Carcinomain Situ And Its Classification
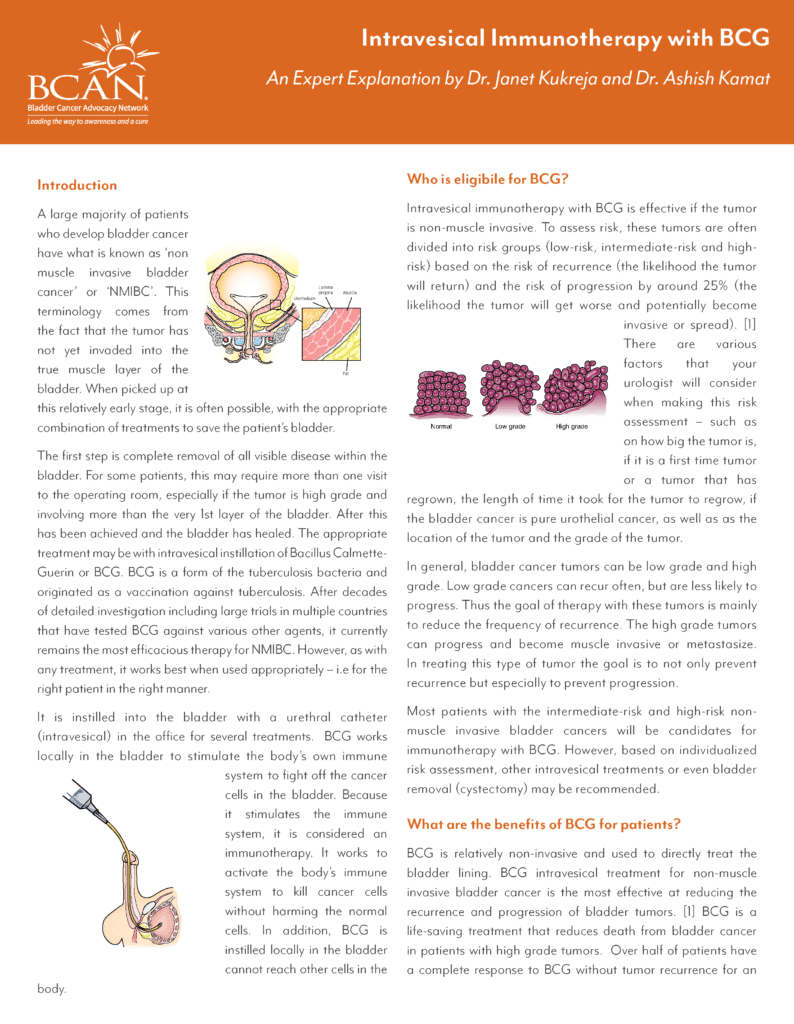
Carcinoma in situ is a flat,high-grade, non-invasive urothelial carcinoma. It can be missed or misinterpreted as aninflammatory lesion during cystoscopy if not biopsied. Carcinoma in situ is often multifocal and can occur in the bladder,but also in the upper urinary tract , prostatic ducts, and prostatic urethra .
From the clinical point of view, CIS may be classified as :
- Primary: isolated CIS with no previous or concurrent papillary tumours and no previousCIS
- Secondary: CIS detected during follow-up of patients with a previous tumour that was notCIS
- Concurrent: CIS in the presence of any other urothelial tumour in the bladder.
Who Can Have This Treatment
BCG is appropriate for noninvasive and minimally invasive bladder cancers. It usually follows a procedure called transurethral resection of bladder tumor . Its intended to help prevent recurrence.
This treatment only affects cells inside the bladder. Its not useful for later stage bladder cancer that has spread into or beyond the bladder lining, or to other tissues and organs.
Counselling Of Smoking Cessation
It has been confirmed that smoking increases the risk of tumour recurrenceand progression . Whileit is still controversial whether smoking cessation in BC will favourably influence theoutcome of BC treatment, patients should be counselled to stop smoking due to the generalrisks connected with tobacco smoking .
Recommended Reading: Does Overactive Bladder Come And Go
Bcg Strains: Is There A Difference
There have been several strains of BCG developed since the original strain in 1921, but whether these strains have varying efficacies on bladder tumours remain unclear. While hundreds of thousands of patients have been treated with BCG for prevention of NMIBC, no clinical difference has been shown among studies despite the use of various strains worldwide.
Trials using various strains have consistently demonstrated the efficacy of BCG immunotherapy in reducing recurrence and progression of NMBIC in all countries across the globe. BCG is recommended by all scientific associations from the European Association of Urology , American Urological Association, Japanese Association or the Canadian Urological Association.
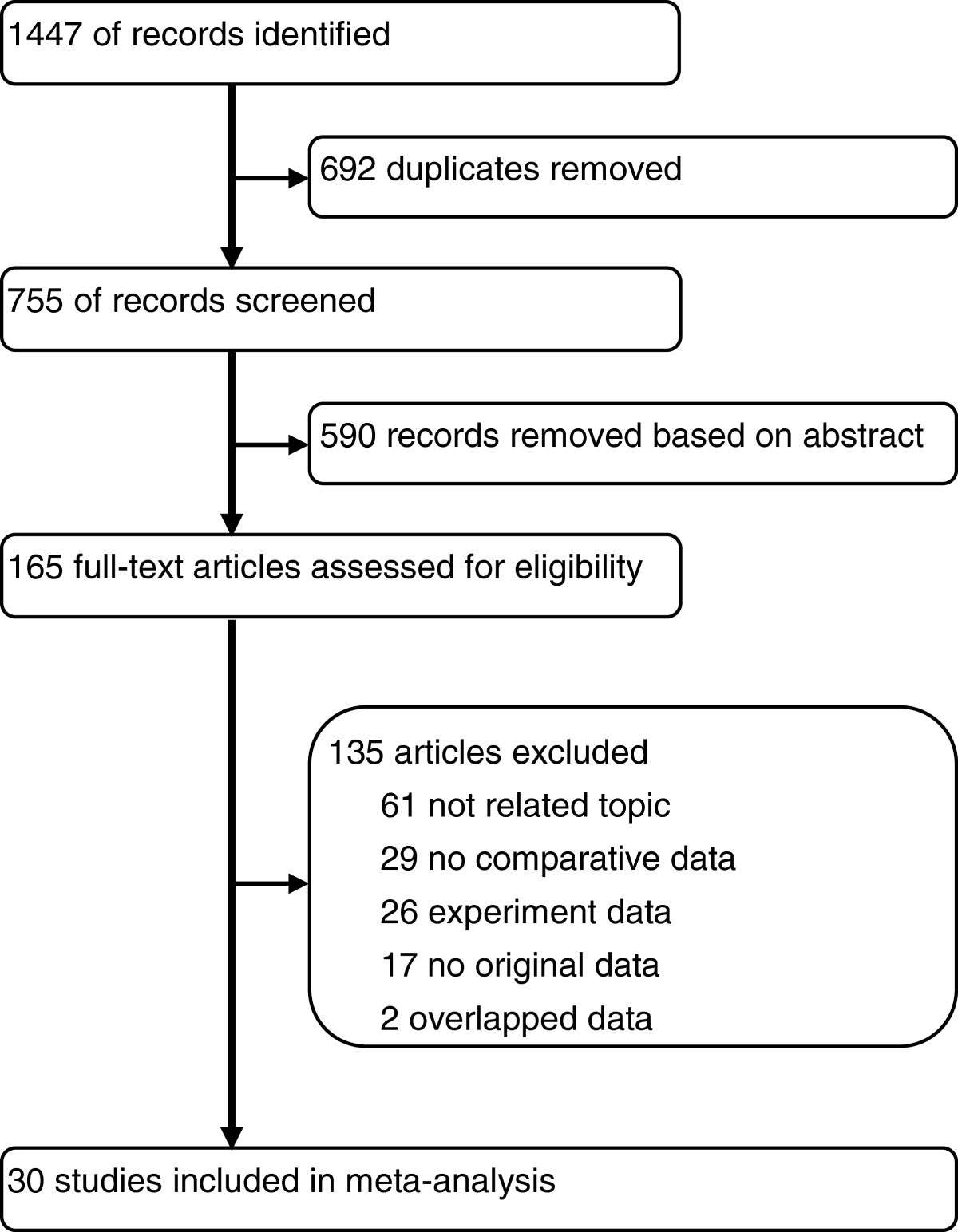
Sengiku and colleagues demonstrated no significant difference between the studied strains . Supporting a previous European Organization for Research and Treatment of Cancer meta-analysis which suggested that there is no large difference between different strains , a recent meta-analysis of randomised trials performed by Quan et al concluded that no meaningful correlations between BCG strain and other survival outcomes could be drawn. Another systematic review and meta-analysis by Chou et al concluded that no comment can be made regarding differences among strains. Gan et al studied the effects of substrain differences in BCG immunotherapy for bladder cancer and came to a similar conclusion.
Summary Of Evidence And Guidelines Forfollow
|
Summary of evidence |
|
|
The first cystoscopy after transurethral resection ofthe bladder at 3 months is an important prognostic indicator for recurrence andprogression. |
|
Patients with intermediate-risk Ta tumours shouldhave an in-between follow-up scheme using cystoscopy. |
Weak |
|
Regular upper tract imaging is recommended for high-riskand very high-risk tumours. |
Weak |
|
Endoscopy under anaesthesia and bladder biopsiesshould be performed when office cystoscopy shows suspicious findings or ifurinary cytology is positive. |
Strong |
|
During follow-up in patients with positive cytologyand no visible tumour in the bladder, mapping biopsies or PDD-guided biopsies and investigation of extravesical locations are recommended. |
Strong |
|
In patients initially diagnosed with TaLG/G1-2bladder cancer, use ultrasound of the bladder during surveillance in casecystoscopy is not possible or refused by the patient. |
Weak |
You May Like: Best Supplement For Overactive Bladder
What Conditions Are Treated With Bcg Treatment
BCG treatment is used to address early-stage bladder cancer. This includes bladder cancers that havent invaded your bladder wall muscle, such as carcinoma in situ bladder cancers and non-muscle invasive bladder cancers . BCG treatment isnt effective against bladder cancer that has metastasized .
Clinical trials are currently underway to explore BCG treatment for fibromyalgia and diabetes. Experts believe that BCG treatment may increase cytokines , which could potentially benefit people with these conditions. More research is needed in these areas, though.
Asco 202: Final Clinical Results Of Pivotal Trial Of Il
The 2022 ASCO annual meeting featured an oral abstract session on kidney and bladder cancer, including a presentation by Dr. Karim Chamie discussing the final results of the trial assessing IL-15RFc superagonist N-803 with BCG in BCG-unresponsive CIS and papillary NMIBC. Patients with NMIBC CIS unresponsive to BCG have limited treatment options. N-803 is a mutant IL-15-based immunostimulatory fusion protein complex that promotes proliferation and activation of natural killer cells and CD8+ T cells, but not regulatory T cells. Phase 1b data in BCG-naïve patients with NMIBC demonstrate that intravesical administration of N-803 with BCG induced complete response in all patients, without recurrences for the study duration of 24 months. Pembrolizumab was approved in 2020 with a 41% complete response rate in a single arm phase 2 trial of 96 patients.1 At ASCO 2022, Dr. Chamie and colleagues report data on 161 subjects from an open-label, 3 cohort multicenter study of intravesical BCG plus N-803 in patients with BCG-unresponsive high-grade NMIBC .
All treated patients received intravesical N-803 plus BCG, consistent with the standard induction/maintenance treatment schedule. The primary endpoint for Cohort A is incidence of complete response of CIS at any time. The primary endpoint for Cohort B is disease-free rate at 12 months. The trial design for QUILT 3.032 is as follows:
Read Also: Does Bladder Cancer Kill You
Risk Adjusted Surveillance And Follow
Guideline Statement 32
32. After completion of the initial evaluation and treatment of a patient with NMIBC, a clinician should perform the first surveillance cystoscopy within three to four months.
Discussion
The natural history of NMIBC is often characterized by recurrence, even for solitary, small, low-grade papillary tumors. At the time of first evaluation and treatment, none of the existent risk stratification tools or urinary biomarkers is sufficiently sensitive and specific to predict which patient will have an early tumor recurrence. Therefore, the only reliable way to know in a particular patient whether they are at risk for early recurrence is by cystoscopic visualization of the urothelium at a relatively early interval after the first treatment/resection. In addition, visualization at a relatively early interval allows the treating urologist to verify that the initial resection was complete. The Panel, therefore, felt that the first repeat cystoscopic evaluation should occur three to four months after the initial treatment and evaluation, regardless of the patient’s overall risk.
Guideline Statement 33
33. For a low-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent surveillance cystoscopy six to nine months later, and then annually thereafter surveillance after five years in the absence of recurrence should be based on shared-decision making between the patient and clinician.
Discussion
Discussion
Options After Bcg Failure
BCG treatment eventually fails in up to 50% of patients and in about half of those within the first 6 months. In tumours that do not respond to BCG anymore, conventional intravesical chemotherapy agents, such as doxorubicin, thiotepa and mitomycin, have limited activity. In addition, valrubicin, the only FDA-approved drug for BCG-refractory CIS, is only effective in < 10% of patients at 2 years and none with coincident stage T1 disease. Thus, the traditional approach after BCG treatment failure has been to advocate early cystectomy. However, several lines of evidence suggest a reasonably safe window of opportunity, probably up to 1.52 years after onset of the index high-grade tumour, in which other conservative, nonradical therapies might be tried without undue risk.,,,
Also Check: Weak Bladder Control After Childbirth
Scoringmodels Using The Who 1973 Classification System
6.1.1.1.The 2006 European Organisation forResearch and Treatment of Cancer scoring model
To be able to predict both the short- and long-term risks of diseaserecurrence and progression in individual patients, the EORTC Genito-Urinary Cancer Grouppublished a scoring system and risk tables based on the WHO 1973 classification in 2006 . The scoring system is based on the six most significantclinical and pathological factors in patients mainly treated by intravesical chemotherapy:
- Number of tumours
- Concurrent CIS
- WHO 1973 tumour grade.
Using the 2006 EORTC scoring model, individual probabilities of recurrenceand progression at one and five years may be calculated.
6.1.1.2.The model for patients with TaG1/G2 tumours treated with chemotherapy
Patients with TaG1/G2 tumours receiving chemotherapy were stratified intothree risk groups for recurrence, taking into account the history of recurrences, history ofintravesical treatment, tumour grade , number of tumours and adjuvant chemotherapy.
6.1.1.3.Club Urologico Español deTratamiento Oncologico scoring model for BCG-treated patients
- gender
- associated CIS
- WHO 1973 tumour grade.
6.1.1.4.The 2016 EORTC scoring model forpatients treated with maintenance BCG
Detection Of Residual Disease And Tumour Upstaging
The significant risk of residual tumour after initial TURB of TaT1 lesionshas been demonstrated .
A SR analysing data of 8,409 patients with Ta or T1 HG BCdemonstrated a 51% risk of justify persistence and an 8% risk of under-staging in T1tumours. The analysis also showed a high risk of residual disease in Ta tumours, but thisobservation was based only on a limited number of cases. Most of the residual lesions weredetected at the original tumour location .
Another meta-analysis of 3,556 patients with T1 tumoursshowed that the prevalence rate of residual tumours and upstaging to invasive disease afterTURB remained high in a subgroup with detrusor muscle in the resection specimen. In thesubgroup of 1,565 T1 tumours with detrusor muscle present, persistent tumour was found in58% and under-staging occurred in 11% of cases .
Recommended Reading: Can Bladder Infection Clear Up On Its Own
Bcg Failure And Subclassification
About 40% of patients of NMIBC will fail intravesical BCG treatment. Although many factors might lead to BCG failure, the dose of BCG and type of T helper response may lead to dramatically diverging outcomes. Low-dose BCG might not trigger enough TH1-type immune response, which is the main response to BCG activity. Too high doses of BCG may paradoxically activate mixed TH1/TH2 responses which will counterbalance the TH1 response . Other factors of BCG failure include occult micrometastatic disease prior to BCG therapy .
Patients who fail intravesical BCG treatment are usually sub-classified into three categories based on the type of failure:
BCG refractory, which is the persistence of disease after induction or maintenance BCG treatment.
BCG relapse, the recurrence of disease after a disease-free period post BCG treatment.
BCG intolerance when the patient is not tolerating the completion of BCG induction .
The definitions, endpoints and clinical trial designs for NMIBC as recommended by the International Bladder Cancer Group might serve as an excellent current state-of-the-art resource . The type of failure should be clearly defined. Because stakes are very high for these patients, for whom BCG has failed, and options are limited, single-arm designs may be relevant for the BCG-unresponsive population. The consensus for a clinically meaningful initial complete response rate or recurrence-free rate is of at least 50% at 6 months, 30% at 12 months and 25% at 18 months.
What Are The Side Effects
Some patients have difficulty completing long-term BCG therapy because of irritation in the bladder.2 To help with this irritation, the treatment frequency may be adjusted to give you a longer break between treatments. You may not notice any reaction after the first few BCG treatments. After the third treatment, patients usually start to experience bladder irritation pain or burning during urination, joint pain, fatigue, and flu-like symptoms that can last a few days. Most symptoms and side effects can be treated with over-the-counter pain medicines.
While BCG is a fairly common treatment for bladder cancer, every person has different experiences. It’s important to talk to your doctor about any questions or concerns you may have at any point during your treatment. Being mentally prepared for what to expect can help to reduce stress or uncertainty about treatment or help you think of additional questions for your healthcare team.
You May Like: Bladder Leakage In Your 20s
Maintaining A Regular Treatment Schedule
An example of a maintenance therapy treatment regimen is BCG immunotherapy delivered once per week for three weeks in a row. Some patients may be advised to receive this three-week round of treatment every three to six months for one year. Other patients may be advised to continue receiving maintenance therapy for longer than one year, with an example treatment regimen schedule of once per week for three weeks, and three to six months between treatments. For maintenance therapy to be as effective as possible, it is important to maintain the regular treatment schedule, as directed by your healthcare professional, without delays or skipping treatments.
Treating Stage 0 Bladder Cancer
Stage 0 bladder cancer includes non-invasive papillary carcinoma and flat non-invasive carcinoma . In either case, the cancer is only in the inner lining layer of the bladder. It has not invaded the bladder wall.
This early stage of bladder cancer is most often treated with transurethral resection with fulguration followed by intravesical therapy within 24 hours.
Read Also: Icd 10 Incontinence Of Bowel And Bladder
Box : Recommendations For Intravesical Bcg
RCTs and practice pattern research demonstrate that BCG immunotherapy in NMIBC reduces recurrences and progression, and affects mortality
3-week BCG maintenance is confirmed to reduce recurrence rates compared with induction alone, as well as metastasis and mortality compared with maintenance chemotherapy thus, it is the optimal regimen for current practice
BCG maintenance schedules other than the 3-week schedule show no significant benefit in RCTs
In the period of around 1.52 years after the identification of high-grade NMIBC, nonradical alternative treatments for patients experiencing BCG-failure can be explored
After the first BCG failure, patients have several treatment options, including repeated BCG , BCG plus interferon, single-agent intravesical chemotherapy , sequential chemotherapy or device-assisted chemotherapy
After the second BCG failure, or if the disease is BCG-refractory, radical cystectomy should be considered with alternatives considered a matter of investigation by clinical trials
Patients with BCG-refractory disease who are not candidates for cystectomy can be considered for chemoradiation
Abbreviations: NMIBC, non-muscle-invasive bladder cancer RCTs, randomized controlled trials.
Relevance Of The International Bcg Shortage To The Aua Guidelines
The global shortages in TICE BCG that occurred in 2014 and 2019 led the AUA to recommend several management strategies to maintain high quality care for patients with NMIBC. These recommendations may supersede the guideline statements below. In particular, the BCG shortage impacts guideline statements 17, 20, and 21. The AUA Statement on the BCG Shortage is available at .
Recommended Reading: Bladder Cancer Metastasis To Lung Symptoms
When Is Bcg Treatment Used
You may have BCG directly into your bladder after surgery to remove non-muscle-invasive bladder cancer. This type of surgery is called a transurethral resection of a bladder tumour .
This treatment helps prevent the cancer from coming back in the bladder lining. It also reduces the risk of the cancer becoming muscle-invasive. Doctors usually suggest this treatment if you have a high-risk bladder cancer, or sometimes if you have an intermediate-risk bladder cancer.
There is usually at least 2 weeks between the surgery to remove the cancer and the start of BCG treatment. This is to give your bladder enough time to heal from the surgery.
You usually have BCG treatment once a week for 6 weeks. This is sometimes called the induction course. You may be offered more BCG treatments. This is usually called maintenance treatment.
Treatment times vary. Your doctor will explain what is best for you.
Predictors Of Response To Bcg
Markers of response to intravesical BCG fall into three broad categories: determination of response , use of surrogate endpoint biomarkers and prediction of response. BCG is most frequently used to treat high-grade disease and assessing the response of CIS specifically is challenging because it is often difficult to detect. A commonly used design is to determine response by cystoscopy, cytology and possibly bladder biopsy at 3 months and 6 months following a BCG induction regimen. However, the 3-month assessment is problematic because of the well documented conversion of positive cytology at 3 months to negative cytology at 6 months, particularly after maintenance BCG. Fluorescence cystoscopy can improve detection of both CIS and papillary bladder cancer, but fluorescence can also be induced by inflammation. It remains to be seen whether fluorescence cystoscopy can reliably improve the determination of BCG response.
Cytology is a subjective test with variable performance molecular tests that are more objective might yield better and more consistent performance in detecting visually occult bladder cancer. Patients who have abnormal results in the UroVysion assay in a urine sample obtained immediately before the last of the 6-week induction instillations have increased risk for tumour recurrence and progression.
Read Also: How Do I Treat A Bladder Infection At Home
Advantages Of T Cells In Immunotherapy
T cells are defined by expression of and heterodimer of T cell receptor chains that directs intracellular signaling without the recognization of MHC molecule. Unlike Ag-specific T cells, T cells can kill tumor cells in a manner that does not require the recognition of tumor-specific Ags. They have shown significant advantages in cancer immunotherapy, including but not limited to the followings:
How Long Does It Last
The aim of maintenance therapy is to try to reduce the risk of bladder cancer recurrence as much as possible.2,3 The length of a patients maintenance therapy with BCG immunotherapy depends on multiple factors, such as the grade of the patients cancer, and the judgment of the healthcare providers on the cancer care team.
Don’t Miss: What Do Bladder Spasms Feel Like