What Does A Prolapsed Bladder Feel Like
Can a womans uterus fall out?
Does it hurt when your uterus falls out?
What are the signs of a falling bladder?
Can your uterus or bladder fall out of your body?
While your uterus and other organs will not fall out of your body , the weakening of your pelvic floor muscles can make it feel and appear as though this may happen. The most common and bothersome symptom is pressing of the uterus or other organs against the vaginal wall.
How do you know if my bladder has fallen?
Urinary symptoms may vary from urinary incontinence, specifically stress incontinence, to difficulty urinating and incomplete emptying of the bladder. Other symptoms like episodes of burning during urination, cloudy urine and blood in the urine may be due to repeated bladder infections which is a risk with a fallen bladder.
What is the procedure for a fallen bladder?
Prolapsed bladder surgery is a procedure to repair a womans bladder that has fallen from its normal place, also called a cystocele or a fallen bladder. While surgery is not usually the first course of treatment, it may be needed for women who have persistent symptoms.
Who Is More Likely To Have A Cystocele
A cystocele can affect women of any age, but your chances of developing a cystocele increase with age because muscles and tissues often become weaker over time. Other factors that increase your risk of having a cystocele include
- giving birth vaginally
- having a family history of pelvic organ prolapse
Surgery For A Pelvic Organ Prolapse
If you have severe bladder prolapse, surgery may be required. During surgery, a mesh support is inserted into the vaginal wall and the bladderâs position is corrected. This can be performed under general, regional or local anesthesia. Talk with your doctor for more information on surgery options and if it is required to fix your prolapsed bladder.
You May Like: Ways To Control Your Bladder
How Common Is A Cystocele
A cystocele is common. Experts estimate that nearly half of women who have given birth have some degree of pelvic organ prolapse.1 However, many other women with the condition do not have symptoms or do not seek care from a health care professional. As a result, the condition is underdiagnosed, and it is not known exactly how many women are affected by cystoceles.
Symptoms Of Prolapsed Bladder
The presence of tissue in the vaginal area, which many women describe as feeling like a ball, is frequently the initial symptom of a prolapsed bladder.
Other signs and symptoms of a prolapsed bladder include:
- Pelvic dissatisfaction or discomfort
- Feeling as if your bladder isnt empty after youve urinated
- Incontinence due to stress
- Frequent bladder infections
- Intercourse that is painful
- Pelvic or lower back pain, fullness, heaviness, or discomfort. When the person stands, lifts, coughs, or as the day develops, the sensation may worsen
- Tampons or applicators are difficult to implant
- The bladder pushes its way into or out of the vaginal opening
- Heaviness or pressure in the vaginal area
You May Like: Signs Bladder Cancer Has Spread
How Do Health Care Professionals Diagnose A Cystocele
To diagnose a cystocele, health care professionals ask about your symptoms and medical history and perform a physical exam, including a pelvic exam to check your lower abdomen. You may be asked to stand during part of the exam, which may feel awkward but allows your health care professional to determine the severity of your cystocele. Your health care professional may also order medical tests to determine how advanced the cystocele is or to help find or rule out other problems in your urinary tract or pelvis.
After Treatment Of Prolapse Bladder
Nonsurgical therapy may be all that is required to successfully treat a prolapsed bladder in mild situations.
Some women will require a second procedure if the first failed, the cystocele resurfaced, or another pelvic floor issue developed. Women who are older, smokers, diabetics, or have had a hysterectomy are more prone to have problems.
Don’t Miss: Bladder And Prostate Cancer At The Same Time
Vaginal Extrusion And Erosion
Additionally, Gomes and colleagues found urethral erosion happened after less than 1 percent of sling surgeries.
A pelvic exam revealed mesh extrusion.
In some cases, conservative management of erosion may be possible. For example, some surgeons may prescribe topical estrogen cream to help vaginal tissues heal.
Do I Need Pelvic Organ Prolapse Surgery
Depending on the severity of your pelvic organ prolapse symptoms, minimally invasive GYN surgery may be the best treatment, said Dr. Paul MacKoul, MD, The Center for Innovative GYN Care. Some patients find that their symptoms are manageable and prefer not to treat them. Others decide that surgical management is the best option for them as conservative treatments are not effective for long-term relief. However, surgery is typically delayed until women are finished with childbearing.
Women with symptoms for whom conservative management options are unsuccessful can seek a minimally invasive pelvic organ prolapse surgery. Surgical outcome can depend upon the severity of symptoms, extent of prolapse, and the patients expectations.
Also Check: Botox Injection For Bladder Incontinence
What Is A Cystocele
A cystocele is a condition in which supportive tissues around the bladder and vaginal wall weaken and stretch, allowing the bladder and vaginal wall to fall into the vaginal canal.
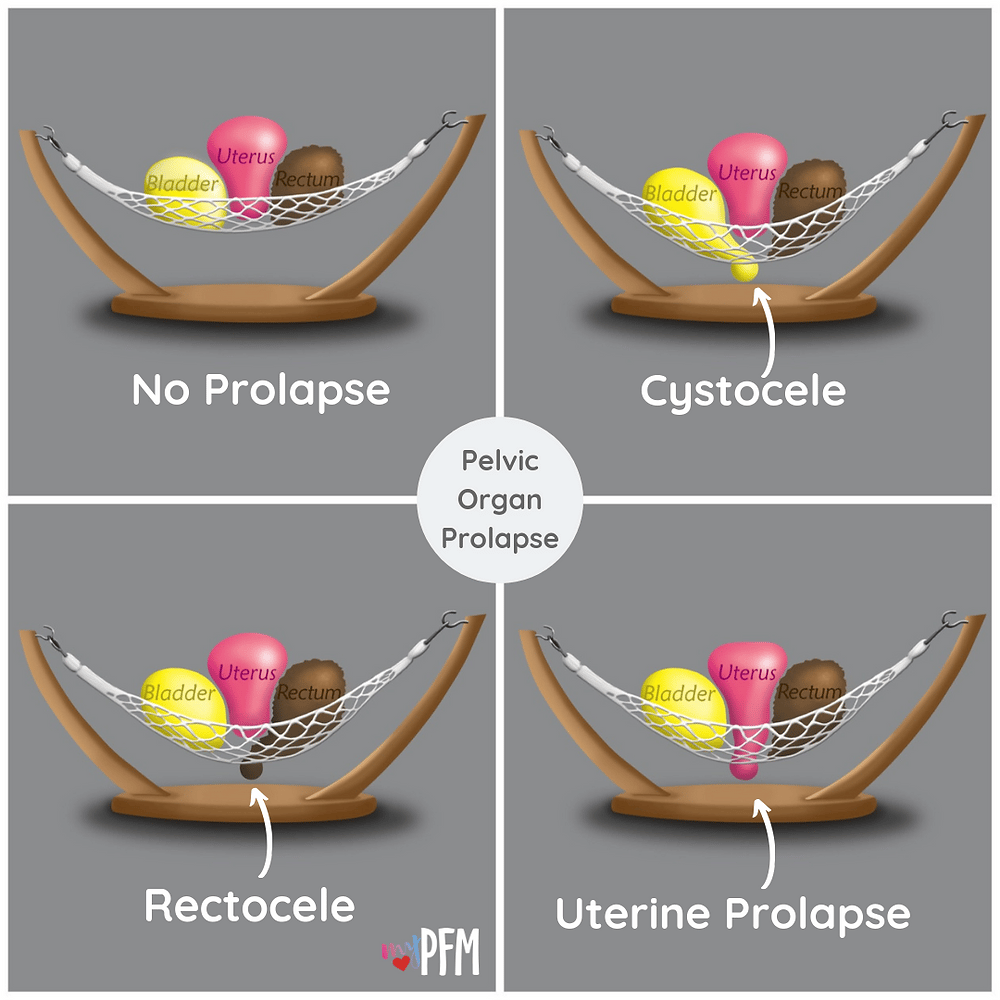
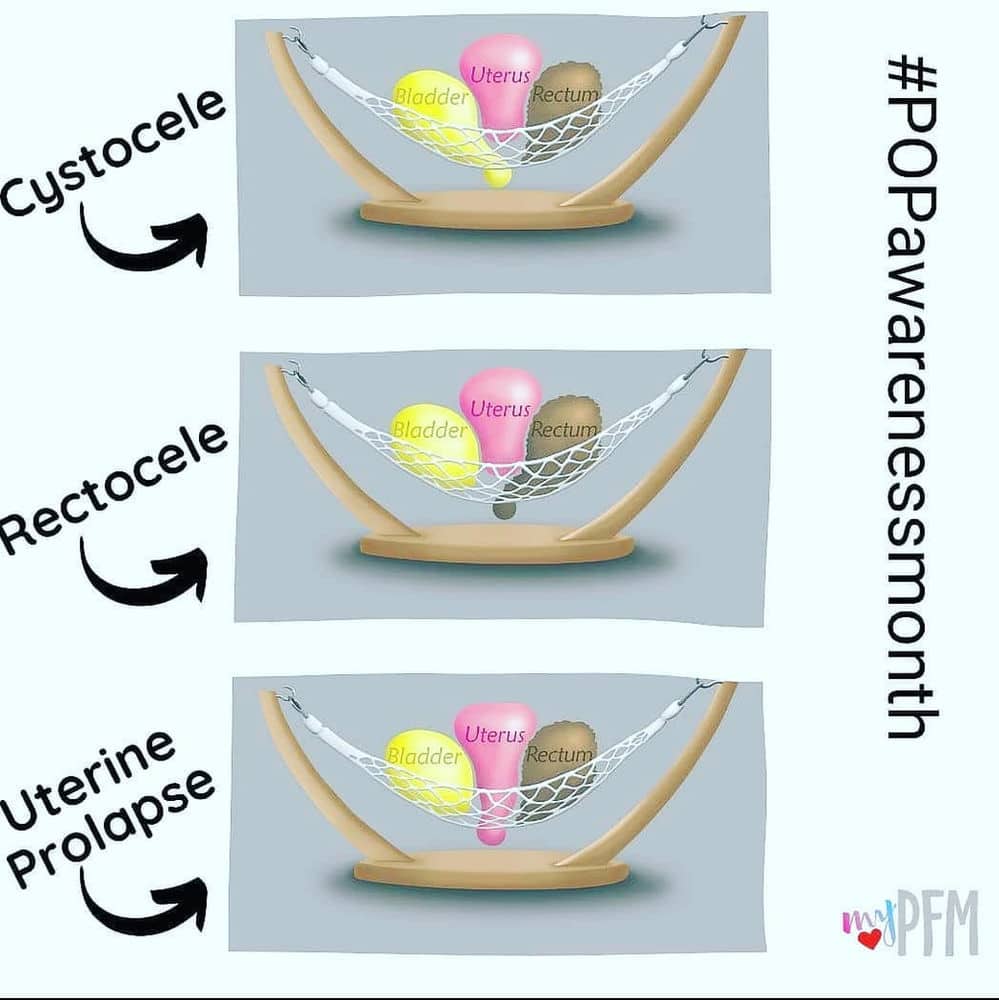
A cystocele is the most common type of pelvic organ prolapse. Pelvic organ prolapse occurs when the vaginal walls, uterus, or both lose their normal support and prolapse, or bulge, into the vaginal canal or through the vaginal opening. Other nearby pelvic organs, such as the bladder or bowel, may be involved and also drop from their normal position in the body.
A cystocele occurs when supportive tissues around the vaginal wall and bladder weaken and stretch, allowing the bladder and vaginal wall to bulge into the vaginal canal.
Treatment For Prolapsed Bladder
Treatment is determined by whether or not you have symptoms, the severity of your anterior prolapse, and whether or not you have any other diseases, such as urinary incontinence or several types of pelvic organ prolapse.
Mild instances, with few or no visible symptoms, usually do not require treatment. Your doctor may advise you to wait and see, with periodic appointments to monitor the prolapse.
Read Also: What Antibiotic Is Good For Bladder Infection
Treating Pelvic Organ Prolapse
There are several treatment options available for a pelvic organ prolapse, depending on your circumstances.
The treatment most suitable for you depends on:
- the severity of your symptoms
- the severity of the prolapse
- your age and health
- whether you’re planning to have children in the future
You may not need any treatment if your prolapse is mild to moderate and not causing any pain or discomfort.
The various treatments for pelvic organ prolapse are outlined below.
Diagnosis Of Bladder Prolapse
Bladder prolapse is diagnosed by:
- medical history including checking for possible risk factors
- physical vaginal examination to allow assessment of the degree of prolapse, pelvic floor muscle function, presence of any other prolapse and other abnormalities in the pelvis, such as tumours or masses.
Read Also: How Do You Know If Your Bladder Is Leaking
Don’t Miss: Colon Cancer And Bladder Problems
Treatment For Symptomatic Bladder Prolapse
If you have symptoms of bladder prolapse it is recommended that, as for people with no symptoms, you make the same lifestyle changes, do pelvic floor muscle training and treat any chronic cough. Make them part of your routine.
However, sometimes prolapse can be more severe and these measures may not be enough on their own to relieve symptoms.
For these cases, there can be two different approaches:
1. Non-surgical approach vaginal pessaries
Some women may prefer this option if they wish to avoid or delay surgery, and it may be the safest option for women who are unfit for surgery.You will need regular check-ups with your healthcare professional if you are using a vaginal pessary long-term.
2.Surgical approach
In some cases, when all other management options have failed to help with the symptoms, or when a woman does not want to use a pessary, surgery may be necessary. The type of surgery used will depend on your combination of prolapse and urinary tract symptoms. Your doctor will discuss the available surgical techniques with you.It is common to have a urinary catheter inserted during the operation to rest your bladder for a day after surgery, but this will depend on the procedure you have. Recovery from surgery takes about six weeks. You doctor will advise you about how to look after yourself during the recovery period, and a physiotherapist can recommend appropriate exercises.
Suggestions may include:
- resting each day.
Risk Factors For Bladder Prolapse
Risk factors for bladder prolapse include anything that puts pressure on the pelvic floor and affects its function, such as:
- pregnancy and childbirth
- regularly straining on the toilet to pass bowel motions or empty the bladder
- being overweight
- chronic cough secondary to smokers cough or chronic lung diseases
- repetitive lifting of children or heavy weights at work or in the gym, or any exercises where there is excessive downward pressure on the pelvic floor
- pelvic or gynaecological surgery
- strong family history
- connective tissue disease, in which the tissues in the body are not able to hold the weight of the organs
Don’t Miss: Muscle Invasive Bladder Cancer Icd 10
What To Expect From Your Doctor
During your appointment, your provider may ask a number of questions, such as:
- When did you first notice your symptoms?
- Do you have urine leakage?
- Do you have frequent bladder infections?
- Do you have pain or leak urine during intercourse?
- Do you have a chronic or severe cough?
- Do you experience constipation and straining during bowel movements?
- What, if anything, seems to improve your symptoms?
- What, if anything, seems to worsen your symptoms?
- Does your mother or a sister have any pelvic floor problems?
- Have you delivered a baby vaginally? How many times?
- Do you wish to have children in the future?
- What else concerns you?
How Is A Cystocele Diagnosed
The doctor may also perform certain tests, including the following:
- Urodynamics: Measures the bladders ability to hold and release urine.
- Cystoscopy : A long tube-like instrument is passed through the urethra to examine the bladder and urinary tract for malformations, blockages, tumors, or stones.
Recommended Reading: Tampon For Bladder Leakage Commercial
Tests For Bladder Prolapse
Tests that may be carried out to confirm or reject a diagnosis of bladder prolapse, depending on your symptoms, are:
- pelvic ultrasound to exclude any masses or cysts putting pressure on the bladder
- urodynamics a test of bladder function and to assess different types of incontinence
- a bladder scan to measure residual urine urine left in the bladder after emptying
- a midstream urine test to exclude urinary tract infection
- magnetic resonance imaging in some cases.
What Are The Complications Of A Cystocele
A cystocele may put pressure on or lead to a kink in the urethra and cause urinary retention, a condition in which you are unable to empty all the urine from your bladder. In rare cases, a cystocele may result in a kink in the ureters and cause urine to build up in the kidney, which can lead to kidney damage.
Recommended Reading: How To Help A Weak Bladder Naturally
How Can I Prevent Pelvic Organ Prolapse
Researchers are studying ways to prevent pelvic organ prolapse. The following steps may reduce your risk of getting a pelvic floor problem:
- Maintain a healthy weight or lose weight . Women who have overweight or obesity are more likely to have pelvic floor problems.
- Choose foods with fiber. Fiber helps prevent constipation and straining during bowel movements. Preventing constipation may reduce the risk of some pelvic floor disorders.
- Do not smoke. Smoking can lead to chronic cough, which puts stress on the pelvic floor muscles.
If You Have Signs Of Anterior Prolapse Your First Line Of Defense Is To:
- Exercises to strengthen the muscles of the pelvic floor
These exercises, also known as Kegels, strengthen your pelvic floor muscles, allowing them to better support your bladder and other pelvic organs. You can get instructions on how to execute these exercises from your doctor or physical therapist, and they can also help you assess if youre doing them correctly.
When taught by a physical therapist and reinforced with biofeedback, Kegel exercises may be most effective at alleviating symptoms. Biofeedback entails the use of monitoring devices to guarantee that youre tightening the right muscles for the right amount of time and with the right intensity. These exercises may make you feel better, but they are unlikely to reduce the size of the prolapse.
- A device that assists
Also Check: Can Dehydration Cause Overactive Bladder
What Are The Symptoms Of Pelvic Organ Prolapse
Other symptoms of pelvic organ prolapse include:
- A feeling of pressure, discomfort, aching, or fullness in the pelvis
- Pelvic pressure that gets worse with standing or coughing or as the day goes on
- Leaking urine or problems having a bowel movement
- Problems inserting tampons
Some women say that their symptoms are worse at certain times of the day, during physical activity, or after standing for a long time. Talk to your doctor or nurse about your symptoms.
Diagnosis Of Prolapsed Bladder
The following tests may be used to diagnose anterior prolapse:
- Pelvic examination Its possible that youll be examined while lying down or standing up. During the examination, your doctor will search for a tissue protrusion in your vaginal wall, which indicates pelvic organ prolapse. Youll probably be asked to bear down as if youre having a bowel movement to see how much this influences the degree of prolapse. Youll be asked to contract your pelvic floor muscles as if youre trying to stop the flow of urine to test their strength.
- Urine and bladder testing You may be checked to assess how well and thoroughly your bladder empties if you have substantial prolapse. If you seem to be retaining more pee in your bladder than is typical after urinating, your doctor may run a test on a urine sample to search for signs of a bladder infection.
- Questionnaire You may be asked to complete a form that will assist your doctor in determining your medical history, the severity of the prolapse, and how much it impacts your quality of life. This data also aids in making treatment decisions.
Don’t Miss: What Does Bladder Pain Feel Like
Prolapsed Bladder Symptoms In Men:
- Male urinary dysfunction: This condition can involve leaking urine after peeing, frequent urination and other bladder and bowel issues.
- Erectile Dysfunction : ED is when men cant get or maintain an erection during sex. Sometimes pelvic muscle tension or pain can contribute to this issue.
- Prostatitis: Pelvic floor dysfunction and prolapse symptoms closely resemble prostatitis, which is an infection or inflammation of the prostate. Prostatitis can have many causes including bacteria, sexually transmitted infections or trauma to the nervous system.
- A sense that something is falling out
- Trouble emptying your bowel or bladder completely
- Urine leakage, frequency, chronic urinary tract infections, difficulty urinating
- Difficult bowel movements or trapping of stool
What Causes Pelvic Organ Prolapse
Pelvic organ prolapse happens when the muscles or connective tissues of the pelvis do not work as they should. The most common risk factors are:
- Vaginal childbirth, which can stretch and strain the pelvic floor. Multiple vaginal childbirths raise your risk for pelvic organ prolapse later in life.4 But you can get prolapse even if you have never had children or if you had a cesarean, or C-section, delivery.
- Long-term pressure on your abdomen, including pressure from obesity, chronic coughing, or straining often during bowel movements
- Giving birth to a baby weighing more than 8½ pounds5
- Aging. Pelvic floor disorders are more common in older women. About 37% of women with pelvic floor disorders are 60 to 79 years of age, and about half are 80 or older.1
- Hormonal changes during menopause. Loss of the female hormone estrogen during and after menopause can raise your risk for pelvic organ prolapse. Researchers are not sure exactly why this happens.6
- Family history. Researchers are studying how genetics can play a role in pelvic organ prolapse.
Recommended Reading: Does Bcg Cure Bladder Cancer
Bladder Prolapse At A Glance
- Bladder prolapse occurs when the hammock of pelvic floor muscles that support the bladder weakens and the bladder drops out of its proper position.
- Bladder prolapse, also called cystocele, commonly occurs in women due to age, injury or childbirth.
- Treatment ranges from lifestyle changes to medications and surgery.
My Bladder Has Fallen And I Cant Get Up Why Didnt Anyone Tell Me About Cystocele
When I was pregnant with my first child, I read everything I could. But, one thing no one told me was that one possible side effect of childbirth could be that my bladder may someday fall out of its normal resting spot inside my body.
Now before I send any of my pregnant readers into a tizzy, please note that this condition, known as cystocele, is fairly uncommon, especially among younger women. But, if you have ever needed a reason to kegel, keep reading.
OK. . .all clear?
Heres the scoop:
It was another ordinary night in the Fairly Odd household in spring 04. Fairly Odd Father was enjoying a night out with the boys to see the Boston Bruins. I was four months pregnant with my third child. Belly was three and Jilly had just turned a year old.
I decided to give the girls a bath, so I got the water in the tub ready. But, as I lifted them into the tub, I felt an odd sensation. It was if something was sliding out of me. Not painful, just not right. I had visions of me birthing my baby right then and there, on the bathroom floor. I thought about an ex-coworker who told the story of how her mother knew she was about to birth her twins when she looked down and saw a leg coming out. I hope I dont see a leg was all my brain could muster.
I then reached down and pushed something back up into my body. Something squishy and fleshy and not a baby leg. I suppose I should be so very thankful of that fact.
I answered his questions:
Read Also: What To Take For Bladder Control