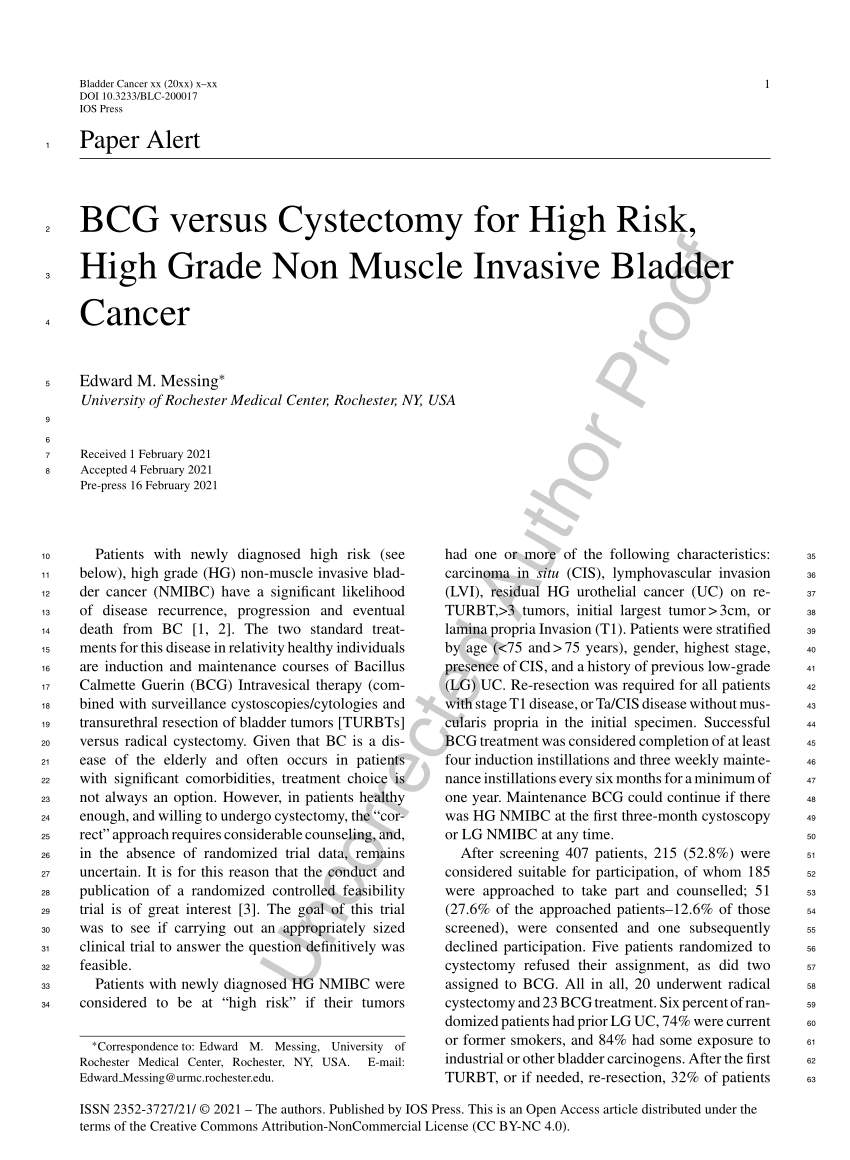
Protocol and study design of the JCOG1019 trial .
Stage Iv Bladder Cancer Treatment
Only a small fraction of patients with stage IV bladder cancer can be cured, and for many patients, the emphasis is on palliation of symptoms. The potential for cure is restricted to patients with stage IV disease with involvement of pelvic organs by direct extension or metastases to regional lymph nodes.
You May Like: Can Anxiety Cause Bladder Leakage
Treating Stage Iii Bladder Cancer
These cancers have reached the outside of the bladder and might have grown into nearby tissues or organs and/or lymph nodes . They have not spread to distant parts of the body.
Transurethral resection is often done first to find out how far the cancer has grown into the bladder wall. Chemotherapy followed by radical cystectomy is then the standard treatment.Partial cystectomy is rarely an option for stage III cancers.
Chemotherapy before surgery can shrink the tumor, which may make surgery easier. Chemo can also kill any cancer cells that could already have spread to other areas of the body and help people live longer. It can be especially useful for T4 tumors, which have spread outside the bladder. When chemo is given first, surgery to remove the bladder is delayed. The delay is not a problem if the chemo shrinks the cancer, but it can be harmful if it continues to grow during chemo. Sometimes the chemo shrinks the tumor enough that intravesical therapy or chemo with radiation is possible instead of surgery.
Some patients get chemo after surgery to kill any cancer cells left after surgery that are too small to see. Chemo given after cystectomy may help patients stay cancer-free longer, but so far its not clear if it helps them live longer. If cancer is found in nearby lymph nodes, radiation may be needed after surgery. Another option is chemo, but only if it wasn’t given before surgery.
Stage Information For Bladder Cancer
The clinical staging of carcinoma of the bladder is determined by the depth of invasion of the bladder wall by the tumor. This determination requires a cystoscopic examination that includes a biopsy and examination under anesthesia to assess the following:
- Size and mobility of palpable masses.
- Degree of induration of the bladder wall.
- Presence of extravesical extension or invasion of adjacent organs.
Clinical staging, even when computed tomographic and/or magnetic resonance imaging scans and other imaging modalities are used, often underestimates the extent of tumor, particularly in cancers that are less differentiated and more deeply invasive. CT imaging is the standard staging modality. A clinical benefit from obtaining MRI or positron emission tomography scans instead of CT imaging has not been demonstrated.
You May Like: Can You Have A Bladder Infection Without Symptoms
Tumor Recurrence And Worsening Progression Rate In Entire Patient Population
The mean age of the patients was 62.9 years and the median follow-up interval was 101.5 months . Solitary/multiple tumors were seen in 114/76 patients, respectively. Tumor recurrence occurred in 82 patients . Most patients who had tumor recurrence could be diagnosed by the routine follow-up cystoscopic examination except for 3 patients who were detected due to gross hematuria. When we divided the patients into two groups, those with or without tumor recurrence, there were no significant differences in age, gender, IVI or smoking status between the two groups . The recurrence rate in multiple tumors was significantly higher than that in solitary tumors . Univariate and multivariate analyses demonstrated that multiple tumor and absence of IVI were significant risk factors for tumor recurrence . Kaplan-Meier curves demonstrated that the 5-year recurrence free survival rate for solitary tumors was significantly higher than that for multiple tumors , and also higher for patients receiving intravesical instillation .
Table 1 Clinical characteristics of all 190 patientsFigure 2
Screening Of The Population At Risk Of Bladdercancer
The application of haematuria dipstick, followed by FGFR3, NMP22® orUroVysion tests if dipstick is positive has been reported in BC screening in high-riskpopulations . The low incidence ofBC in the general population and the short lead-time impair feasibility andcost-effectiveness . Routinescreening for BC is not recommended .
Read Also: What Can You Do For A Bladder Infection
Risk Adjusted Surveillance And Follow
Guideline Statement 32
32. After completion of the initial evaluation and treatment of a patient with NMIBC, a clinician should perform the first surveillance cystoscopy within three to four months.
Discussion
The natural history of NMIBC is often characterized by recurrence, even for solitary, small, low-grade papillary tumors. At the time of first evaluation and treatment, none of the existent risk stratification tools or urinary biomarkers is sufficiently sensitive and specific to predict which patient will have an early tumor recurrence. Therefore, the only reliable way to know in a particular patient whether they are at risk for early recurrence is by cystoscopic visualization of the urothelium at a relatively early interval after the first treatment/resection. In addition, visualization at a relatively early interval allows the treating urologist to verify that the initial resection was complete. The Panel, therefore, felt that the first repeat cystoscopic evaluation should occur three to four months after the initial treatment and evaluation, regardless of the patient’s overall risk.
Guideline Statement 33
33. For a low-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent surveillance cystoscopy six to nine months later, and then annually thereafter surveillance after five years in the absence of recurrence should be based on shared-decision making between the patient and clinician.
Discussion
Discussion
Computed Tomography Urography And Intravenousurography
Computed tomography urography is used to detect papillary tumours inthe urinary tract, indicated by filling defects and/or hydronephrosis .
Intravenous urography is an alternative if CT isnot available , but particularly in muscle-invasivetumours of the bladder and in UTUCs, CT urography provides more information .
The necessity to perform a baseline CT urography once abladder tumour has been detected is questionable due to the low incidence of significantfindings obtained . The incidence of UTUCs is low, but increases to 7.5% in tumours located in the trigone . The risk of UTUC during follow-up increases in patients with multiple- andhigh-risk tumours .
Also Check: Over The Counter Bladder Medication
Treatment For Hg Pt1 Bladder Cancer With Pt2 Or More Histology At Second Tur
There is no doubt about the need to perform radical cystectomy for patients with muscle-invasive disease at the second TUR. Most of these tumors are understaged at the initial TURBT due to technical problems, and may not be large or bulky like muscle-invasive tumors that are diagnosed at the initial TURBT and/or with computed tomography or magnetic resonance imaging. The discussion on the treatment strategies for these tumors does not include whether cystectomy should be performed but whether neoadjuvant chemotherapy and/or extended lymph node dissection should be performed.
Several randomized Phase III trials and meta-analyses demonstrated the survival benefit of cisplatin-based neoadjuvant chemotherapy for patients with MIBC. However, whether neoadjuvant chemotherapy prolongs the survival of patients with T1 cancer at the initial TURBT and with muscle-invasive disease detected by a second TUR is unclear. Neoadjuvant chemotherapy offers potential advantages in tumor downstaging and eradication of micrometastases, so this therapy should be indicated for patients who have risk factors for locally advanced disease or nodal metastasis.
Strategy Of The Procedure
The goal of TURB in TaT1 BC is to make the correct diagnosis and completelyremove all visible lesions. It is a crucial procedure in the management of BC. Transurethralresection of the bladder should be performed systematically in individual steps .
The operative steps necessary to achieve a successful TURB includeidentifying the factors required to assign disease risk , clinical stage , adequacy of the resection , and presence of complications . To measure the size of thelargest tumour, one can use the end of cutting loop, which is approximately 1 cm wide as areference. The characteristics of the tumour are described as sessile, nodular, papillary orflat.
You May Like: Bladder Problems After Endometrial Ablation
Role Of Cystectomy In Nmibc
Guideline Statement 27
27. In a patient with Ta low- or intermediate-risk disease, a clinician should not perform radical cystectomy until bladder-sparing modalities have failed.
Discussion
Low-grade, noninvasive tumors very rarely metastasize, and even large-volume, multifocal cancers can usually be managed with techniques, such as staged resection. Patients with low-grade recurrences can be successfully managed with intravesical chemotherapy 225 or BCG. 177,226,227 In addition, small, multifocal recurrences despite intravesical therapy can usually be treated effectively with office fulguration, repeat TURBT or even surveillance, in select cases. 64-67
Guideline Statement 28
28. In a high-risk patient who is fit for surgery with persistent high-grade T1 disease on repeat resection, or T1 tumors with associated CIS, LVI, or variant histologies, a clinician should consider offering initial radical cystectomy.
Discussion
Guideline Statement 29
29. In a high-risk patient with persistent or recurrent disease within one year following treatment with two induction cycles of BCG or BCG maintenance, a clinician should offer radical cystectomy.
Durvalumab And Vicineum In Subjects With High
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government.Know the risks and potential benefits of clinical studies and talk to your health care provider before participating. Read our disclaimer for details. |
| First Posted : August 23, 2017Last Update Posted : February 10, 2022 |
- Study Details
Background:
Non-muscle-invasive bladder cancer is in the early stages. But it usually comes back after treatment. The drugs Vicineum and Durvalumab may help the immune system find and destroy cancer cells.
Objective:
To test if the drugs Durvalumab and Vicineum together are safe and effective to treat people with bladder cancer that has not spread to the muscle in the bladder.
Eligibility:
People ages 18 and older who have bladder cancer that has not spread to the muscle in the bladder and was treated unsuccessfully with Bacillus Calmette-Guerin
Design:
Participants will be screened with:
Medical history
Physical exam
Blood and urine tests
Tumor sample from previous surgery. If one is not available, they will have a biopsy: A small piece of tumor is removed.
Cystoscopy to examine the inside of the bladder. This may include a biopsy or removing tumors.
CT or MRI: They lie in a machine that takes pictures of the body.
Electrocardiogram to test heart function
Participants will receive Durvalumab and Vicineum in 2 phases:
Objectives:
Recommended Reading: Can Too Much Sugar Cause A Bladder Infection
Theimpact Of Second Resection On Treatment Outcomes
A second TURB can increase recurrence-free survival , improve outcomes afterBCG treatment and provide prognostic information .
In a retrospective evaluation of a largemulti-institutional cohort of 2,451 patients with BCG-treated T1G3/HG tumours , the second resection improved RFS,progression-free survival and overall survival only in patients without detrusormuscle in the specimen of the initial resection .
Individual Treatment Strategy In Primary Orrecurrent Tumours After Turb Without Previous Bcg Intravesical Immunotherapy
The type of further therapy after TURB should be based on the risk groupsshown in Section 6.3 and Table 6.1. The stratification and treatment recommendations arebased on the risk of disease progression. In particular in intermediate-risk tumours, the2006 EORTC scoring model may be used to determine a patientsindividual risk of disease recurrence as the basis to decide further treatment on.
Any decisions should reflect the following principles :
- Patients in the low-risk group have a negligible risk of disease progression. The singlepost-operative instillation of chemotherapy reduces the risk of recurrence and isconsidered as sufficient treatment in these patients.
- Patients in the intermediate-risk group have a low risk of disease progression . In these patientsone-year full-dose BCG treatment , or instillations of chemotherapy for amaximum of one year, is recommended. The final choice should reflect the individualpatients risk of recurrence and progression as well as the efficacy and sideeffects of each treatment modality.
- Patients in the high-risk group have a high risk of disease progression . In these patientsfull-dose intravesical BCG for one to three years , is indicated. The additional beneficial effectof the second and third years of maintenance should be weighed against its added costs,side-effects and problems connected with BCG shortage.
Figure 7.1: Treatment strategy in primary or recurrent tumourwithout previous BCG*
Recommended Reading: Does Bactrim Treat Bladder Infection