Thyroid Transcription Factor 1
Thyroid transcription factor 1 is a 38-kDa homeodomain-containing transcription factor. It is expressed in the nuclei of thyroid follicular cells, certain lung cells , and cells in the diencephalon area of the brain. TTF-1 has been identified by immunohistochemistry in most SmCC and adenocarcinomas of the lung and in follicular cell-derived thyroid tumors. It was once proposed as a specific marker to determine the origin of metastasis from those tumor types. However, the once-alleged specificity of TTF-1 for lesions of pulmonary and thyroid origin has been increasingly questioned. A case series in 2001 found TTF-1 positivity in 42% of extrapulmonary SmCC cases, including 2 bladder primaries. It was thus concluded that TTF-1 was not reliable for use in determining the primary site of SmCC. Nonetheless, TTF-1 is still useful for the differential diagnosis of extracutaneous SmCC metastasis to the skin versus primary Merkel cell carcinoma of the skin because most studies have confirmed that Merkel cell carcinoma is consistently negative for TTF-1.
Bladder Cancer/small Cell Bladder Cancer
Anyone here been diagnosed with small cell bladder cancer. I had a cystectomy in later February and was told that all visible cancer had been removed. Today at a 2nd opinion session at the Mayo I learned that the original diagnosis missed the fact that I have small cell bladder cancer. Im in shock that the original pathology work missed this. I will be starting chemo ASAP. I know the outlook is not good and Im looking for some positive threads to hold onto. Thanks
Hello . Sorry to hear about your second diagnosis. Im a bladder cancer survivor of 8 years, but until you raised the possibility, didnt know about the possibility of Small Cell Carcinoma of the Bladder . Im due for my annual cystoscopy in 5 weeks with a new urologist, and I will start my relationship with him through a discussion about SCCB.
We may not find another member of Mayo Connect with your diagnosis, given the fact that it is extremely rare . So be sure that I will get back to you here after my cystoscopy next June 8 so we can have a discussion about what I have learned. Feel free to get back to me much sooner than that we can start the discussion as soon as youre willing. Meantime, my initial research turned up two web sites you may find interesting:
Treating Stage Iv Bladder Cancer
These cancers have reached the pelvic or abdominal wall , may have spread to nearby lymph nodes , and/or have spread to distant parts of the body . Stage IV cancers are very hard to get rid of completely.
Chemotherapy is usually the first treatment if the cancer has not spread to distant parts of the body . The tumor is then rechecked. If it appears to be gone, chemo with or without radiation or cystectomy are options. If there are still signs of cancer in the bladder, chemo with or without radiation, changing to another kind of chemo, trying an immunotherapy drug, or cystectomy may be recommended.
Chemo is typically the first treatment when bladder cancer has spread to distant parts of the body . After this treatment the cancer is rechecked. If it looks like it’s gone, a boost of radiation to the bladder may be given or cystectomy might be done. If there are still signs of cancer, options might include chemo, radiation, both at the same time, or immunotherapy.
In most cases surgery cant remove all of the cancer, so treatment is usually aimed at slowing the cancers growth and spread to help people live longer and feel better. If surgery is a treatment option, it’s important to understand the goal of the operation whether it’s to try to cure the cancer, to help a person live longer, or to help prevent or relieve symptoms from the cancer.
Because treatment is unlikely to cure these cancers, many experts recommend taking part in a clinical trial.
Recommended Reading: Bladder Leakage Only At Night
Dll3 As A Therapeutic Target
The molecular analysis of SCBC led to the discovery of several important prognostic and predictive factors. For instance, tumors with DLL3 protein expression of greater than 10 percent were associated with shorter OS and PFS from diagnosis and shorter OS from surgery. To test whether DLL3 might serve as a therapeutic target, a DLL3-targeting antibody-drug conjugate was tested in a patient-derived xenograft model and was found to be highly effective in models of SCBC derived from otherwise highly resistant tumors. This exciting finding could lead to a new generation of promising clinical trials in SCBC.
This study is the first to assess prognostic value in proteins associated with neuroendocrine differentiation and is one of the largest of gene expression profiling in SCBC.
More information at mianlab.org
Image: Originally published as Figure 5 in above-referenced article. DLL3 IHC of FFPE sample of a SCBC patient-derived xenograft model and isotype control of same FFPE sample showing lack of staining .
In Most Cases Localized Small
The small-cell undifferentiated or anaplastic variant of bladder cancer presents a challenging clinical problem, both because of its rarity and the consequent paucity of level I data to guide treatment paradigms. Representing only 1% to 2% of incident bladder cancers, depending on the site of reporting, this entity is most likely the product of a stem cell tumor, with differentiation along an unusual pathway. We have previously modeled the existence of a bladder cancer stem cell, demonstrating preclinically and clinically its potential to differentiate along varied pathways, most commonly glandular or squamous. There is extensive evidence to support the common clonal origin of small-cell bladder cancer and urothelial cancer. The fundamental biology of SCBC has not yet been elucidated, although the general consensus is that it is a smoking-related disorder, with common aberrant patterns of chromosomes and gene expression, as well as presence of neuroendocrine biochemical markers. If this tumor does not have a stem cell origin, it most likely represents de-differentiation from the scattered neuroendocrine cells in the bladder wall.
Metastatic SCBC
Clinically Localized SCBC: Conventional Approaches
It has conventionally seemed very attractive to avoid the mutilation and morbidity of cystectomy in the context of a relatively poor potential for cure, and thus an emphasis has been placed on radiotherapy alone, chemotherapy alone, or combinations of the two.
You May Like: How To Relieve Bladder Infection
Squamous Cell Carcinoma Of The Bladder
Squamous cell carcinoma is the second most common type of bladder cancer. It accounts for about 5 percent of bladder cancers in North America and Europe. This cancer begins in the thin, flat squamous cells that may form in the bladder after chronic inflammation and infection. Squamous cell carcinoma is most often found in parts of the world where a parasitic infection called schistosomiasis is widespread, such as the Middle East.
What Is Bladder Cancer
Bladder cancer starts when cells that make up the urinary bladder start to grow out of control. As more cancer cells develop, they can form a tumor and, with time, spread to other parts of the body.
The bladder is a hollow organ in the lower pelvis. It has flexible, muscular walls that can stretch to hold urine and squeeze to send it out of the body. The bladder’s main job is to store urine. Urine is liquid waste made by the 2 kidneys and then carried to the bladder through 2 tubes called ureters. When you urinate, the muscles in the bladder contract, and urine is forced out of the bladder through a tube called the urethra.
You May Like: What To Do If You Have A Bladder Infection
Other Potential Therapeutic/prognostic Markers
Tumor protein 53 is a tumor suppressor protein crucial in multicellular organisms. It regulates the cell cycle and conserves genomic stability, thus its alias as the guardian of the genome. p53 gene mutation represents the most common genetic alteration in human neoplasias and has been associated with high grade, high stage, and poor prognosis in a variety of malignancies, including those of the lung, breast, stomach, prostate, and urinary bladder. The protein product of mutant p53 gene is significantly more stable than the wild type and subsequently accumulates in the cells, manifested as p53 overexpression on immunostaining. Multiple case series on bladder SmCC have documented p53 overexpression, ranging from 37.5% to 80% of the cases studied in individual series. The largest series to date demonstrated a p53 overexpression rate at 54% of bladder SmCC cases. This case series revealed no definite correlation between p53 overexpression and poorer prognosis, possibly because the overall prognosis for bladder SmCC is poor, regardless of various clinicopathologic parameters.
Proto-oncoprotein c-kit is involved in many physiologic and pathologic processes, including hematopoiesis and oncogenesis. Its sensitivity in bladder SmCC cases is rather low, demonstrated at 27% and 28% in 2 case series. Despite its limited value in establishing a diagnosis of bladder SmCC, c-kit may be a worthwhile therapeutic target in a subset of patients with this disease.
Prognosis And Survival For Bladder Cancer
If you have bladder cancer, you may have questions about your prognosis. A prognosis is the doctors best estimate of how cancer will affect someone and how it will respond to treatment. Prognosis and survival depend on many factors. Only a doctor familiar with your medical history, the type and stage and other features of the cancer, the treatments chosen and the response to treatment can put all of this information together with survival statistics to arrive at a prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person that the doctor will consider when making a prognosis. A predictive factor influences how a cancer will respond to a certain treatment. Prognostic and predictive factors are often discussed together. They both play a part in deciding on a treatment plan and a prognosis.
The following are prognostic and predictive factors for bladder cancer.
Recommended Reading: Can Overactive Bladder Start Suddenly
Treating Stage Iii Bladder Cancer
These cancers have reached the outside of the bladder and might have grown into nearby tissues or organs and/or lymph nodes . They have not spread to distant parts of the body.
Transurethral resection is often done first to find out how far the cancer has grown into the bladder wall. Chemotherapy followed by radical cystectomy is then the standard treatment.Partial cystectomy is rarely an option for stage III cancers.
Chemotherapy before surgery can shrink the tumor, which may make surgery easier. Chemo can also kill any cancer cells that could already have spread to other areas of the body and help people live longer. It can be especially useful for T4 tumors, which have spread outside the bladder. When chemo is given first, surgery to remove the bladder is delayed. The delay is not a problem if the chemo shrinks the cancer, but it can be harmful if it continues to grow during chemo. Sometimes the chemo shrinks the tumor enough that intravesical therapy or chemo with radiation is possible instead of surgery.
Some patients get chemo after surgery to kill any cancer cells left after surgery that are too small to see. Chemo given after cystectomy may help patients stay cancer-free longer, but so far its not clear if it helps them live longer. If cancer is found in nearby lymph nodes, radiation may be needed after surgery. Another option is chemo, but only if it wasn’t given before surgery.
Treating Stage Ii Bladder Cancer
These cancers have invaded the muscle layer of the bladder wall , but no farther. Transurethral resection is typically the first treatment for these cancers, but it’s done to help determine the extent of the cancer rather than to try to cure it.
When the cancer has invaded the muscle, radical cystectomy is the standard treatment. Lymph nodes near the bladder are often removed as well. If cancer is in only one part of the bladder, a partial cystectomy may be done instead. But this is possible in only a small number of patients.
Radical cystectomy may be the only treatment for people who are not well enough to get chemo. But most doctors prefer to give chemo before surgery because it’s been shown to help patients live longer than surgery alone. When chemo is given first, surgery is delayed. This is not a problem if the chemo shrinks the bladder cancer, but it might be harmful if the tumor continues to grow during chemo.
If cancer is found in nearby lymph nodes, radiation may be needed after surgery. Another option is chemo, but only if it wasn’t given before surgery.
For people who have had surgery, but the features of the tumor show it is at high risk of coming back, the immunotherapy drug, nivolumab, might be offered. When given after surgery, nivolumab is given for up to one year.
For patients who cant have surgery because of other serious health problems, TURBT, radiation, chemotherapy, or some combination of these may be options.
Read Also: Why Do I Get A Bladder Infection After Intercourse
Cancer That Has Spread To The Bladder
Sometimes cancer that has started elsewhere in the body can spread to the bladder. This can happen with prostate, rectum, ovary, cervix and womb cancer for example.
Cancers that have spread from somewhere else in the body are called secondary cancers. The cancer cells are the same type as the first cancer. So is the treatment.
If you have cancer that has spread to the bladder, you need to go to the section about your primary cancer.
-
Cancer and Its Management J Tobias and D HochhauserWiley Blackwell, 2015
-
A M Kamat and othersThe Lancet, 2016. Volume 388, Pages 276 -2810
-
AJCC Cancer Staging Manuel American Joint Committee on CancerSpringer, 2017
-
Bladder cancer: diagnosis and management of bladder cancerNational Institute of Health and Clinical Excellence, 2015
-
Bladder Cancer
Papillary Vs Flat Cancer
Bladder cancers are also divided into 2 subtypes, papillary and flat, based on how they grow .
- Papillary carcinomas grow in slender, finger-like projections from the inner surface of the bladder toward the hollow center. Papillary tumors often grow toward the center of the bladder without growing into the deeper bladder layers. These tumors are called non-invasive papillary cancers. Very low-grade , non-invasive papillary cancer is sometimes called papillary urothelial neoplasm of low-malignant potential and tends to have a very good outcome.
- Flat carcinomas do not grow toward the hollow part of the bladder at all. If a flat tumor is only in the inner layer of bladder cells, it’s known as a non-invasive flat carcinoma or a flat carcinoma in situ .
If either a papillary or flat tumor grows into deeper layers of the bladder, it’s called an invasive urothelial carcinoma.
Recommended Reading: Frequent Bladder Infections In Females
About The Bladder Renal Pelvis And Ureter
The bladder is a hollow organ in the pelvis that stores urine before it leaves the body during urination. This function makes the bladder an important part of the urinary tract. The urinary tract is also made up of the kidneys, ureters, and urethra. The renal pelvis is a funnel-like part of the kidney that collects urine and sends it into the ureter. The ureter is a tube that runs from each kidney into the bladder. The urethra is the tube that carries urine out of the body. The prostate gland is also part of the urinary tract.
The bladder, like other parts of the urinary tract, is lined with a layer of cells called the urothelium. This layer of cells is separated from the bladder wall muscles, called the muscularis propria, by a thin, fibrous band called the lamina propria.
Cancerous Tumours Of The Bladder
A cancerous tumour of the bladder can grow into nearby tissue and destroy it. It can also spread to other parts of the body. Cancerous tumours are also called malignant tumours.
Bladder cancer is often divided into 3 groups based on how much it has grown into the bladder wall.
- Non-invasive bladder cancer is only in the inner lining of the bladder .
- Non–muscle-invasive bladder cancer has only grown into the connective tissue layer .
- Muscle-invasive bladder cancer has grown into the muscles deep within the bladder wall and sometimes into the fat that surrounds the bladder.
Read Also: Why Do I Keep Getting Bladder Infections After Intercourse
Small Cell Neuroendocrine Carcinoma
Last author update:Last staff update:Copyright:Page views in 2021:Page views in 2022 to date:Cite this page:
- High grade neuroendocrine neoplasm resembling small cell carcinoma of other organs
- Pure or admixed with high grade urothelial carcinoma of the kidney
- Rare, < 1% of renal neoplasms, ~ 50 cases reported
- Very rarely has been reported with renal cell carcinoma
- Median age 59 – 65 years, may be seen with high grade urothelial carcinoma of the kidney
- Likely arises from a multipotent stem cell
- Median survival 8 – 20 months
- Medullary location, lack of central necrosis in a large tumor
- 55 year old man with multicentric small cell neuroendocrine neoplasm of the renal pelvis and ureter
- 59 year old woman with primary small cell carcinoma of kidney after renal transplantation
- 71 year old woman with combined small cell and transitional cell carcinoma of the renal pelvis
- 76 year old woman with small cell carcinoma of the kidney
- Primary oat cell carcinoma of the kidney
- Surgery
- Chemotherapy +/- radiation
- Slightly improved survival of 17.3 months with neoadjuvant chemotherapy prior to nephrectomy
- Unifocal, centered in renal pelvis, usually invading perinephric adipose tissue
- Median size 11 cm, mean 7.1 cm in another study
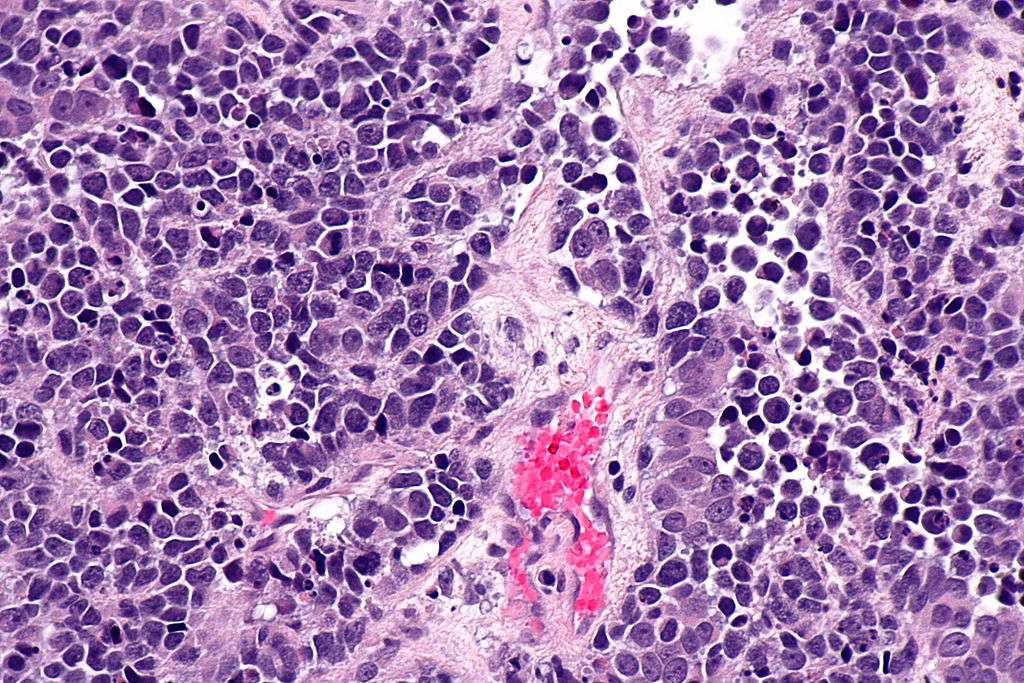
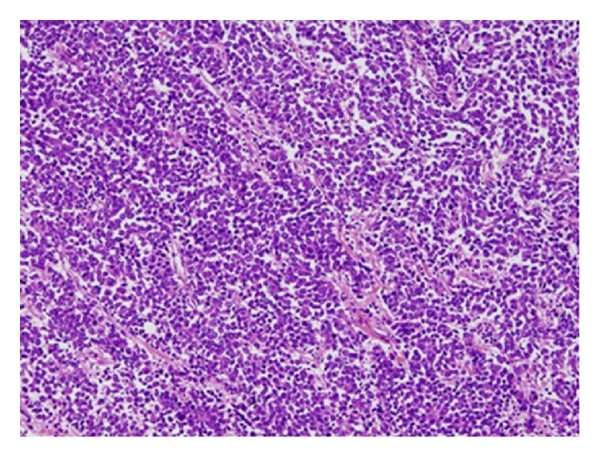
Urothelial small cell
In renal pelvis
- Similar morphology to small cell carcinoma of the lung
- Diffuse growth of small cells with minimal cytoplasm, nuclear molding, indistinct nucleoli, high mitotic activity and apoptosis, lymphovascular invasion, necrosis