Diagnosis Of Bladder Prolapse
Bladder prolapse is diagnosed by:
- medical history including checking for possible risk factors
- physical vaginal examination to allow assessment of the degree of prolapse, pelvic floor muscle function, presence of any other prolapse and other abnormalities in the pelvis, such as tumours or masses.
What Medications Treat A Prolapsed Bladder
- In mild cases of prolapsed bladder, estrogen may be prescribed in an attempt to reverse bladder prolapse symptoms, such as vaginal weakening and incontinence. For more severe degrees of prolapse, estrogen replacement therapy may be used along with other types of treatment.
- Estrogen can be administered orally as a pill or topically as a patch or cream. The cream has very little systemic absorption and has a potent effect locally where it is applied.
- Topical administration has less risk than the oral preparations.
Physical Blockage In The Lower Urinary Tract
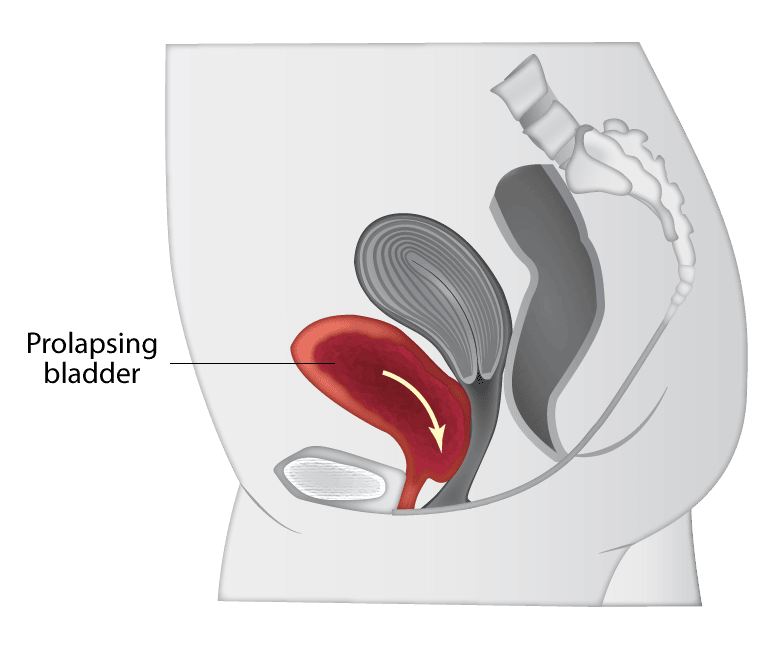
For women, any blockage in the lower urinary tractthe bladder and urethracan also lead to urinary retention.
The blockage can be inside the bladder, such as in the case of bladder stones or tumors.
The neck of the bladder can be obstructed in what is known as bladder outlet obstruction . This condition in women is rare and poorly understood.
The urethra can also be obstructed in what is known as urethral stricture. Scar tissue formed by previous urethral trauma can obstruct the urethra. Infections can also cause swelling which narrows the urethra.
Recommended Reading: Treatment For Early Stage Bladder Cancer
Who Gets Pelvic Organ Prolapse
Pelvic floor disorders affect one in five women in the United States.1 Pelvic organ prolapse is less common than urinary or fecal incontinence but affects almost 3% of U.S. women.1 Pelvic organ prolapse happens more often in older women and in white and Hispanic women than in younger women or women of other racial and ethnic groups.2,3
Some women develop more than one pelvic floor disorder, such as pelvic organ prolapse with urinary incontinence.
What You Need To Know
- When pelvic muscle, tissue and ligaments weaken, the uterus can drop down into the vaginal canal, causing uterine prolapse.
- Nearly one-half of all women between ages 50 and 79 have some degree of uterine or vaginal vault prolapse, or some other form of pelvic organ prolapse.
- Factors that increase your risk of uterine prolapse include childbirth, age, obesity, chronic constipation and having a hysterectomy.
- There is no definitive way to prevent uterine prolapse. Losing weight, eating a fiber-rich diet, quitting smoking and performing pelvic floor exercises can help to reduce the risk of this condition.
Also Check: My Bladder Is Full But I Cant Pee
Can Uterine Prolapse Be Prevented
There is no certain way to prevent uterine prolapse. However, the following can help lower your risk:
-
Lose weight, if youre overweight
-
Follow a diet rich in fiber and fluids to prevent constipation and straining
-
Avoid heavy lifting
-
Quit smoking, if you smoke
-
Seek prompt treatment for a chronic cough, which can place extra pressure on your pelvic organs
-
Do Kegel exercises to strengthen your pelvic floor muscles
These actions may also help if you already have uterine prolapse.
See your healthcare provider when symptoms first start to bother you. Dont wait until your discomfort becomes severe. Regular pelvic exams can help detect uterine prolapse in its early stages.
What Type Of Doctor Should I See For Pelvic Prolapse
Your doctor may recommend a specialist with certification in Female Pelvic Medicine and Reproductive Surgery , such as a gynecologist, a urologist or a urogynecologist, also known as a urogyn. A urogynecologist is a medical doctor who has completed a residency in obstetrics and gynecology or urology.
You May Like: Bladder Pressure And Frequent Urination
Symptoms Of Pelvic Organ Prolapse
Pelvic organ prolapse symptoms include:
- a feeling of heaviness around your lower tummy and genitals
- discomfort or numbness during sex
- problems peeing such as feeling like your bladder is not emptying fully, needing to go to the toilet more often, or leaking a small amount of pee when you cough, sneeze or exercise
Sometimes pelvic organ prolapse has no symptoms and is found during an internal examination carried out for another reason, such as cervical screening.
At What Stage Of Prolapse Require Surgery
Consider surgery if the prolapse is causing pain, if you are having problems with your bladder and bowels, or if the prolapse is making it hard for you to do activities you enjoy. An organ can prolapse again after surgery. Surgery in one part of your pelvis can make a prolapse in another part worse.
Also Check: Tens Unit For Overactive Bladder
What Are The Symptoms Of Prolapse
- A sensation of sitting on something that is not supposed to be there.
- A protrusion through the vaginal opening.
- Difficulty emptying the bladder or bowels.
- Pain in the lower back or abdomen.
- An increase in vaginal discharge.
- Sexual dysfunction, including painful or difficult intercourse.
- Development of other pelvic floor disorders, including urinary or bowel incontinence, overactive bladder and recurrent bladder infection.
Prolapse can be worse at some times than others. For instance, symptoms are usually more pronounced after strenuous activity or straining for constipation. Gravity and pressure also tend to make prolapse worse at the end of the day. Laying down or resting usually make symptoms less noticeable.
What Is The Best Treatment For A Prolapsed Bladder
If you do have symptoms of anterior prolapse, first line treatment options include:
- Pelvic floor muscle exercises. These exercises often called Kegel exercises or Kegels help strengthen your pelvic floor muscles, so they can better support your bladder and other pelvic organs. …
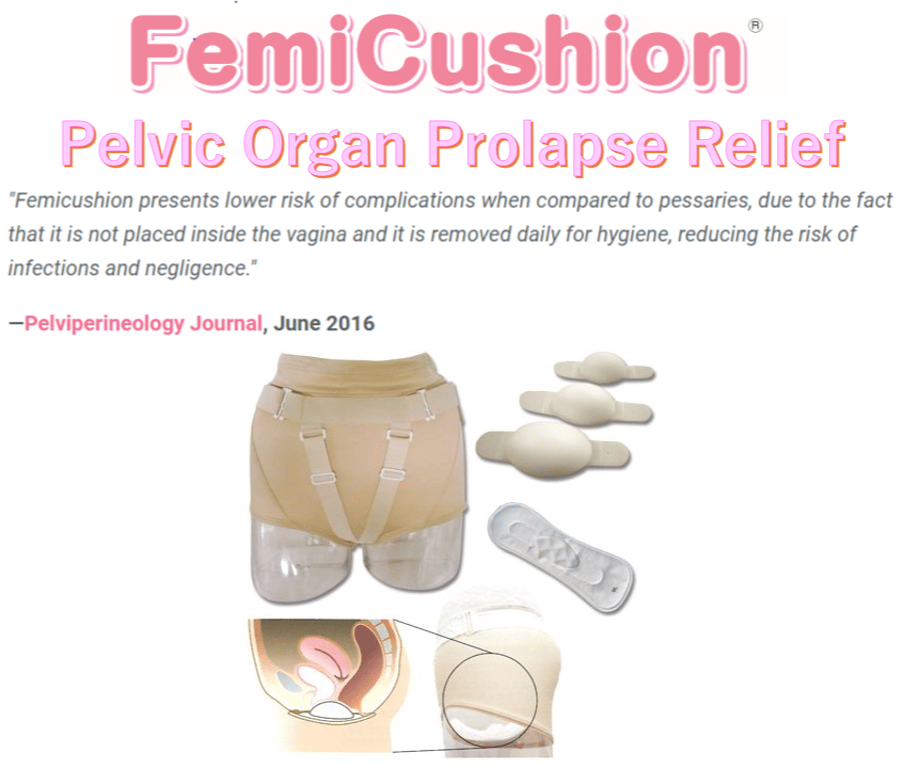
- A supportive device .
Don’t Miss: Can Lower Back Pain Cause Bladder Problems
Whos At Risk For Developing Pop
The risk of POP increases as women get older and after childbirth. Women who have had multiple vaginal deliveries or vaginal deliveries that required the use of instruments such as forceps or a vacuum have a higher risk for developing POP. Other risk factors include:
- Family history: Your mother or other women in your family have a history of POP.
- Injury: You had a pelvic floor injury caused by a fall or other accident or had a pelvic surgery, such as a hysterectomy.
- Smoking: Youre a smoker, as this can contribute to chronic coughing and lead to weakened connective tissues in the pelvic floor.
- Lifting and overuse: You have stressed your pelvic floor with repeated, strenuous activities or heavy lifting.
- Chronic constipation/straining: Youve experienced chronic constipation and straining with bowel movements.
- Weight: Youre overweight or obese.
Symptoms Of Bladder Prolapse
The symptoms of bladder prolapse depend on the severity of the prolapse, your level of physical activity and the presence of any other type of prolapse.They include:
- urinary stress incontinence leaking urine when coughing, sneezing, laughing, running or walking, or urge incontinence, which is urgently needing to go and leaking on the way
- needing to empty your bladder more frequently
- inability to completely empty your bladder when going to the toilet
- recurrent urinary tract infections
- protrusion of the vaginal wall out through the vaginal entrance
- needing to go back to the toilet immediately after finishing passing urine.
Don’t Miss: How To Know If Cat Has Bladder Infection
What Customers Are Saying:
I feel so much better today, and upon further investigation believe that there is a chance that the responses I got saved me from a serious, even life threatening situation. I am very grateful to the experts who answered me.
Susan O.USA
I can go as far as to say it could have resulted in saving my sons life and our entire family now knows what bipolar is and how to assist and understand my most wonderful son, brother and friend to all who loves him dearly.Thank you very much
Corrie MollPretoria, South Africa
I thank-you so much! It really helped to have this information andconfirmation. We will watch her carefully and get her in for theexamination and US right away if things do not improve. God bless you aswell!
ClaudiaAlbuquerque, NM
Outstanding response time less than 6 minutes. Answered the question professionally and with a great deal of compassion.
KevinBeaverton, OR
Suggested diagnosis was what I hoped and will take this info to my doctor’s appointment next week.I feel better already! Thank you.
ElanorTracy, CA
Thank you to the Physician who answered my question today. The answer was far more informative than what I got from the Physicians I saw in person for my problem.
JulieLockesburg, AR
You have been more help than you know. I seriously don’t know what my sisters situation would be today if you had not gone above and beyond just answering my questions.
John and StefanieTucson, AZ
Frequently Asked Questions About Pelvic Floor Disorders
Every year, 300,000 American women have an injury during vaginal childbirth that leads to incontinence and other pelvic floor disorders, including prolapse. But what do you really know about these disorders? Here are some of the most common questions that our Michigan Medicine urogynecologists answer about pelvic floor disorders:
Read Also: Rare Types Of Bladder Cancer
For Pop Surgery Experience Counts
Although some women are fearful of POP surgery, its a safe and effective treatment option. Virtua has experienced, board-certified female pelvic medicine specialists with specific expertise in pelvic support surgery.
If POP is affecting your quality of life, you dont have to live with ityour doctor can help.
Get more information about female pelvic medicine at Virtua, or call to schedule a consultation with a Virtua female pelvic medicine specialist.
For more information about POP, visit Voices for PFD.
How Do I Prepare For My Vaginal Prolapse Surgery
You are an important member of your own healthcare team. The steps you take before surgery can improve your comfort and outcome.
You can prepare for vaginal prolapse surgery by:
-
Answering all questions about your medical history, allergies, and medications. This includes prescriptions, over-the-counter drugs, herbal treatments, and vitamins. It is a good idea to carry a current list of your medical conditions, medications, and allergies at all times.
-
Getting preoperative testing as directed. Testing will vary depending on your age, health, and specific procedure. Preoperative testing may include a chest X-ray, EKG , blood tests, and other tests as needed.
-
If you are overweight, talk to your doctor about losing weight before surgery through a healthy diet and exercise plan.
-
Losing excess weight before the surgery through a healthy diet and exercise plan
-
Not eating or drinking before surgery as directed. Your surgery may be cancelled if you eat or drink too close to the start of surgery because you can choke on stomach contents during anesthesia.
-
Stopping smoking as soon as possible. Even quitting for just a few days can be beneficial and help the healing process.
-
Taking or stopping medications exactly as directed. This may include not taking aspirin, ibuprofen , and blood thinners.
Questions to ask your doctor
It is also a good idea to bring a list of questions to your appointments. Questions can include:
You May Like: What Causes Bladder Spasms With Catheter
If You Have Urinary Retention And Need Intermittent Catheters Check Out Compactcath
CompactCath is a revolutionary pocket-sized catheter that is discreet, light, no-touch, and pre-lubricated with anti-bacterial silicone oil. Some of our customers reported having fewer infections since switching to CompactCath. Request free samples and read our reviews on reviews.io.
Ive found particularly useful in work and social situations where you want to duck into a bathroom to cath but dont want to make a big deal of getting your handbag and lugging everything into a small stall. It can be stowed in your pocket for a quick cath without the drama CompactCath is definitely a must-have addition to my cathing supply
- 1755 E Bayshore Road, Suite 10A & 10B, Redwood City, CA 94063
- support@compactcath.com
Causes Of Pelvic Organ Prolapse
Pelvic organ prolapse happens when the group of muscles and tissues that normally support the pelvic organs, called the pelvic floor, becomes weakened and cannot hold the organs in place firmly.
A number of things can weaken your pelvic floor and increase your chance of developing pelvic organ prolapse.
These include:
- pregnancy and childbirth especially if you had a long, difficult birth, or if you gave birth to a large baby or multiple babies
- getting older and going through the menopause
- being overweight
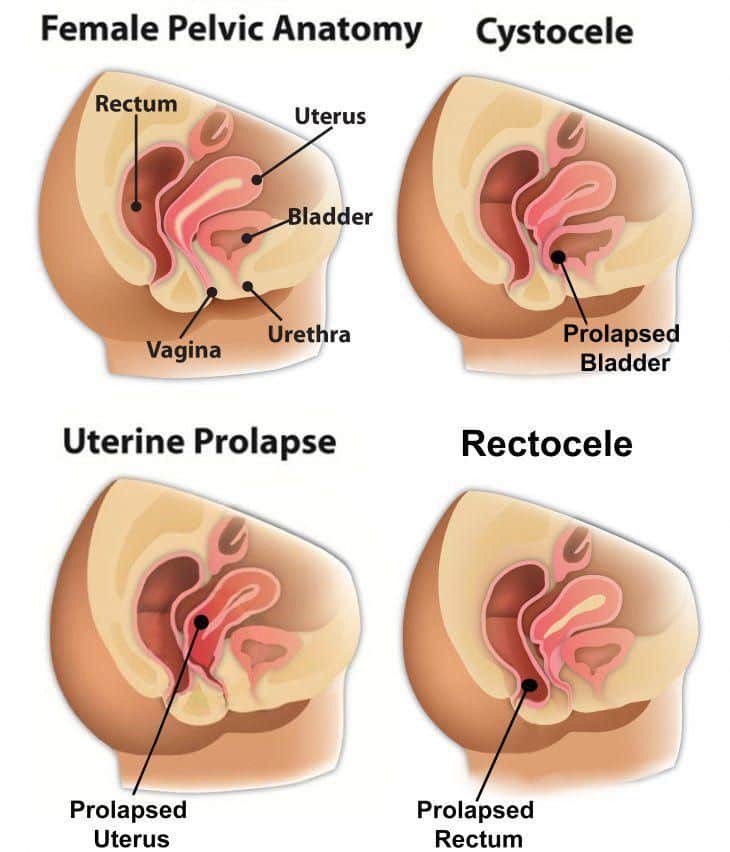
The 4 main types of prolapse are:
It’s possible to have more than 1 of these at the same time.
Pelvic organ prolapse will usually be classified on a scale of 1 to 4 to show how severe it is, with 4 being a severe prolapse.
Page last reviewed: 24 March 2021 Next review due: 24 March 2024
Also Check: Can Endometriosis Cause Bladder Problems
What Happens At Your Appointment
Your doctor will ask if they can do an internal pelvic examination.
For this you’ll need to undress from the waist down and lie back on the examination bed.
Sometimes they’ll ask you to lie on your left-hand side and examine you in that position to get a better view of the prolapse.
You can ask for this examination to be done by a female doctor and, if you like, bring someone you trust along with you for support.
Where Can I Go To Find Out More Information Or Get Treatment
The Division of Urogynecolgy in the Department of Obstetrics and Gynecology at the University of Michigan is committed to providing consultation services, comprehensive treatment planning and a broad range of services for patients with urinary incontinence, pelvic organ prolapse, fecal incontinence and other conditions associated with the pelvic floor. For further information, you can contact us at 734-763-6295.
Recommended Reading: Bladder Exercises For Overactive Bladder
Recognizing The Symptoms Of Uterine Prolapse
There are several symptoms related to pain including:
- Pain or discomfort in the pelvic area
- Pain during sex
Symptoms relating to urinary function include:
- Difficulty urinating or with bowel movements
- Urinary incontinence
- Incomplete voiding
Painful or bleeding tissue protruding is one of the most obvious signs. However, women suffering from a very mild uterine prolapse or early-stage uterine prolapse may experience few, if any, symptoms.
How Is A Cystocele Diagnosed
The doctor may also perform certain tests, including the following:
- Urodynamics: Measures the bladders ability to hold and release urine.
- Cystoscopy : A long tube-like instrument is passed through the urethra to examine the bladder and urinary tract for malformations, blockages, tumors, or stones.
Don’t Miss: Does A Bladder Infection Cause Incontinence
Stages Of Bladder Prolapse
The severity of bladder prolapse can be measured in several ways. Terms such as mild, moderate and severe are not always completely accurate, as they depend on a persons opinion, but are often used in day-to-day conversations to help people understand the severity of the prolapse.A more commonly used grading is:
Many gynaecologists now use the Pelvic Organ Prolapse Quantification system, which measures in centimetres where the prolapse is in relation to the vaginal entrance to ascertain the stage of prolapse.
How Can I Prevent Pelvic Organ Prolapse
Researchers are studying ways to prevent pelvic organ prolapse. The following steps may reduce your risk of getting a pelvic floor problem:
- Maintain a healthy weight or lose weight . Women who have overweight or obesity are more likely to have pelvic floor problems.
- Choose foods with fiber. Fiber helps prevent constipation and straining during bowel movements. Preventing constipation may reduce the risk of some pelvic floor disorders.
- Do not smoke. Smoking can lead to chronic cough, which puts stress on the pelvic floor muscles.
Read Also: Cranberry Supplements For Bladder Infection
What Do I Need To Bring To My First Visit
Fill out the questionnaire sent to your home prior to your visit or fill out the questionnaire at your first appointment. This is a long questionnaire, but it asks important questions about your reproductive and general health and family history. This information will help us help you.
Please bring relevant and important medical records, radiology reports or laboratory reports. We ask that you do not send or fax records to our clinic. Please hand-carry all medical records to your first visit.
How Will I Be Evaluated
When you see your doctor, you will have a health history taken in order to get a thorough explanation of your symptoms. A pelvic exam is necessary to diagnose pelvic organ prolapse. If you do have prolapse, the urogynecologist will determine which organs are involved and how severe the prolapse is. Other tests might be ordered, based on your individual examination.
Read Also: Is High Grade Bladder Cancer Curable
What Can I Expect At My First Visit
- The doctor will review your questionnaire and conduct a thorough history of your symptoms as well as some physical exams and tests
- Evaluation of pelvic support
- Evaluation for loss of urine or stool
- Possible placement of a catheter in your bladder to check for the amount of urine left after you void
- Neurological exam
- Discussion with your physicians about your diagnosis and possible treatment options
- Make follow-up appointments or schedule surgery
When Is Surgery Needed For A Prolapsed Bladder
Severe prolapsed bladders that cannot be managed with a pessary and/or behavioral therapy usually require surgery to correct them. There are several different types of surgery depending on the severity of the prolapse and whether or not other organs are affected.
- The bladder is repaired with an incision in the vaginal wall.
- The prolapsed area is closed and the wall is strengthened. This may be done primarily using one’s own tissues or through the use of grafts, which may be biologic or synthetic .
- If one has stress urinary incontinence, this is also corrected.
- Depending on the procedure, surgery can be performed while the woman is under general, regional, or local anesthesia. Most women are discharged home on the same day of surgery.
- Various materials have been used to strengthen pelvic weakness associated with prolapsed bladder. A surgeon should explain in detail the risks, benefits, and potential complications of these materials, and he or she should explain the procedure itself before proceeding with the surgery. Complications related to surgery may include bleeding, infection, pain, urinary incontinence, recurrent prolapse, trouble urinating, and injury to the bladder.
- The cost of surgical treatment will vary with the procedure performed, the length of hospitalization, and the presence/absence of other medical conditions.
- After surgery, most women can expect to return to a normal level of activity after 6 weeks.
Read Also: Can You Get Bladder Infection From Intercourse