Detecting Bladder Cancer With A Cystoscopy
Cystoscopy enables the inside of the urethra and bladder to be examined and sampled. Alongside urine testing and diagnostic imaging procedures, cystoscopy is used in both the initial diagnosis of bladder cancer and in ongoing surveillance for recurrence. In addition, cystoscopy-based procedures are commonly used to remove or treat small bladder tumors.
What Happens During A Cystoscopy
During flexible cystoscopy, the patient lies on their back and an anesthetic gel is passed into the urethra to make the area numb. Once the local anesthetic is working, the doctor inserts the cystoscope through the urethra and then into the bladder. Sterile water may be injected through the cystoscope into the bladder to help make the inner surface of the bladder easier to see. The cystoscope is moved around inside the bladder so that the entire inner surface can be examined.
During rigid cystoscopy, the procedure is similar to flexible cystoscopy but as the patient is usually under general anesthesia they will not be aware of any associated physical sensations. If the doctor sees an abnormal area, biopsies will be taken or a transurethral resection of bladder tumor may be carried out to remove the suspected tumor. The extracted tissues are then sent to a laboratory to be tested for cancer.
Monopolar Versus Bipolar Electrocautery
Both bipolar and monopolar electrocautery can be used for transurethral resection of bladder tumors. A recent study retroactively compared monopolar versus bipolar TURBT. The study examined perioperative complications in monopolar versus bipolar TURBT. They found that bipolar TURBT was associated with a lower incidence of bladder injury, with slightly shorter postoperative length of hospitalization and lower costs. In contrast, Venkatramani and colleagues found that bipolar transurethral resection was not superior to monopolar with regard to obturator reflex, bladder perforation, or hemostasis. However, other authors have reached the opposite conclusion.
Don’t Miss: Do You Need Antibiotics For Bladder Infection
How The Surgery Is Done
A thin hollow tube with a light and camera, known as a cystoscope, is passed through the urethra and into the bladder. The surgeon may use a wire loop on the cystoscope to remove the tumour through the urethra. Other methods for destroying the cancer cells include burning the base of the tumour with the cystoscope or a high-energy laser.
If the cancer has reached the lamina propria or is high grade, you may need a second TURBT 26 weeks after the first procedure to make sure that all cancer cells have been removed. If the cancer comes back after initial treatment, your surgeon may do another TURBT or might suggest removing the bladder in an operation known as a cystectomy.
How Does A Turbt Work
When the TURBT procedure is used to treat non-muscle invasive bladder cancer tumors, the urologist tries to completely remove the tumor and destroy any cancer cells in the bladder. The urologist may also use high-energy electricity or a high-energy laser beam to destroy the base of the tumor and try to eliminate any cancer cells that may remain in the area.
Sometimes urologists will recommend administration of a chemotherapy drug injected directly into the bladder to help kill any remaining cancer cells and try to reduce the likelihood that cancer cells will grow again. This is called intravesical chemotherapy treatment. Some patients may need another TURBT procedure a few weeks or months later as part of their treatment.
Don’t Miss: How To Empty Your Bladder With A Uti
Tumor At The Lateral Wall
In addition to the anesthetic options discussed above, there are several techniques the surgeon can employ to lessen the likelihood of a complication stemming from the inadvertent stimulation of the obturator nerve during resection of a laterally located tumor. Preventing overdistention, decreasing the cutting/coagulation current settings, and the use of intermittent cautery can lessen the incidence of adductor contraction. The endoscopic injection of local anesthetic into the tumor base can also deliver an obturator nerve block if a percutaneous attempt was not made preoperatively. Lastly, use of a bipolar resecting system restricts the flow of current to between the two electrodes of the resecting loop thus decreasing stimulation of the obturator nerve.
What Is The Cpt Code For Transurethral Resection Of Bladder Tumor
4/5code
Correspondingly, what is the CPT code for bladder biopsy?
Per the AMA’s Current Procedural Terminology , there are three options for coding urinary bladder specimens: 88305, 88307 and 88309. These codes should be applied as follows: 88305 Urinary bladder biopsy. This code applies regardless of the surgical approach.
Likewise, what is the CPT code for ureteral stent placement? 52332
Keeping this in view, what is Turbt stands for?
A procedure called transurethral resection of a bladder tumor is frequently used to help diagnose bladder cancer, as well as being a common part of bladder cancer treatment.
What is cystoscopy Fulguration?
fulguration A procedure that uses heat from an electric current to destroy abnormal tissue, such as a tumor or other lesion. It may also be used to control bleeding during surgery or after an injury. The electric current passes through an electrode that is placed on or near the tissue.
Also Check: Homemade Cat Food For Bladder Stones
A Single Immediate Postoperative Intravesical Instillation Of Chemotherapy
All participants will undergo IPIC unless bladder perforation occurs or is suspected during TUR. Within 24h postoperatively, one intravesical instillation of 60mg of epirubicin in 30ml of saline will be administered. The catheter will be clamped and left for 1h, and subsequently unclamped. The patients who do not undergo IPIC will be excluded from the analysis of primary endpoint, but included in the analysis of secondary endpoints.
Preoperative Considerations History And Physical
As with any operation, the treatment begins in the outpatient setting. At this time, a full history is obtained, and a focused urological physical examination is performed. The history should include the patients age, sex, past medical history, smoking history, history of bladder cancer or other malignancies, previous surgical history including endoscopic treatment and any intravesical therapy following the diagnosis of bladder cancer . A review of the patients imaging studies is important to determine the status of the upper urinary tract.
On the day of the operation, the history and physical exam should be reviewed. The case should be discussed with the anesthesiologist. The type of anesthesia is important. The patient should be fully relaxed so that the bladder can be filled to the desired amount . General anesthesia with complete neuromuscular blockade is often preferred, as it allows the patient to be paralyzed as needed intraoperatively and to recover quickly postoperatively. Spinal anesthesia is also a reasonable option as it ensures the patient will not move during the procedure and maximizes bladder relaxation. Although we have never used this technique, transvesical injection of the obturator nerve has been reported to be an effective method to block the adductor or obturator reflex. Lastly, in addition to the routine preoperative lab values, the team should review any history of anticoagulant therapy, which is common in elderly patients.
Don’t Miss: How To Fix Bladder Issues
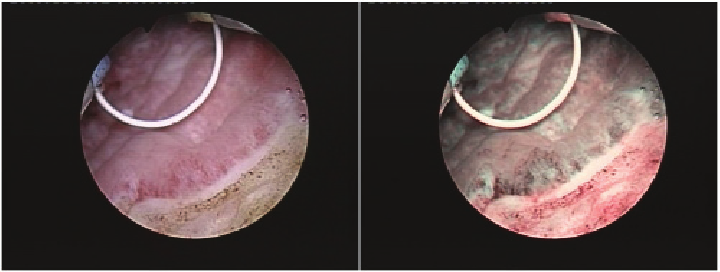
Surgical Procedure And Device For Pdd
Approximately 3h before surgery, patients orally received a water-dissolved 5-ALA solution at a dose of 20mg/kg . The PDD-EBTUR will be performed by a single surgeon with substantial experience in this surgical technique , while the PDD-cTURBT will be performed by one of the following experienced urologists: M. Miyake, S. Hori, Y. Nakai, S. Anai, K. Torimoto, N. Tanaka, and K.Fujimoto. The surgical procedures and devices for PDD-EBTUR and PDD-cTURBT are described in our previous report .
How You Have It
The surgeon puts a thin rigid tube called a cystoscope into your urethra.
The cystoscope has optic fibres inside it, a light, camera and eyepiece at one end. The surgeon can look through the eyepiece or see images on a TV screen.
The surgeon passes small instruments down the cystoscope to cut any tumours out of your bladder lining.
Recommended Reading: Can Clindamycin Treat Bladder Infection
Are There Any Risks Associated With Cystoscopy
Cystoscopy is usually a safe procedure and serious complications are uncommon. The most frequent complication is urinary tract infection . UTIs may require antibiotic treatment, so it is important to seek medical help if urinary symptoms persist for longer than expected following a cystoscopy or if other UTI symptoms develop . Less commonly, patients may be temporarily unable to pass urine after a cystoscopy and it may be necessary for a catheter to be inserted into the bladder to enable emptying. There is also a small risk that the urethra or bladder may be damaged by the cystoscope and subsequently require remedial surgery.
In patients who undergo rigid cystoscopy, side effects associated with anesthesia may be experienced. Common side effects of general anesthesia include nausea, vomiting, sore throat, muscle aches, itching, shivering, and sleepiness side effects most frequently associated with spinal anesthesia include itchiness, a drop in blood pressure, and temporary difficulty passing urine .
Trans Urethral Removal Of Bladder Tumour
A trans urethral resection of bladder tumour is usually the first treatment you have for early bladder cancer.
Your surgeon removes the tumour in your bladder through the urethra. The urethra is the tube that carries urine from the bladder to the outside of your body.
You might have TURBT to remove early bladder cancer:
- during a cystoscopy test if your specialist sees a tumour
- after having tests that have shown a bladder tumour
You usually have it under general anaesthetic, which means you are asleep. In some hospitals, you may have a spinal anaesthetic instead of a general anaesthetic. This is an injection into your spine so you cant feel anything from below your waist.
This treatment takes between 15 to 90 minutes.
Don’t Miss: What Doctor To See For Bladder Infection
What Is A Cystoscopy
A cystoscope is a thin tube with a light and camera attached to the end. During a cystoscopy, the cystoscope is passed through the urethra into the bladder. The two main types of cystoscopy are termed flexible and rigid:
- Flexible cystoscopy uses a flexible cystoscope tube that is able to bend easily as it passes through the urethra. This procedure can be carried out under local anesthetic while the patient is awake and is commonly used for simple visual examination of the inside of the bladder, although the collection of bladder washings or small tissue samples may be undertaken.
- Rigid cystoscopy uses a hard, straight cystoscope. For this type of cystoscopy, patients are usually under general anesthesia in some patients, spinal anesthesia that numbs the lower half of the body may be used instead. Rigid cystoscopy is performed when tissue samples and/or removal of small bladder tumors are required. Long, small-diameter instruments can be passed down the cystoscope to take biopsies from the bladder lining, and a tool called a resectoscope that has a cutting wire loop at the end may be used to remove abnormal tissue or small tumors. This procedure is referred to as transurethral resection of a bladder tumor or TURBT.
Diagram of a cystoscopy for a man
Diagram of a cystoscopy for a woman
Damage To The Bladder
There is a small risk of a hole being made in the bladder during surgery. If this happens, the catheter is left in the bladder to allow the hole to heal. The catheter will be removed when the hole has healed. Rarely, you may have an operation to close the hole.
The nurse or doctor may ask you for a sample of your urine to check for any infection. If you have a urine infection, your doctor will give you antibiotics to treat it before surgery.
You will see a member of the surgical team and a specialist nurse who will talk to you about the operation. This is a good time to ask any questions, or to talk about any worries you may have.
You usually go into hospital on the day of your operation. You usually have a general anaesthetic. But you may have the operation done under a spinal anaesthetic. For a spinal anaesthetic, the doctor injects a drug through a needle into your back. This numbs the nerves from the waist down. You will be awake during the operation, but you will not feel anything. If you are having a spinal anaesthetic, you may also have another drug to help you relax.
You will see the doctor who gives you the anaesthetic either at a pre-assessment clinic, or when you are admitted to hospital.
The nurse will talk to you about what you should do before the operation. This can include instructions about medications or eating and drinking.
Most people are given chemotherapy into the bladder straight after surgery.
Read Also: Can Lower Back Pain Cause Bladder Problems
Sexual Effects Of Urostomy
Its normal for both men and women to be concerned about having a sex life with a urostomy. Having your ostomy pouch fit correctly and emptying it before sex reduces the chances of a major leak. A pouch cover or small ostomy pouch can be worn with a sash to keep the pouch out of the way. Wearing a snug fitting shirt may be more comfortable. Choose sexual positions that keep your partners weight from rubbing against the pouch. For more tips, see Urostomy Guide.
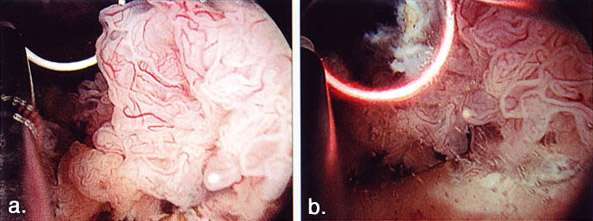
Tumours At The Ureteral Orifices
Coagulation close to the ureteral orifices should be avoided as it may cause scarring and lead to ureteric obstruction . However, tumours that involve the ureteral orifices can be resected judiciously under pure cutting settings. This would be particularly beneficial as satisfactory renal function can be facilitated if cisplatin-based neoadjuvant chemotherapy is considered for MIBC. Although it may result in vesicoureteric reflux and would be uncommon to cause stricture, a temporary ureteric stent placement between 2 and 6 weeks can further reduce the risk. A form of imaging such as renal ultrasound, CT urogram or Diethylenetriamine Pentaacetic Acid renal scan after resection is recommended.
Also Check: Bcg Tx For Bladder Cancer
Tumor Involving The Ureteral Orifice
A tumor near or involving the ureteral orifice poses the challenge of obtaining complete resection and adequate hemostasis while preserving the caliber of the intramural ureter. Resecting with a purely cutting current and the judicious use of pinpoint cautery at the lowest effective setting for hemostasis make ureteral stricture unlikely. If postoperative flank pain develops, a renal ultrasound can be performed to evaluate for hydroureteronephrosis. If present, a percutaneous nephrostomy tube can be placed. Tumor location at the ureteral orifice should not deter appropriate endoscopic management.
Reflux of urine into the upper tracts, which may occur with ureteral stenting or via vesicoureteral reflux following resection of the ureteral orifice, has been shown to increase the risk of seeding and tumor occurrence in the ureter and renal pelvis in some retrospective studies. Conversely, Solsona and colleagues found no significant difference in upper tract recurrence patterns when refluxing and nonrefluxing patients were studied post-TURBT. Regardless, close follow-up and monitoring for bladder as well as upper tract recurrence are advisable. Patients who symptomatically reflux after TURBT have been successfully managed with the endoscopic injection of bulking agents. Surgical reimplantation of the refluxing ureter is also possible.
Tumours On The Lateral And Anterior Walls
Resection of lateral wall tumours may result in stimulation of ONR resulting in increased risk of perforation . Strategies that have been shown to reduce the likelihood of ONR would include avoidance of bladder overfilling, reduced cutting current, use of short intermittent burst current , use of bipolar electrocautery, and use of neuromuscular blockade .
Tumours on the anterior wall could be challenging to resect and may require suprapubic depression by an assistant as well as proper resectoscope angles. More effective resection might be achieved by using open-angled loops.
You May Like: Can A Bladder Infection Heal Itself
Factors That Would Affect Recurrence And Progression
Bladder cancer is associated with a high rate of recurrence among patients with NMIBC. A number of studies assessed the factors that might be associated with recurrence and progression of bladder cancer following TURBT. The majority of the studies were rated as low quality and no strong recommendations were made in the guidelines due to study heterogeneity and hence low grade evidence. Nevertheless, there were a number of factors that have been shown to significantly influence the outcomes.
The largest randomised controlled trial included 2,596 patients in seven European Organization for Research and Treatment of Cancer trials. It demonstrated recurrence rates ranging from 15% to 61% and progression rates of less than 1% to 17% at one year. At five years, the probabilities of recurrence and progression ranged from 31% to 78% and from less than 1% to 45%, respectively. The risk of recurrence was linked to a number of clinicopathologic factors including size, multifocality, prior recurrence, stage, CIS and grade . Based on these key factors the European Organization for Research and Treatment of Cancer scoring system and risk tables for recurrence and progression in patients with NMIBC have been developed as shown in .
Restaging Transurethral Resection Of Bladder Tumors
American Urological Association guidelines and European Association of Urology guidelines recommend repeat resection for all patients with lamina propria invasion without muscularis propria present in the specimen. In addition, EAU guidelines recommend restaging in all T1 tumors as well as all high-grade Ta tumors. According to AUA guidelines, repeat resection is considered for patients with high-grade Ta bladder cancer and T1 tumors with muscularis propria in the specimen.
Restaging TURBT is typically performed 68 weeks following initial resection. Richstetter and colleagues found that residual tumor was found in 38% of restaging TURBT specimens. The risks of restaging TURBT are similar to the risks of initial TURBT and include anesthetic risk, bleeding, perforation, potential delay of definitive therapy, and increased difficulty with future therapies such as cystectomy.
You May Like: What’s Good For Bladder Control
Key Steps And Principles Of Turbt
After induction of anaesthesia patient is placed in the dorsal lithotomy position. The procedure can be performed either under spinal or general anaesthetics. General anaesthetics would be preferred if neuromuscular blockade is indicated to prevent stimulation of obturator nerve reflex during the resection of lateral wall tumours. Bimanual examination of the bladder under anaesthesia is performed before resection. The prostate should also be assessed for men. The TURBT is undertaken after a detailed pancystoscopic evaluation using both 30- and 70-degree lenses for optimal assessment of the urethra, prostate and bladder including the bladder neck. Alternatively, a retroflexion manoeuvre using a flexible cystoscope can also be utilized. The anterior wall and the dome of the bladder might require suprapubic pressure for better visualisation.