Other Terms Often Used To Describe Bladder Cancer
Although bladder cancer types are assigned based on the cells that the cancer originates from, several other terms may be used to describe the disease.
- Advanced bladder cancer is another term that may be used to describe metastatic bladder cancer. It means that the cancer has spread to distant parts of the body such as the lungs, bones, liver, or lymph nodes outside the pelvis.
- Locally advanced bladder cancer refers to cancer that has grown through the bladder wall, and possibly into nearby lymph nodes or organs, but has not spread to distant sites in the body.
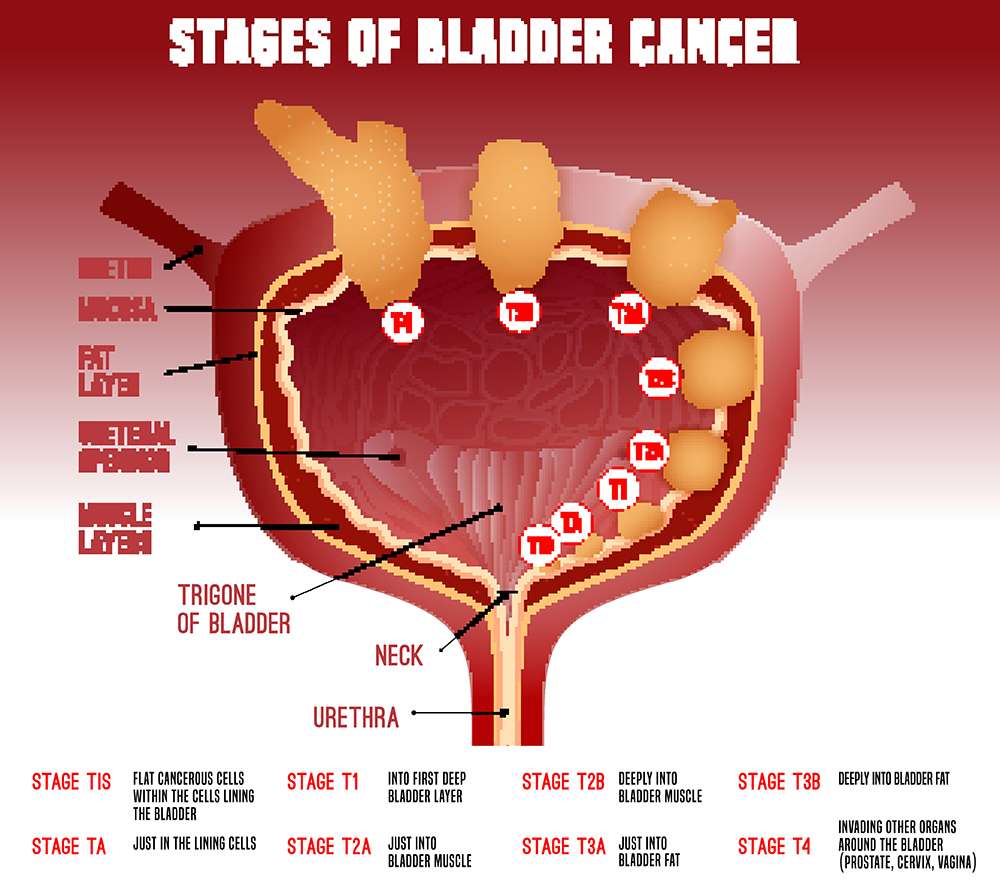
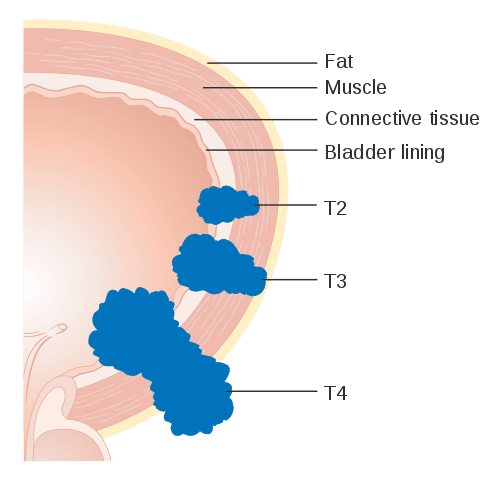
- Bladder cancer stage describes where the cancer is located within the bladder and any sites of spread. As described above, the TNM staging system assigns a patients bladder cancer to a tumor , lymph node and metastasis category. These categories may also be combined to give an overall stage number: an overall stage of 0 or 1 describes early disease, while stage 4 is the most advanced. For further information regarding staging, see Bladder Cancer Stages.
- Bladder cancer grade is based on the microscopic appearance of cancer cells and suggests how fast a cancer might grow. Low-grade cancer cells appear similar to normal cells and usually grow slowly, whereas high-grade cancer cells have a very abnormal appearance and tend to grow quickly. High-grade cancers are more likely than low-grade cancers to spread.
Tests To Check You Are Fit For Surgery
You have tests before your operation to check:
- your fitness for an anaesthetic, if you need one
- that youll make a good recovery from surgery
You might have some or all of the following tests:
- blood tests to check your general health and how well your kidneys are working
- a swab test to rule out some infections
- an ECG to check that your heart is healthy
- breathing tests
- an echocardiogram
- a chest x-ray to check that your lungs are healthy
- a test to check your heart and lung function when you’re resting and exercising
You also have a blood test to match your blood for any transfusions you might need during your surgery.
Amplification Deletion And Other Genomic Events In Bladder Cancer
Many comprehensive studies have identified numerous genomic amplification and deletion events occurring in bladder cancer . These findings were confirmed and extended in the recent TCGA analysis based upon Affymetrix SNP profiling and low-pass whole-genome sequencing, both analyzed by GISTIC . Thirteen genes were targets of focal deletion and 19 were targets of focal amplification . The majority of those genes fall into the same categories as those for which mutations are seen, including cell cycle, chromatin regulation, receptor tyrosine kinase signaling, and transcription.
In TCGA dataset, 3 invasive bladder cancers contained FGFR3TACC3 fusion sequences , a chromosomal translocation identified previously in bladder cancer . These fusion proteins are highly transforming. They have now been seen in multiple cancer types, and cancers bearing them may be especially sensitive to FGFR3 inhibitors. Four cancers had fusions involving ERBB2 and various other genomic regions of uncertain functional significance .
Also Check: Device To Stop Bladder Leakage
Causes Of Bladder Cancer
Most cases of bladder cancer appear to be caused by exposure to harmful substances, which lead to abnormal changes in the bladder’s cells over many years.
Tobacco smoke is a common cause and it’s estimated that more than 1 in 3 cases of bladder cancer are caused by smoking.
Contact with certain chemicals previously used in manufacturing is also known to cause bladder cancer. However, these substances have since been banned.
Read more about the causes of bladder cancer.
Invasive Bladder Cancer: Genomic Insights And Therapeutic Promise
*Corresponding Authors:*Corresponding Authors:Corresponding Authors:
Jaegil Kim, Rehan Akbani, Chad J. Creighton, Seth P. Lerner, John N. Weinstein, Gad Getz, David J. Kwiatkowski Invasive Bladder Cancer: Genomic Insights and Therapeutic Promise. Clin Cancer Res 15 October 2015 21 : 45144524.
Recommended Reading: Antimuscarinic Drugs For Overactive Bladder
What Other Types Of Bladder Cancer Are There
Several less common types of bladder cancer make up the remaining approximately 10% of bladder cancers. Some examples of the uncommon types include:
- Squamous cell carcinoma: Squamous cells develop in the lining of the bladder as a result of irritation or inflammation. These cells may eventually become cancerous. Although squamous cell carcinoma is uncommon, making up around 4% of all bladder cancers,2 it has a high likelihood of progression.
- Adenocarcinoma: This type of bladder cancer consists of glandular-type cells and is usually invasive. Overall, around 2% of bladder cancers are adenocarcinomas.2
- Small cell carcinoma: Small cell carcinomas of the bladder start in nerve-like cells. This bladder cancer type is rare, accounting for less than 1% of bladder cancers,4 but can grow rapidly and spread to other parts of the body.
- Sarcoma: A sarcoma is a type of cancer that begins in the bodys supporting tissues, such as bone, muscle, fibrous tissues, and fat. Very rarely, sarcomas may arise from the muscle or fat layers of the bladder.
Although the treatment for most bladder cancer types is similar for early-stage tumors, different drugs may be used if chemotherapy is undertaken.
Prognostic Nomograms For Muscle
As detailed earlier in this chapter, the TNM staging system provides valuable prognostic information following radical cystectomy. Despite its usefulness, there is often wide variation among patients with regard to absolute risk for recurrence as a result of the heterogeneity of tumor biology and patient characteristics. Better understanding and prediction of disease outcome is important to deliver appropriate adjuvant therapy and to counsel patients with regard to the risk for disease recurrence. The use of standard pathological data to predict outcomes was discussed earlier in this chapter. Nomograms have been developed in an effort to better predict the prognosis in patients with muscle-invasive disease . In addition to standard pathological features, molecular markers are now being incorporated into predictive models not only to improve prognostic accuracy, but also to provide the potential to predict response to therapy .
RICHARD J. COTE, … MAHUL B. AMIN, in, 2009
Don’t Miss: High Grade Non Invasive Bladder Cancer
What Causes Bladder Cancer
Healthcare providers and researchers dont know exactly why certain bladder cells mutate and become cancerous cells. Theyve identified many different risk factors that may increase your chance of developing bladder cancer, including:
- Cigarette smoke: Smoking cigarettes more than doubles your risk of developing bladder cancer. Smoking pipes and cigars and being exposed to second-hand smoke may also increase your risk.
- Radiation exposure: Radiation therapy to treat cancer may increase your risk of developing bladder cancer.
- Chemotherapy: Certain chemotherapy drugs may increase your risk.
- Exposure to certain chemicals: Studies show that people who work with certain chemicals used in dyes, rubber, leather, paint, some textiles and hairdressing supplies may have an increased risk.
- Frequent bladder infections: People who have frequent bladder infections, bladder stones or other urinary tract infections may be at an increased risk of squamous cell carcinoma.
- Chronic catheter use: People who have a chronic need for a catheter in their bladder may be at risk for squamous cell carcinoma.
Urinary Mutdna Demonstrates Tumour Evolution On
As opposed to assays targeting mutations detected in matched tumour samples, combined use of our disease specific assay and sWGS allowed the detection of de novo mutations. To determine additional examples of tumour evolution we performed sWGS analysis of samples taken between the first and last time-points in selected patients based on high SNV levels or interesting CNA profiles at the first time-point . In 5 patients there was evidence of dynamic tumour evolution during NAC, highlighting the strength of studying mutDNA in peripheral fluids as an alternative to traditional biopsy approaches, . All de novo mutations were detected in the urinary specimens and were not detected in the initial tumour specimen. There was no correlation between the detection of these private mutations and clinical outcome.
Figure 5
You May Like: Is Caffeine A Bladder Irritant
Appendix A: Search Strategy
Primary Search Strategy for Emerging Approaches to Diagnosis and Treatment of Non-Muscle-Invasive Bladder Cancer and Treatment of Non-metastatic Muscle-invasive Bladder Cancer
Choosing An Adjuvant Treatment
For patients with low-risk NMIBC, it is recommended that adjuvant therapy with a single instillation of perioperative chemotherapy be considered. It is critical that intravesical chemotherapy is not given in the setting of a bladder perforation because extravasation of chemotherapy into the peritoneum is a devastating complication. Therefore, a high-level of suspicion during extensive resections and completion of a cystogram prior to chemotherapy instillation is essential. The recommendation for a single dose of chemotherapy post-TURBT is supported by meta-analyses that demonstrate an approximately 15% reduction of recurrence with instillation of mitomycin or epirubicin compared with TURBT alone in low-risk disease.24 An alternative option is perioperative gemcitabine. A randomized trial of peri-TURBT gemcitabine versus saline demonstrated a reduction in 4-year recurrence rate from 54% to 34% with few adverse effects among 215 patients with low-grade NMIBC.25
Don’t Miss: Can Bladder Infection Be Caused By Intercourse
Tests That May Be Done
Physical exam: The doctor will check you for signs of bladder cancer and other health problems. This might include a rectal exam, during which a gloved finger is put into your rectum. If you are a woman, a pelvic exam might also be done. During these exams, the doctor can sometimes feel a bladder tumor.
Urine tests: For these tests, you’ll be asked to pee in a cup. Your urine is then tested for cancer cells, blood, or certain proteins .
Cystoscopy: For this exam, a doctor called a urologist looks at the inside of your bladder using a tool called a cystoscope. This is a thin tube with a tiny light and camera on its end. It’s put through the opening of your urethra and moved up into your bladder.
Blue light cystoscopy: Sometimes, special drugs are put into the bladder during the exam. Cancer cells soak up these drugs and then glow when the doctor shines a blue light through the scope. This can help the doctor see cancer cells that might have been missed with the normal light.
Bladder biopsy: This is needed to know for sure if you have bladder cancer. For this test, a cystoscope is used it to take a tiny piece of the bladder . More than one sample may be taken because sometimes cancer starts in more than one part of the bladder. Salt water washings of the inside of your bladder may also be collected to look for cancer cells. Any samples are sent to a lab and tested to see if there are cancer cells in them.
Cystoscopy With Cautery Destruction Of The Bladder Tumor
Cystoscopy is an outpatient procedure during which a thin, lighted tube with a camera is passed through the urethra into the bladder, allowing your doctor to see the inside of the bladder.
Most modern cystoscopes are also equipped with channels that permit small instruments to be passed into the bladder. During a cystoscopy, your doctor may use these instruments to remove tissue, stop bleeding with a special electrical device called an electrocautery or even perform laser treatment. If the bladder cancer tumor is small enough, this cautery may be used to remove the cancer.
Also Check: Does Drinking Cranberry Juice Help A Bladder Infection
Relevance Of The International Bcg Shortage To The Aua Guidelines
The global shortages in TICE BCG that occurred in 2014 and 2019 led the AUA to recommend several management strategies to maintain high quality care for patients with NMIBC. These recommendations may supersede the guideline statements below. In particular, the BCG shortage impacts guideline statements 17, 20, and 21. The AUA Statement on the BCG Shortage is available at .
Treating Stage Iv Bladder Cancer
These cancers have reached the pelvic or abdominal wall , may have spread to nearby lymph nodes , and/or have spread to distant parts of the body . Stage IV cancers are very hard to get rid of completely.
Chemotherapy is usually the first treatment if the cancer has not spread to distant parts of the body . The tumor is then rechecked. If it appears to be gone, chemo with or without radiation or cystectomy are options. If there are still signs of cancer in the bladder, chemo with or without radiation, changing to another kind of chemo, trying an immunotherapy drug, or cystectomy may be recommended.
Chemo is typically the first treatment when bladder cancer has spread to distant parts of the body . After this treatment the cancer is rechecked. If it looks like it’s gone, a boost of radiation to the bladder may be given or cystectomy might be done. If there are still signs of cancer, options might include chemo, radiation, both at the same time, or immunotherapy.
In most cases surgery cant remove all of the cancer, so treatment is usually aimed at slowing the cancers growth and spread to help people live longer and feel better. If surgery is a treatment option, it’s important to understand the goal of the operation whether it’s to try to cure the cancer, to help a person live longer, or to help prevent or relieve symptoms from the cancer.
Because treatment is unlikely to cure these cancers, many experts recommend taking part in a clinical trial.
Read Also: Painful Bladder Syndrome Dietary Modification
What Questions Should I Ask My Doctor
Bladder cancer is relatively rare, so you may not know as much as youd like about the condition. Here are some questions that may be helpful:
- What stage of bladder cancer do I have?
- What are possible treatments?
- What are treatment side effects?
- Will I need surgery?
- How will surgery affect my daily life?
- How often does bladder cancer come back?
- How do you treat recurrent bladder cancer?
- Are there any cutting-edge clinical trials available?
A note from Cleveland Clinic
If you have bladder cancer, it may help to know about half of all people with the condition receive treatment when their tumors are limited to the inner layer of their bladder wall. For them, surgery to remove tumors means theyre cancer-free. But bladder cancer often comes back . If youre worried about recurring cancer, talk to your healthcare provider. Theyre your best resource for information on risk factors that increase the chance youll have another bout of bladder cancer. Theyll help you stay vigilant about symptoms that may be signs of recurring bladder cancer and be there for you if you need more bladder cancer treatment.
Last reviewed by a Cleveland Clinic medical professional on 08/26/2022.
References
Next Steps After Diagnosis
After receiving an NMIBC diagnosis, you may be wondering what to do next.
First, learn what you can about NMIBC and its treatment. Ask your doctor any questions you have, no matter how big or small.
Expect to feel a variety of strong emotions. You may need time to process your diagnosis. Reach out to trusted loved ones, and consider joining a support group.
If youre able, and if your doctors approve, try to exercise and get outdoors. Doing things you enjoy is important for maintaining your mental health during treatment and beyond.
Don’t Miss: High Risk Non Muscle Invasive Bladder Cancer
Detection Of Dna Alterations In Tur Samples From Mibc Patients Undergoing Nac
We performed TAm-Seq using a bladder-specific sequencing panel on all samples, for the analysis of SNVs, as previously described. The initial panel design included primers targeting the promoter region of TERT, but the resulting short amplicons did not perform well due to the repetitive sequences in this region and were excluded from further analysis. We detected a total of 22 SNVs across 12 of the 16 patients . The most frequent mutations detected were in TP53 , followed by KRAS , then PIK3CA . One SNV each was also detected in the BRAF, CTNNB1 and FGFR3 genes. These findings agree with previous studies annotating the frequency of SNVs in MIBC, . Though the numbers of SNVs detected in TUR samples varied amongst patients, there was no correlation with SNVs in TUR per patient and clinical outcome.
Figure 2
Furthermore, we developed an sWGS approach, adapted from published methods, to assess CNAs in TUR. Gross genome wide CNAs were detected in all tumour specimens, including for those 5 patients in whom no SNVs were observed . Across the 16 TUR samples, we detected focal CDKN2A loss , E2F3/SOX4 gain , PPARG gain , YWHAZ gain , CREBBP loss , MYCL1 gain and CNAs of other BC genes, as previously shown.
When To Contact A Doctor
A person not diagnosed with cancer should see a doctor regularly for routine health checks. This can include cancer screenings to check for early signs of potential cancer.
A person diagnosed with non-invasive cancer should see a doctor more frequently for checks. A doctor can check to see if the cancer has progressed or come back.
A person in treatment for invasive cancer should work with a doctor to determine how often they need medical appointments. They should do their best to keep all appointments and follow treatments as prescribed.
A person should contact a doctor if they notice any side effects from treatment. A doctor may be able to help them cope with the side effects.
Recommended Reading: How To Control Your Bladder At Night