Fda Grants Priority Review To Keytruda For Patients With High
On December 2, 2019, Merck announced that the FDA has granted priority review for its supplemental biologics license application for the antiPD-1 agent pembrolizumab . If approved, the drug would be indicated as monotherapy to treat patients with Bacillus Calmette-Guerinunresponsive, high-risk, nonmuscle-invasive bladder cancer who are ineligible for or have decided not to undergo cystectomy.
The filing was based on data from the multicenter, open-label, single-arm, phase 2 KEYNOTE-057 clinical trial of 102 patients with Bacillus Calmette-Guerinunresponsive, high-risk, nonmuscle-invasive bladder cancer with carcinoma in situ with or without papillary tumors who were ineligible for or had decided not to undergo cystectomy.
Major efficacy outcome measures were complete response and duration of response. Patients received 200 mg of pembrolizumab every 3 weeks for up to 24 months or until unacceptable toxicity, progressive disease, or detection of persistent or recurrent high-risk nonmuscle-invasive bladder cancer.
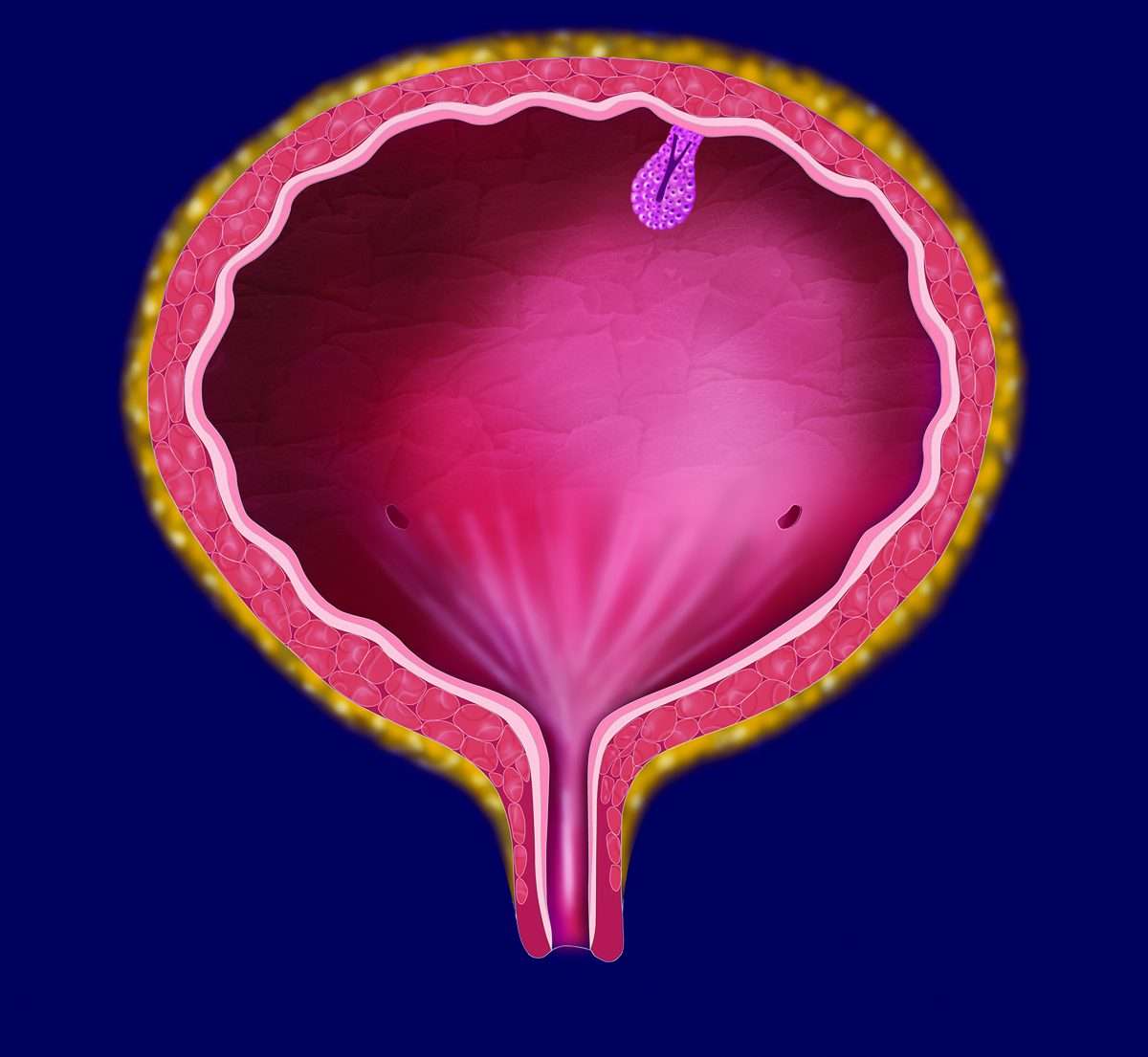
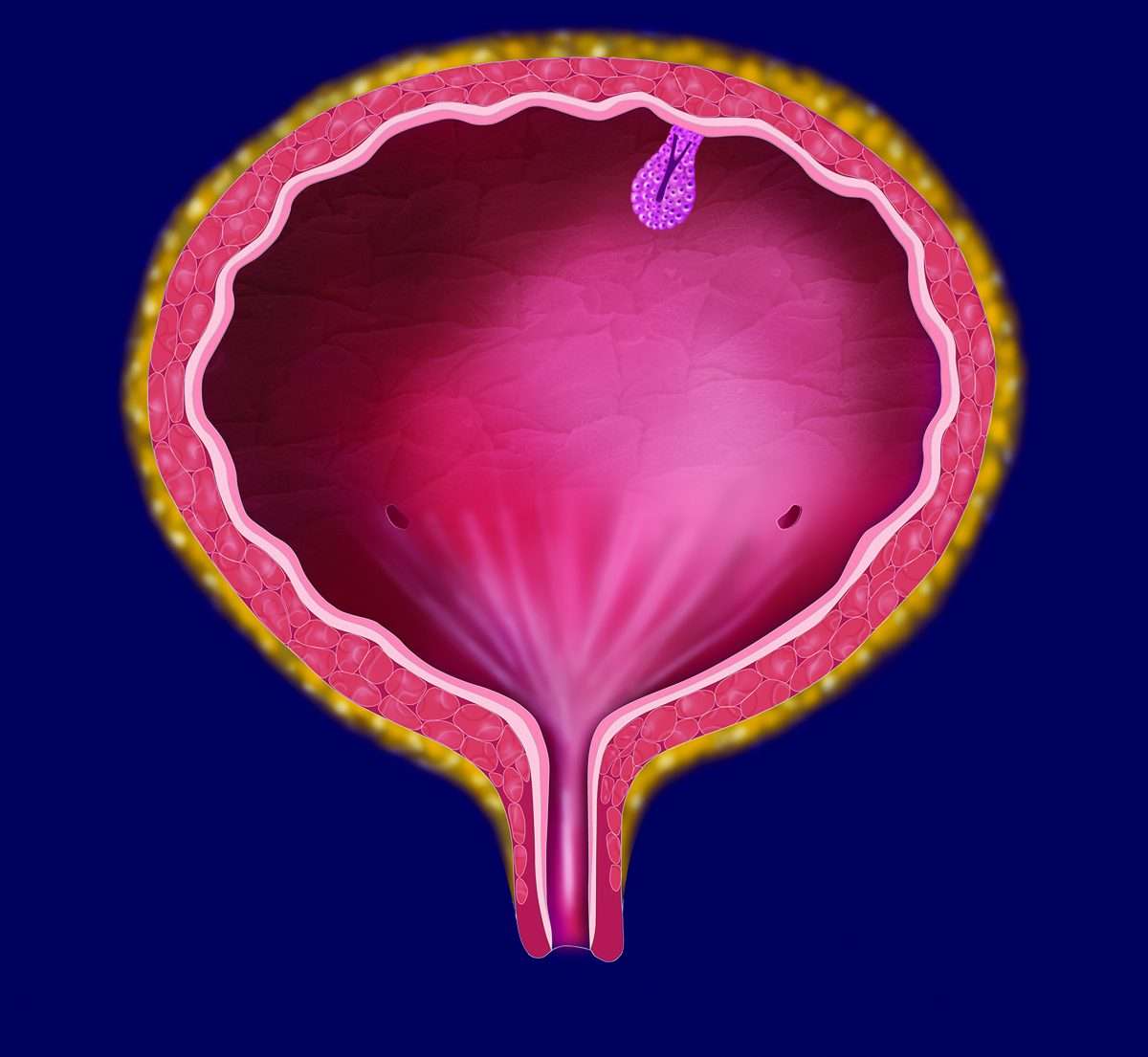
It is estimated that > 80,000 new cases of bladder cancer will be diagnosed in 2019 in the United States. Approximately 75% of these patients are diagnosed with nonmuscle-invasive bladder cancer, which means that the cancer cells have not grown into the main muscle layer of the bladder. Patients with high-grade nonmuscle-invasive bladder cancer are at high risk for developing muscle-invasive and metastatic disease.
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
Guideline Statement 24
Discussion
Guideline Statement 25
Discussion
Guideline Statement 26
Intravesical Immunotherapy With Bcg
BCG is a live attenuated strain of Mycobacterium bovis, originally developed as a vaccine for tuberculosis. There are several strains available from different manufacturers with the commonest used in the UK being Oncotice BCG®. The content of a vial is reconstituted with 50 ml of saline and then administered through a urethral catheter to remain in the urinary bladder for about 2 h time. The mechanism of action is incompletely understood but it is postulated to work via a local immune response characterised by induced expression of cytokines in the urine and bladder wall . Before starting BCG in new patients, it is important to adequately debulk all visible tumour and re-resect T1 high grade tumours to reduce understaging. BCG strain may have an impact on treatment outcome in NMIBC immunotherapy. A recent prospective randomised study of 142 high-risk NMIBC patients with two of the commonest BCG strains showed that treatment with BCG Connaught conferred significantly greater 5-year recurrence-free survival compared with treatment with BCG Tice .
Don’t Miss: Natural Bladder Control For Men
Publication History And Summary Of Changes
1.4.1. Publication history
The EAU Guidelines on Bladder Cancer were first published in 2000. This 2022 NMIBC Guidelines document presents a limited update of the 2021 publication.
1.4.2. Summary of changes
Additional data has been included throughout this document text. In particular in Chapters/Sections:
- 5.4 Imaging with the introduction of Vesical Imaging-Reporting and Data System ).
- 5.7.3 Surveillance of non-muscle-invasive bladder cancer inclusion of urine biomarkers in a surveillance strategy of an individual patient.
- 5.8 Cystoscopy inclusion of the procedural chance . The recommendation was amended accordingly.
|
Recommendations |
Strength rating |
|
In men, use a flexible cystoscope, if available and apply irrigation bag squeeze to decrease procedural pain when passing the proximal urethra. |
Strong |
- 5.10.2.2 Evaluation of resection quality, resulting in a recommendation change.
|
Recommendations |
Quality Assessment Sensitivity And Publication Bias
To verify how individual studies influenced the pooled results, a sensitivity analysis was performed by eliminating one study at a time. No serious publication bias was found according to the funnel plots . Among all the enrolled publications, three of them were prospective trials . Therefore, we utilized Cochrane Collaborations risk of the bias assessment tool to assess the risk of bias in these three studies. All the three studies reported to use the randomization methods, but two of them did n not mention details . Only one studies described allocation concealment , and none of them reported blind method in the researches. The assessment of risk of the bias was shown in Figures 3, 4.
FIGURE 3. Risk of bias graph depicting each risk of bias item as percentages across prospective studies.
FIGURE 4. Risk of bias summary.
Don’t Miss: Can Endometriosis Affect Your Bladder
Risk Adjusted Surveillance And Follow
Guideline Statement 32
32. After completion of the initial evaluation and treatment of a patient with NMIBC, a clinician should perform the first surveillance cystoscopy within three to four months.
Discussion
The natural history of NMIBC is often characterized by recurrence, even for solitary, small, low-grade papillary tumors. At the time of first evaluation and treatment, none of the existent risk stratification tools or urinary biomarkers is sufficiently sensitive and specific to predict which patient will have an early tumor recurrence. Therefore, the only reliable way to know in a particular patient whether they are at risk for early recurrence is by cystoscopic visualization of the urothelium at a relatively early interval after the first treatment/resection. In addition, visualization at a relatively early interval allows the treating urologist to verify that the initial resection was complete. The Panel, therefore, felt that the first repeat cystoscopic evaluation should occur three to four months after the initial treatment and evaluation, regardless of the patient’s overall risk.
Guideline Statement 33
33. For a low-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent surveillance cystoscopy six to nine months later, and then annually thereafter surveillance after five years in the absence of recurrence should be based on shared-decision making between the patient and clinician.
Discussion
Discussion
Risk Stratification Based On Clinical And Pathological Parameters
Table 1 summarizes the available predictive models to predict recurrence and progression in patients with NMIBC. The most important risk factor for progression is grade, not stage, because patients with high-grade tumors progress with similar frequency regardless of whether they were invasive or non-invasive . Millan-Rodriguez et al. evaluated a cohort of 1529 primary NMIBC patients treated with transurethral resection and random bladder biopsy and identified prognostic factors for recurrence, progression and disease-specific mortality . Multivariate analysis demonstrated that the main prognostic factors of recurrence were multiplicity, tumor size > 3 cm, presence of CIS and treatment with bacillus CalmetteGuerin . The prognostic factors for progression were grade 3 disease, multiplicity, tumor size > 3 cm, CIS and treatment with BCG. Furthermore, the prognostic factors for mortality were presence of grade 3 disease and CIS.
Read Also: How To Control My Bladder
Study Selection And Characteristics
A total of 1,539 original publications were retrieved through systematic search, among them 514 were excluded as repeated records. After manual selection for titles, abstracts, and full-text articles, we enrolled seven eligible studies involving 1,247 patients who are pathologically diagnosed with NMIBC after bladder-preserving surgery . The detailed process of the studies selection was shown in Figure 1.
FIGURE 1. Flowchart for article selection.
Among these researches, three of them was prospective studies, and all the studies was performed in the Chinese hospital. In total, 511 high risk NMIBC patients received IVC and subsequent IAC regimen, while 736 underwent intravesical installation alone. Most of the studies administered similar IAC regimen , and the interval time between each cycle ranged from 3 to 6 weeks. The detailed characteristics and drug usage of each enrolled study was listed in Table 1. And the final pooled results of all studies were displayed in Table 2.
TABLE 1. Characteristics of included studies.
TABLE 2. Summary of therapeutic efficacy and survival outcomes.
Second Turbt And Subsequent Management
Generally, the second TURBT under WL was performed within 2âmonths of the first TURBT. The second TURBT involved resectioning the bottom of the tumor and the surrounding mucosa, centering on the previously resected area. Subsequently, intravesical recurrence was evaluated over 2âyears of regular medical examinations performed as a daily clinical practice. Postoperative adjuvant therapy was mainly intravesical bacillus Calmette-Guerin infusion therapy, per the bladder cancer clinical practice guidelines.
Also Check: Stage One Bladder Cancer Treatment
Electromotive Intravesical Drug Administration
Electromotive drug administration uses an electric current to enhance transepithelial drug penetration . EMDA is administered via a battery-powered generator delivering an electric current of 030 mA DC at 055 V, which is passed between two electrodes. An active electrode is placed into the bladder as part of a transurethral catheter and dispersive ground electrode pads are placed on the skin of the lower abdomen .
The penetration of MMC into the bladder wall with EMDA is significantly greater than that achieved by passive diffusion as shown in in vitro studies . In clinical practice, EMDA MMC has been shown to be safe with no life-threatening adverse events. Most reports on EMDA have focussed on its role following first TURBT and there are limited reports of its use in high-risk patients.
In one such study, Di Stasi et al. reported a prospective RCT of 108 patients who were randomised into three equal groups of 36 each who underwent 40 mg electromotive MMC instillation with 20 mA electric current for 30 min, 40 mg passive MMC with a dwell time of 60 min or 81 mg BCG with a dwell time of 120 min. The complete response for electromotive versus passive MMC at 3 and 6 months was 53 versus 28 % and 58 versus 31 % . For BCG, the responses were 56 and 64 %. Median time to recurrence was 35 versus 19.5 months and for BCG it was 26 months .
Relevance Of The International Bcg Shortage To The Aua Guidelines
The global shortages in TICE BCG that occurred in 2014 and 2019 led the AUA to recommend several management strategies to maintain high quality care for patients with NMIBC. These recommendations may supersede the guideline statements below. In particular, the BCG shortage impacts guideline statements 17, 20, and 21. The AUA Statement on the BCG Shortage is available at .
Don’t Miss: Can Leukemia Cause Bladder Problems
Outcome Measurements And Statistical Analysis
We assessed oncological outcomes for patients who underwent RC according to the natural history of their BC. primHR-NMIBC and primMIBC were defined as no prior history of BC, and recHR-NMIBC and secMIBC as previously treated NMIBC that recurred or progressed to MIBC, respectively. Log-rank analysis was used to compare survival outcomes, and univariable and multivariable Cox and logistic regression analyses were used to identify predictors for survival.
Inclusion And Exclusion Criteria
Seven eligible studies were selected in accordance with the PICOS principle. 1) population:patients with pathologically confirmed high-risk NMIBC 2) intervention: patients treated with IAC + IVC regimen 3) comparison: treated with intravesical installation alone 4) outcomes: prognosis indicators including tumor recurrence rate, tumor progression rate, survival rate, tumor-specific death rate, adverse events and time to first tumor recurrence 5) study design: any studies related to this subject including prospective or retrospective studies or randomized controlled trial. Eligible studies should meet the following criteria:1) patients underwent bladder-preserving surgery 2) pathologically confirmed high-risk NMIBC 3) interventions were IAC + IVC 4) sufficient data that includes tumor recurrence rate, tumor progression rate, survival rate, or cancer-specific survival 5) prospective or retrospective cohort studies or randomized controlled trial 6) published with the English language. Studies involving radical cystectomy, neoadjuvant treatment, immunotherapy, and unsuitable types such as reviews, case reports, editorials, and letters were excluded.
Also Check: How To Treat A Leaky Bladder
Pembrolizumab In Bladder Cancer
- Pembrolizumab was approved for treatment of patients with Bacillus Calmette-Guérinunresponsive, high-risk, nonmuscle invasive bladder cancer with carcinoma in situ with or without papillary tumors who are ineligible for or have elected not to undergo cystectomy.
- The recommended dose of pembrolizumab in patients with high-risk BCG-unresponsive nonmuscle invasive bladder cancer is 200 mg via intravenous infusion over 30 minutes every 3 weeks until persistent or recurrent high-risk nonmuscle invasive bladder cancer, disease progression, unacceptable toxicity, or for up to 24 months in patients without disease progression.
Product labeling provides recommended dosing modifications, including withholding, resuming, and discontinuing treatment for the following adverse reactions: immune-mediated pneumonitis, colitis, endocrinopathies, nephritis, skin adverse reactions, and hepatitis in patients with and without hepatocellular carcinoma liver enzyme elevations in patients with renal cell carcinoma receiving combination therapy hematologic toxicity in patients with classical Hodgkin lymphoma or primary mediastinal large B-cell lymphoma inability to taper corticosteroid treatment persistent grade 2 or 3 adverse reactions and infusion-related reactions.
Safety Profile
REFERENCES
Data Collection And Analysis
Patient data from each institution were collected and analyzed by electronic data capture using the REDCap system. All endpoints were analyzed with a per-protocol set, which excluded ineligible cases, cases without endpoint data, and cases that deviated from the research protocol.
The primary endpoint and patient background data were locked in February 2021 and analyzed. Propensity score matching analysis was conducted for the primary endpoints. Propensity scores were calculated for the initial PDD-TURBT group and the initial WL-TURBT group by using the background factors of age, sex, tumor diameter, history of bladder cancer, and the number of tumors. Pair matching was performed by setting the caliper to 0.2, and the primary endpoints were compared between the postmatching groups using Fisherâs exact test. Logistic regression analysis was also performed to identify the factors that affected the primary endpoint. The free software EZR ver. 1.54 was used for the statistical analysis. The significance level of the tests was 5% on both sides, and the confidence interval estimation was 0.95.
You May Like: Bladder Tumor Removal Surgery Recovery
Role Of Cystectomy In Nmibc
Guideline Statement 27
27. In a patient with Ta low- or intermediate-risk disease, a clinician should not perform radical cystectomy until bladder-sparing modalities have failed.
Discussion
Low-grade, noninvasive tumors very rarely metastasize, and even large-volume, multifocal cancers can usually be managed with techniques, such as staged resection. Patients with low-grade recurrences can be successfully managed with intravesical chemotherapy 225 or BCG. 177,226,227 In addition, small, multifocal recurrences despite intravesical therapy can usually be treated effectively with office fulguration, repeat TURBT or even surveillance, in select cases. 64-67
Guideline Statement 28
28. In a high-risk patient who is fit for surgery with persistent high-grade T1 disease on repeat resection, or T1 tumors with associated CIS, LVI, or variant histologies, a clinician should consider offering initial radical cystectomy.
Discussion
Guideline Statement 29
29. In a high-risk patient with persistent or recurrent disease within one year following treatment with two induction cycles of BCG or BCG maintenance, a clinician should offer radical cystectomy.
Intravesical Chemotherapy With Hyperthermia
Thermal energy appears to improve the absorption of several intravesical agents, and as such adjunctive hyperthermia has been shown to increase cytotoxicity in bladder cells in in vitro and animal models . Several devices are available to deliver thermochemotherapy for NMIBC with the commonest used heat delivery system being Synergo® . This machine delivers local hyperthermia in conjunction with intravesical chemotherapy using a 915-MHz intravesical radiofrequency energy applicator placed on a thermocouple-controlled 20 F urethral catheter . Other HT systems include the BSD-2000 , the ALBA hyperthermia system , the BWT system by Elmedical, the Sonotherm 1000 and the Combat BRS system .
A recent systemic review and meta-analysis of 22 trials examining intravesical chemohyperthermia for NMIBC showed a 59 % reduction in recurrence rate for TURB + CHT compared to TURBT + chemotherapy alone . However, due to short follow-up, no conclusions could be drawn about time to recurrence and progression. In addition, the overall bladder preservation rate after CHT was 87.6 %.
In one of the few studies with long-term follow-up, Colombo et al. reported on a cohort of 83 patients with intermediate/high grade NMIBC with a median follow-up of 91 months . They showed a significantly better 10-year disease-free survival rate for thermochemotherapy . Bladder preservation rates for thermochemotherapy were also significantly higher .
Recommended Reading: How To Control Overactive Bladder Naturally
Risk Stratification Based On Molecular Biomarkers
For molecular biomarkers to be of clinical use, they should be able to increase the predictive accuracy beyond the standard clinical and pathological parameter models. Several investigators have attempted to use molecular biomarkers as prognostic factors to predict outcomes in patients with NMIBC. However, molecular biomarkers have shown mixed results so far and are not sufficiently validated to be used in clinical practice at this time.
It is becoming clear that superficial low-grade cancers and invasive or high-grade cancers harbor distinctive genetic defects: The low-grade, non-invasive papillary tumors are characterized by activating mutations in the H-Ras gene and fibroblast growth factor receptor 3 gene and the high-grade invasive tumors are characterized by structural and functional defects in the p53 and retinoblastoma protein tumor-suppressor pathways. The deletion of both arms of chromosome 9 occurs frequently in bladder cancer during the earliest stages of tumorigenesis. However, these chromosomal aberrations do not seem to distinguish between the two tumor development pathways. Tumor invasion and progression in the bladder seems to be a multifactorial process, promoted by micro-environmental changes that include the up-regulation of N-cadherin, the down-regulation of E-cadherin, the overexpression of matrix metalloproteinases 2 and 9, an imbalance between angiogenic and anti-angiogenic factors and increased synthesis of prostaglandin.