Figo Stages For Cervical Cancer
Doctors assign the stage of the cancer by evaluating the tumor and whether the cancer has spread to other parts of the body.
Staging is based on the results of a physical exam, imaging scans, and biopsies.
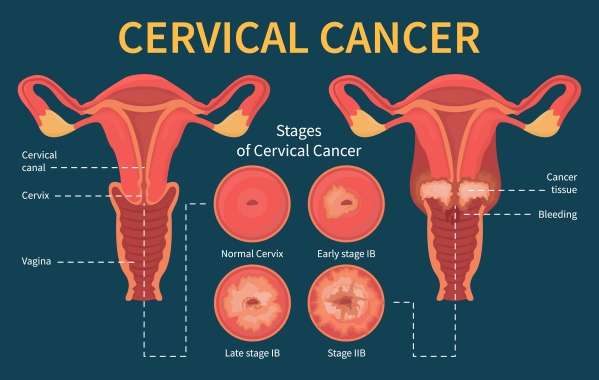
Stage I: The cancer has spread from the cervix lining into the deeper tissue but is still just found in the uterus. It has not spread to other parts of the body. This stage may be divided into smaller groups to describe the cancer in more detail .
-
Stage IA: The cancer is diagnosed only by viewing cervical tissue or cells under a microscope. Imaging tests or evaluation of tissue samples can also be used to determine tumor size.
-
Stage IA1: There is a cancerous area of less than 3 millimeters in depth.
-
Stage IA2: There is a cancerous area 3 mm to less than 5 mm in depth.
Stage IB:In this stage, the tumor is larger but still only confined to the cervix. There is no distant spread.
Stage IB1: The tumor is 5 mm or more in depth and less than 2 centimeters wide. A centimeter is roughly equal to the width of a standard pen or pencil.
Stage IB2: The tumor is 5 mm or more in depth and between 2 and 4 cm wide.
Stage IB3: The tumor is 4 cm or more in width.
Stage II: The cancer has spread beyond the uterus to nearby areas, such as the vagina or tissue near the cervix, but it is still inside the pelvic area. The cancer has not spread to other parts of the body. This stage may be divided into smaller groups to describe the cancer in more detail .
Pelvic Lymph Node Dissection
Cancer that starts in the cervix can spread to lymph nodes in the pelvis. To check for lymph node spread, the surgeon might remove some of these lymph nodes. This procedure is known as a pelviclymph node dissection or lymph node sampling. It is done at the same time as a hysterectomy or trachelectomy.
Removing lymph nodes can lead to fluid drainage problems in the legs. This can cause severe leg swelling, a condition called Lymphedema.
Who’s Affected By Cervical Cancer
Following the success of the NHS Cervical Screening Programme and the early detection of cell changes, the number of cervical cancer cases in the UK has reduced. Around 3,000 cases of cervical cancer are diagnosed in the UK each year.
It’s possible for women of all ages to develop cervical cancer, but the condition mainly affects sexually active women aged between 30 and 45. Cervical cancer is very rare in women under 25.
Recommended Reading: What Does The Start Of A Bladder Infection Feel Like
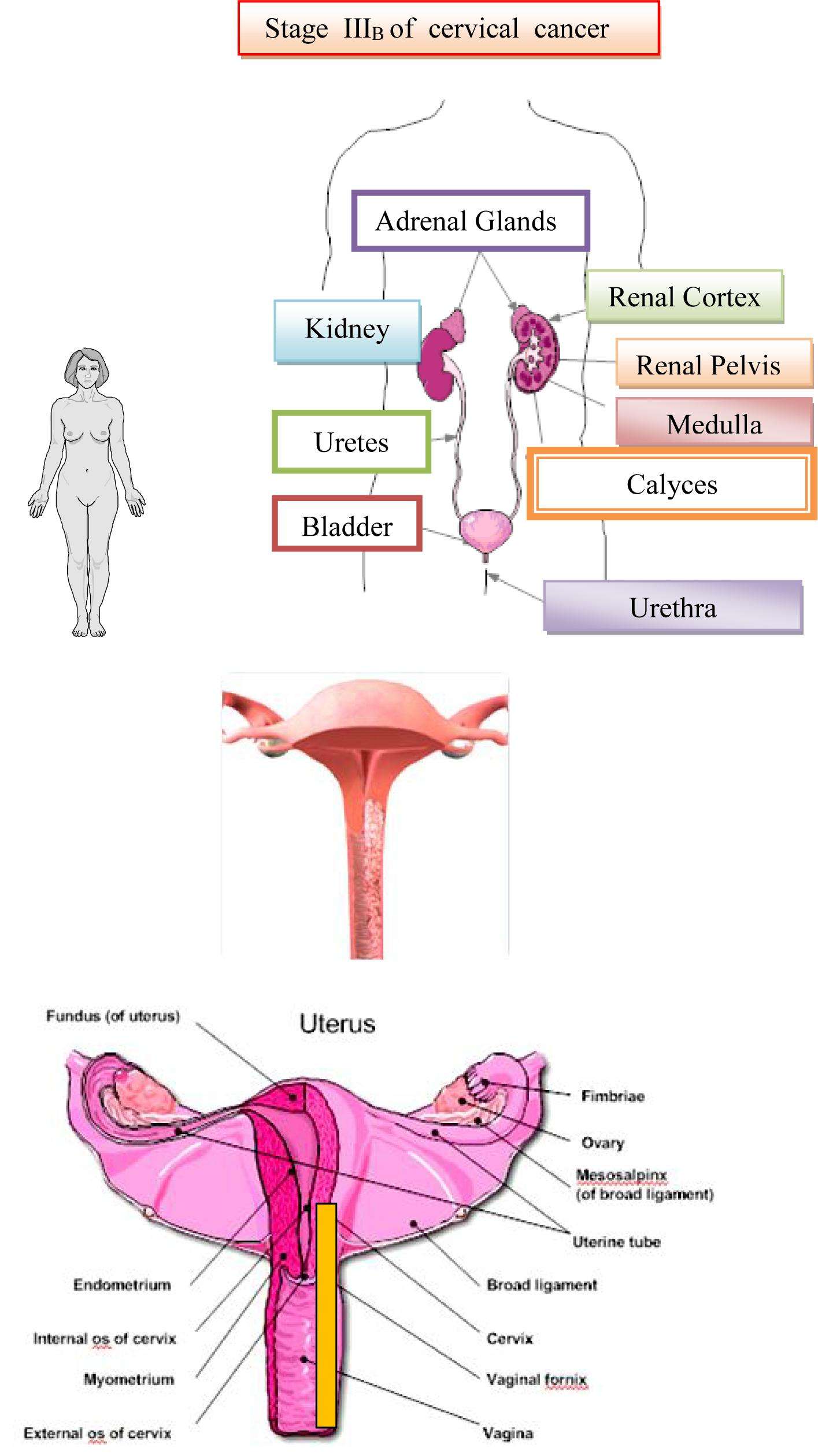
Stage : Cancer Has Spread Beyond The Uterus/cervix To The Vagina Ovaries Fallopian Tubes And/or Lymph Nodes In The Pelvis Or Abdomen
Stage 3 is subdivided into the following:
- Stage 3A: Cancer is in the outer layer of your uterus or the fallopian tubes and ovaries.
- Stage 3B: It has spread to the tissues around the uterus or vagina.
- Stage 3C1: The cancer has spread outside of the uterus and to the lymph nodes of the pelvis.
- Stage 3C2: Cancer cells are inside the body of the uterus and the lymph nodes of the higher aorta.
In Stage 3, in addition to unusual vaginal bleeding, you may experience discomfort or pain in the abdomen, bloating, feeling full quickly, and difficulty or pain urinating.
Symptoms Of Advanced Cancer
Advanced cervical cancer means that a cancer that began in the cervix has spread to another part of the body.
Symptoms depend on where the cancer is in the body. They might include:
- tiredness and feeling unwell
- griping pain in your tummy
- feeling bloated
- constipation
- vomiting large amounts
It might not mean that you have advanced cancer if you have these symptoms. They can be caused by other conditions.
Tell your doctor or specialist nurse if you’re worried about a symptom or if it continues for more than a few days.
Recommended Reading: Small Cell Bladder Cancer Survival Rate
Mechanisms Of Tumor Spread
The mechanisms and pathways by which malignant tumors of the abdomen and pelvis spread are determined by regional anatomy and tumor pathophysiology. Abdominal and pelvic organs are suspended in the peritoneal cavity by ligaments and mesenteries formed by the peritoneum as it reflects from the extraperitoneal surface. The abdominal ligaments and mesenteries serve as conduits through which blood vessels, nerves, and lymphatics may travel. They also may serve to facilitate tumor spread between organs or restrict tumor spread between compartments. A variety of descriptions are in common usage regarding the mechanisms of tumor spread. Tumors can spread in several ways: directly from organ to organ without regard for fascial planes or anatomic compartments via the subserous connective tissue, blood vessels, or lymphatics of the abdominal mesenteries and ligaments or throughout the peritoneal cavity. Chapter 6 provides additional information regarding the spread of disease within the abdomen and pelvis.
Direct Contiguous Spread
Subperitoneal Spread
The intraperitoneal organs are suspended within the peritoneal cavity and are interconnected via a scaffolding of supporting ligaments and mesenteries. Beneath the peritoneal lining lies the subperitoneal space. This space contains connective tissue, lymphatics, and blood vessels, all of which can serve as conduits for tumor spread.
Subperitoneal Tumor Extension
Lymphatic Spread
BENIGN VERSUS MALIGNANT LYMPH NODES
Hematogenous Spread
Urinary Outcome And Fistula Formation
A total of 23 patients had VVF in their disease history. Eight patients had VVF prior to any treatment and four of them without urinary symptoms received brachytherapy. VVF disappearance was observed in two of them: one at 18 Gy of RT , and one six months after BT . Among the 63 patients without VVF prior to treatment, 15/63 developed VVF during follow-up, with 13/15 occurring the year following the start of radiotherapy . Median time to onset was 3.1 months after the start of EBRT . Six out of 15 VVFs were associated with local relapse, while nine patients out of the 48 patients with no VVF at diagnosis and no local relapse, developed a VVF which were therefore considered as complications.
Eleven of the 23 patients with VVF underwent surgery related to VVF: anterior pelvectomy + cutaneous uretero-ileostomy , isolated cutaneous uretero-ileostomy , continent ileocolonic urinary reservoir , total pelvectomy , VVF repair . Five patients also had a colostomy for associated recto-vaginal fistulae or severe digestive symptoms. At the last follow-up, 12/23 patients had no urinary symptom, while five still experienced repeated urinary tract infections or dribbling.
You May Like: Types Of Bladder Cancer Treatments
Tests For Cervical Cancer Staging
To determine the stage, doctors may use the following tests, or a combination of these procedures:
- Positron emission tomography scan
- Magnetic resonance imaging
- Ultrasound exam
- Chest X-ray
Your care team may also need to perform a procedure to collect more information about the cancer. These may include:
What Are The Treatment Options For Bladder Cancer
There are four types of treatment for patients with bladder cancer. These include:
- Surgery
Sometimes, combinations of these treatments will be used.
Surgical options
Surgery is a common treatment option for bladder cancer. The type of surgery chosen will depend on the stage of the cancer.
- Transurethral resection of the bladder is used most often for early stage disease . It is done under general or spinal anesthesia. In this procedure, a special telescope called a resectoscope is inserted through the urethra into the bladder. The tumor is then trimmed away with the resectoscope, using a wire loop, and the raw surface of the bladder is then fulgurated .
- Partial cystectomy is the removal of a section of the bladder. At times, it is used for a single tumor that invades the bladder wall in only one region of the bladder. This type of surgery retains most of the bladder. Chemotherapy or radiation therapy is often used in combination. Only a minority of patients will qualify for this bladder-sparing procedure.
- Radical cystectomy is complete removal of the bladder. It is used for more extensive cancers and those that have spread beyond the bladder .
This surgery is often done using a robot, which removes the bladder and any other surrounding organs. In men, this is the prostate and seminal vesicles. In women, the ovaries, uterus and a portion of the vagina may be removed along with the bladder.
Chemotherapy
- Methotrexate
Intravesical therapy
Radiation therapy
Don’t Miss: Kegel Exercises For Bladder Control
What Stages Have To Do With Cancer Spread
Cancers are staged according to tumor size and how far it has spread at the time of diagnosis. Stages help doctors decide which treatments are most likely to work and give a general outlook.
There are different types of staging systems and some are specific to certain types of cancer. The following are the basic stages of cancer:
- In situ. Precancerous cells have been found, but they havent spread to surrounding tissue.
- Localized. Cancerous cells havent spread beyond where they started.
- Regional. Cancer has spread to nearby lymph nodes, tissues, or organs.
- Distant. Cancer has reached distant organs or tissues.
- Unknown. Theres not enough information to determine the stage.
- Stage 0 or CIS. Abnormal cells have been found but have not spread into surrounding tissue. This is also called precancer.
- Stages 1, 2, and 3. The diagnosis of cancer is confirmed. The numbers represent how large the primary tumor has grown and how far the cancer has spread.
- Stage 4. Cancer has metastasized to distant parts of the body.
Your pathology report may use the TNM staging system, which provides more detailed information as follows:
T: Size of primary tumor
- TX: primary tumor cant be measured
- T0: primary tumor cant be located
- T1, T2, T3, T4: describes the size of the primary tumor and how far it may have grown into surrounding tissue
N: Number of regional lymph nodes affected by cancer
M: Whether cancer has metastasized or not
Does Cervical Cancer Spread Fast
After diagnosis, many patients have the question, Does Cervical Cancer Spread Fast?. In most cases, cervical cancer is a slow growing disease. However, the various types of cervical cancer can behave differently, with some more aggressive than others. Roughly 90% of cases are identified as squamous cell carcinoma. The rest of the cases are labeled as Adenocarcinoma. Approximately 200 of the over 11,000 total cases diagnosed in the United States each year will be classified as small cell cervical cancer or large cell cervical cancer, both aggressive variants. Every patient is different, some precancerous cells in the cervix can be present for several years before developing into cancer.
Cervical cancer starts as precancer in the cells on the cervix floor. Untreated cervical cancer can spread to the bladder, intestines, lymph nodes, bones, lungs, and liver. Cervical cancer happens when cells in the cervix develop and divide uncontrollably. Unlike many different cancers whose causes are largely still unknown, cervical cancer is most frequently attributable to human papillomavirus .
Read Also: Bladder Cancer Metastasis To Liver Prognosis
What Are Stage 4 Cervical Cancer Treatments
Because stage 4 cervical cancer is advanced, the treatments are more aggressive. However, if you decide that you do not want to undergo the above treatments, there are options for palliative care to improve your quality of life. These options include:
- Chemoradiation
- For stage 4A cervical cancer, both chemotherapy and radiation are given. The chemotherapy drug or drugs are delivered every 4 weeks to make radiation therapy more effective. Brachytherapy can also supplement the EBRT.
Figuring Out Your Stage
Doctors use two ways to decide the stage of uterine cancer. One is a method created by the International Federation of Gynecology and Obstetrics . The other is the American Joint Committee of Cancer TNM staging system. The two methods are almost the same.
Both systems are based on three categories: tumor, lymph nodes, and metastasis . In the TNM staging system, the categories are assigned letters:
Tumor . How big is the main tumor, and has it spread to nearby organs?
Lymph nodes . Has the disease moved into nearby lymph nodes? These are the small, bean-shaped glands found throughout the body that are part of your immune system — your body’s defense against germs.
Metastasis . Has the cancer spread to far-away lymph nodes or other organs? This is called metastasis.
In TMN staging, doctors also assign numbers after the letters T, M, N that explain how advanced your cancer is.
Once your doctor works out the TMN staging, they’ll also figure out a broader set of stages that use Roman numerals. There are four stages of endometrial cancer: I, II, III, and IV.
Lower numbers mean that the cancer hasn’t spread as much. If you have stage IV, the cancer cells have spread to parts of the body that are farther away.
Also Check: Home Remedies For A Uti Or Bladder Infection
How Is Metastatic Uterine Cancer Treated
Treatment of metastatic uterine cancer requires the expertise of a multispecialty team that has a high level of experience with this malignancy such as the specialists at Moffitt Cancer Center. Our team collaborates as a tumor board, ensuring every Moffitt patient with metastatic uterine cancer receives a treatment plan tailored to her unique needs. Additionally, Moffitt is at the forefront of cancer research and offers a number of clinical trials that patients may be eligible to participate in. These clinical trials provide access to the latest and most advanced treatments before they have been made widely available. Virtual visits appointments are also available.
Symptoms If Cancer Has Spread To The Lymph Nodes
Lymph nodes are part of a system of tubes and glands in the body that filters body fluids and fights infection.
The most common symptom that happens when cancer spreads to the lymph nodes, is that they feel hard or swollen. Cervical cancer can spread to lymph nodes in the area between the hip bones .
Cancer cells can also stop lymph fluid from draining away. This might lead to swelling in your legs due to fluid build up. The swelling is called lymphoedema.
Symptoms if cancer has spread to the liver
You might have any of these symptoms if the cancer has spread to your liver:
- discomfort or pain on the right side of your abdomen
- feeling sick
- poor appetite and weight loss
- swollen abdomen
- yellowing of the skin
- itchy skin
Symptoms if cancer has spread to the bones
Cervical cancer may spread to the bones. The most common symptom if cancer has spread to the bone is bone pain. It is usually there most of the time and wakes you up at night. It can be a dull ache or stabbing pain.
Your bones might also become weaker and more likely to break .
Having bone pain does not mean that your cancer has definitely spread to the bones. There may be other reasons for your bone pain. Speak to your doctor or nurse if you are worried.
Read Also: Best Antibiotic To Treat Bladder Infection
What Causes Cervical Cancer And Am I At Risk
Cervical cancer is much more common in developing nations than it is in developed nations. Cervical cancer is the 2nd most common cause of cancer death in developing nations, with 84% of all cervical cancer cases occurring in Africa, Latin American, and Caribbean underdeveloped areas. It is fairly rare in the United States. Every year, an estimated 13,800 cases of cervical cancer are diagnosed in the United States. There has been a 75% decrease in deaths from cervical cancer in developed nations over the past 50 years. Most of this decrease is attributed to the effective institution of cervical cancer screening programs in developed nations.
One of the most important risk factors for cervical cancer is infection with a virus called HPV . It should be stressed that only a very small percentage of women who have HPV will develop cervical cancer. Just because you have HPV doesn’t mean you will get cancer. However, almost all cervical cancers have evidence of the HPV virus in them, so HPV infection is a major risk factor for developing it. HPV is a sexually transmitted infection that is incredibly common in the population. In fact, most college-aged men and women have been exposed to HPV.
Because having an STI is a risk factor for cervical cancer, any risk factor for developing STIs is also a risk factor for developing cervical cancer. These include:
What Is Cervical Cancer
Cervical cancer occurs when previously healthy cells in the cervix become abnormal. As they grow, they crowd healthy cells. If the abnormal cells spread to other areas of the body, it makes it harder for the body to function correctly.
Cervical cancer used to be one of the most common causes of cancer death for American women. Fortunately, because of the Pap test, rates of cervical cancer have dropped dramatically. During a Pap test, your doctor collects cervical cells for microscopic examination to find precancerous or cancerous cells. A Pap test is typically done every 3 to 5 years in your healthcare providers office unless you are at an increased risk for cervical cancer. It is crucial to catch cancer early, and routine cervical cancer screening allows most women to do that.
You May Like: How To Reduce Bladder Inflammation Naturally
What Screening Tests Are Used For Cervical Cancer
Cervical cancer is considered a preventable disease. It usually takes a very long time for pre-cancerous lesions to progress to invasive cancers. Effective screening programs in the United States have led to the drastic decline in the numbers of cervical cancer deaths in the last 50 years. For women who do develop cervical cancer in developed nations, 60% of them either have never been screened or haven’t been screened in the last five years. The importance of regular cervical cancer screening cannot be overstated.
The mainstay of cervical cancer screening has been the Pap test. Pap is short for Papanicolaou, the inventor of the test, who published a breakthrough paper in 1941. A Pap test is easily performed in your provider’s office. During a pelvic examination, your provider uses a wooden spatula and/or a brush to get samples of cervical cells. These cells are placed on a slide, or in a liquid preservative, and sent to a laboratory where an expert in examining cells under a microscope can look for cancerous changes. Many women find the exam uncomfortable, but rarely painful. Depending on the results of the test, your provider may need to perform further examinations.
The American Cancer Society recommends the following guidelines for cervical cancer screening: