What Did This Study Do
The SAVE U RCT involved 208 women who needed surgery for uterine prolapse, where the uterus had descended nearly to the opening of the vagina or below . The trial took place in the Netherlands from 2009 to 2012.
The women were randomised to undergo sacrospinous hysteropexy or vaginal hysterectomy with uterosacral ligament suspension . Women were excluded if they had previous pelvic floor surgery, or other pelvic symptoms. Surgeons were given a detailed guideline on the surgeries to ensure a uniform technique, although there was some variation in the type of stitches used.
For this follow-up study, 204 women were assessed five years after surgery.
There was some risk of bias because the trial could not be blinded.
How Common Is A Prolapse After A Hysterectomy
4 Min Read
The uterus is one of the most important support structures in the pelvic floor. It provides support for the vagina and can help prevent conditions like vaginal prolapse or bladder prolapse. A hysterectomy removes the uterus, thus, removing additional vaginal support. In 2008 and 2014, two studies were conducted to determine whether or not the risk of prolapse developing increased once the uterus was removed. Both studies concluded that the possibility of developing vaginal prolapse 1 to 2 years post surgery is greater than not having the procedure done at all.
The most common form of vaginal prolapse associated with a hysterectomy is called enterocele the small intestine herniating down toward the vagina. However, depending on the type of hysterectomy and your recovery, there is a risk of developing various types of vaginal prolapse.
Degree Of Bother By Symptoms Is A Key Factor
In older patients, whether and how to treat POP depends on their functional status, the degree to which they are bothered or inconvenienced by the condition, and their personal preference.
If an elderly woman has anatomic POP but lacks bothersome symptoms, the condition rarely requires treatment. Conversely, POP symptoms may cause depression and poor self-image and impair participation in social activities. Associated bladder, bowel or sexual symptoms can also take their toll. And quality of life may be impacted regardless of the stage of prolapse. Vaginal bulge causing discomfort and/or bleeding, difficulty voiding and/or defecating, recurrent urinary tract infections and POP-associated low back pain are all symptoms that may warrant treatment.
Recommended Reading: How To Cope With Overactive Bladder
When Should Someone Seek Medical Care For A Prolapsed Bladder
Any woman who notices symptoms of a prolapsed bladder should contact her doctor.
A prolapsed bladder is commonly associated with prolapses of other organs within a woman’s pelvis. Thus, timely medical care is recommended to evaluate for and to prevent problematic symptoms and complications caused by weakening tissue and muscle in the vagina. Prolapsed organs cannot heal themselves, and may worsen over time.
Several treatments are available to correct a prolapsed bladder.
Visit A Pelvic Floor Physical Therapist
If you are experiencing urinary incontinence, there is a good chance that your pelvic floor muscles may not function properly.
A pelvic floor physical therapist can help you restore function to these muscles, which may help improve your urinary control.
Some benefits of working with a physical therapist include:
- Learning exercises to helpstrengthen your pelvic floor muscles on your own
- Practicing the relaxation of your pelvic floor muscles to maintain bladder control and
- Dealing with stress and anxiety that may contribute to urinary leakage
Rehabilitation of the pelvic floor muscles has been shown to decrease the risk of future urinary tract infections, which is another benefit of visiting a physical therapist.
Also Check: Overactive Bladder After Turp Surgery
What Is A Vaginal Mesh Suspension
In some women, the supporting ligaments of the vagina are so weakened or torn that they are beyond repair. For these women, an artificial material can be used to take the place of the weakened ligaments. There are a number of types of materials used to perform this operation, but the most common is a thin, plastic, non-reactive mesh. This mesh is flexible, much like cloth, and can be cut and tailored to fit each womans anatomy. The mesh is first sutured onto the top of the vagina as it sits inside the body. The vagina is pulled up to its normal position, and the other end of the mesh is sutured to the connective tissue around the sacral bone to hold the vagina in place. The mesh is very strong, and the operation has a high success rate. However, in rare cases, the body can have a reaction to the mesh since it is foreign material. For that reason, the procedure is reserved for women who have had a previous failed vaginal prolapse surgery and need repeat surgery.
This mesh operation is called a sacral colpopexy and is most often performed through an abdominal incision. However, recent innovations now allow this procedure to be performed laparoscopically by experienced laparoscopic surgeons. In some centers the addition of the Da Vinci Robot has assited with laparoscopic support surgery. As with other laparoscopic procedures, the hospital stay is shorter and the recovery faster.
Also Check: Loss Of Bladder Control In Cancer Patients
Pros Of Bladder Suspension Surgery
1. Less Urine LeakageWhen the procedure is effective, urine leakage is not only reduced but almost nonexistent. This means that you can return to your normal activities and not have to be self-conscious when you are on-the-go. Urine leakage can impact your emotional and mental state negatively, but bladder suspension surgery can help you get your life back.
2. Treats All Types of Stress IncontinenceNo matter what your cause of stress incontinence is, this can be an effective surgical procedure. Those people dealing with urine leakage caused by menopause, child birth, surgery or muscle problems are great candidates for this type of surgery. It is almost 90% effective, which makes it the superior treatment option to Kegal exercises or medication.
Also Check: Can Stress Cause Overactive Bladder
Also Check: Best Antibiotic To Treat Bladder Infection
Uterine Prolapse & Hysterectomy Surgery
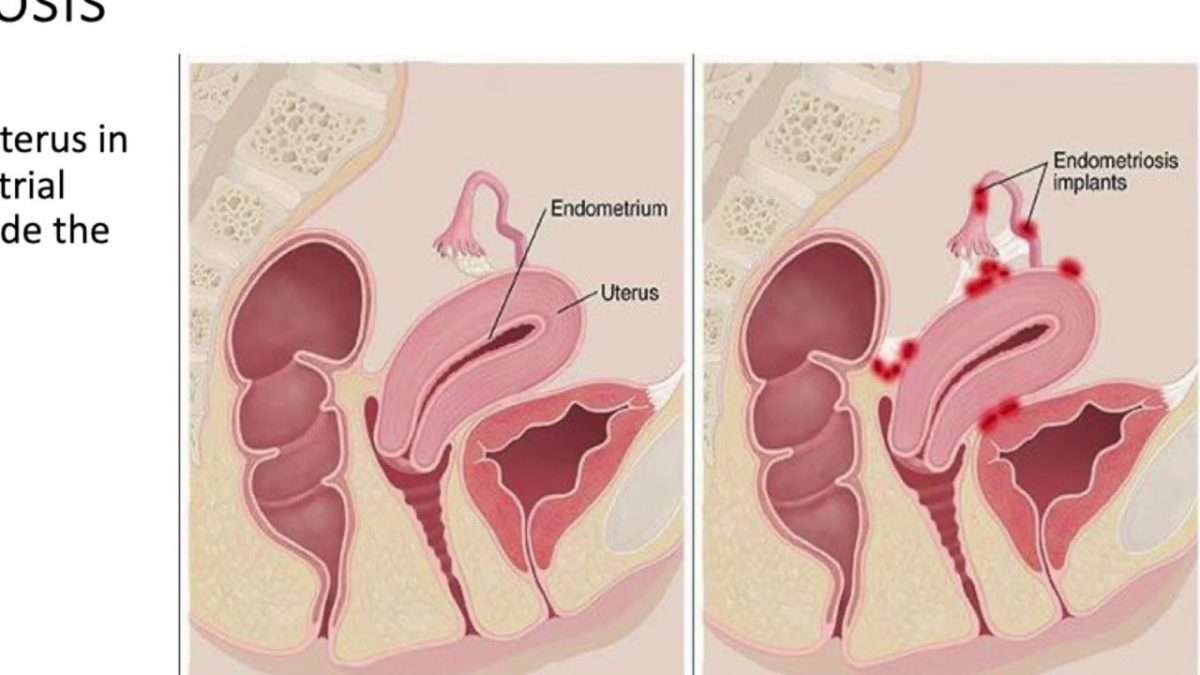
Uterine prolapse is a condition that occurs when the uterus slips down into, or protrudes out of, the vaginal canal. Normally, the uterus is supported by a network of muscles and ligaments. When the pelvic floor muscles and ligaments stretch and weaken, they provide inadequate support for the uterus, causing the uterus to prolapse from its normal position. Uterine prolapse affects women of all ages, but most commonly affects postmenopausal women who have had vaginal deliveries during childbirth. Depending on the severity of the prolapse, treatment may or may not be necessary. For cases in which uterine prolapse does impact daily life, effective treatments are available. Uterine prolapse is estimated to account for approximately 200,000 prolapse surgeries each year in the United States.
Causes Uterine prolapse is a condition that has a number of causes and risk factors. Most often, pregnancy and trauma during childbirth, especially with larger newborns and difficult labor or delivery, cause muscle weakness and stretching of the supporting tissues and ligaments of the uterus. The effects of aging, including decreased muscle tone and reduced amounts of estrogen, are also believed to contribute to uterine prolapse. Other risk factors for uterine prolapse include tumors in the pelvic cavity, collagen quality, smoking, and obesity.
Before Choosing Surgeryexpand All
There is no guarantee that any treatmentincluding surgerywill relieve all of your symptoms. Also, new problems may occur after surgery, such as pain during sexual intercourse, pelvic pain, or urinary incontinence.
More than one type of surgery may be done at the same time to fix multiple problems.
Surgery done through the vagina may take less time to perform than surgery done through an incision in the abdomen. The recovery time is usually shorter.
Surgery done with an abdominal incision may result in less pain during sex than after procedures done through the vagina. But with an abdominal incision, there is a risk of damage to the intestines and a risk of complications from adhesions.
After surgery with mesh placed in the abdomen, there is a small risk that the mesh will erode into the vagina. Mesh erosion can cause scarring and pain that can be long-lasting. Additional surgery may be needed to remove the mesh.
If you are considering a surgery using vaginally placed mesh, ask your health care professional for detailed information about its risks, benefits, and potential complications. POP can be treated successfully without mesh in many cases.
When considering surgery for POP, it is important to weigh your options. Talk with your health care professional about which option is best for your situation.
Article continues below
Don’t Miss: What’s Good For Weak Bladder
Is There A Possibility Of Recurrence After Surgery
The results of a study carried out by then Radcliff John Hospital in Oxford show that 10.8 % of women undergoing pelvic organ prolapse surgery have a second or third operation within the next 11 years. The study followed a group of 2099 women that had surgery for POP between 1995 and 2005. Worth mentioning is that of the women that needed repeat surgery, 61,5% needed surgery in a different area than the site of the original operation.
What Is Pelvic Organ Prolapse Surgery
Perhaps youve had a pelvic organ prolapse, and non-surgical treatments arent helping? Or maybe your prolapse is more severe? If so, your surgeon may recommend, pelvic organ prolapse surgery.
This surgery involves lifting the pelvic organs, such as the bladder, bowel and uterus, and stitching the tissues around them to give you more support.
Also Check: Does Beer Help Bladder Infections
Don’t Miss: Gemcitabine Treatment For Bladder Cancer
What Other Therapies Treat A Prolapsed Bladder
Physical therapy such as electrical stimulation and biofeedback may be used to help identify and strengthen the muscles in the pelvis, particularly in those individuals who fail to respond to pelvic floor muscle exercises on their own.
- Electrical stimulation: A doctor can apply a probe to targeted muscles within the vagina or on the pelvic floor. The probe is attached to a device that measures and delivers small electrical currents that contract the muscles. These contractions help strengthen the muscles. A less intrusive type of electrical stimulation is available that magnetically stimulates the pudendal nerve from outside the body. This activates the muscles of the pelvic floor and may help treat incontinence.
- Biofeedback: A sensor is used to monitor muscle activity in the vagina and on the pelvic floor. The doctor can recommend exercises that can strengthen these muscles. These exercises may help strengthen the muscles to reverse or relieve some symptoms related to a prolapsed bladder. The sensor can monitor the muscular contractions during the exercises, and the doctor may be able to determine if the targeted muscles would benefit from the exercises.
How To Deal With Changes After A Hysterectomy
A hysterectomy that also involves the removal of ovaries results in the permanent cessation of a womans menstrual cycle. This condition is known as surgical menopause or surgery-induced menopause. Hormonal changes also take place during menopause for which the doctor may recommendhormone replacement therapy .
Menopause results in a decrease in the estrogen hormone that gives rise to signs and symptoms of menopause. HRT aims at making up for the loss of estrogen by replacing it with synthetic estrogen.
If you experience vaginal dryness and pain during sex, you can use a vaginal lubricant just before performing the carnal act.
You may feel depressed or stressed due to the loss of one or more of your reproductive organs. You can relax and destress yourself by indulging in massage therapy, deep breathing, meditation, and yoga.
You May Like: Bladder Cancer In Elderly Woman
How Effective Is Surgery For Uterine Prolapse
After sacrocolpopexy or sacrohysteropexy to correct uterine prolapse, about 90 out of 100 women no longer have problems such as urine leakage and pain during sex at least for some time.
But there is a risk of the womb dropping down again : In about 23 out of 100 women, it either drops down again or bulges out of the vagina within two years of the procedure.
Sacrocolpopexy and sacrohysteropexy surgery is performed through the abdominal wall, and a synthetic mesh is always used. Various other procedures are performed through the vagina for instance, sacrospinous fixation. In these procedures it is probably possible to operate without using synthetic mesh because compared to operations using the womans own tissue the use of mesh isnt more likely to prevent a prolapse recurrence. But recurrences are more likely after surgery that is performed through the vagina than after sacrocolpopexy and sacrohysteropexy.
All About Prolapse Surgery: Pros & Cons
briavergeldedios
People fear what they dont understand. For instance, consider perimenopause.
Its easy to panic when your period goes erratic along with unusual symptoms. You might even think that its a result of some health condition. But instead its really perimenopause or at least this is a strong possibility and something that often gets overlooked.
After all, perimenopause remains a mystery to the masses. Yet, theres a Worlds Perimenopause Day on October 11. Youre not alone if this is your first time hearing of this!
And this is exactly what this blog is for! We will unveil the truth about the not-so-mysterious perimenopause bleeding and your most pressing question how long is too long, for a period during perimenopause?
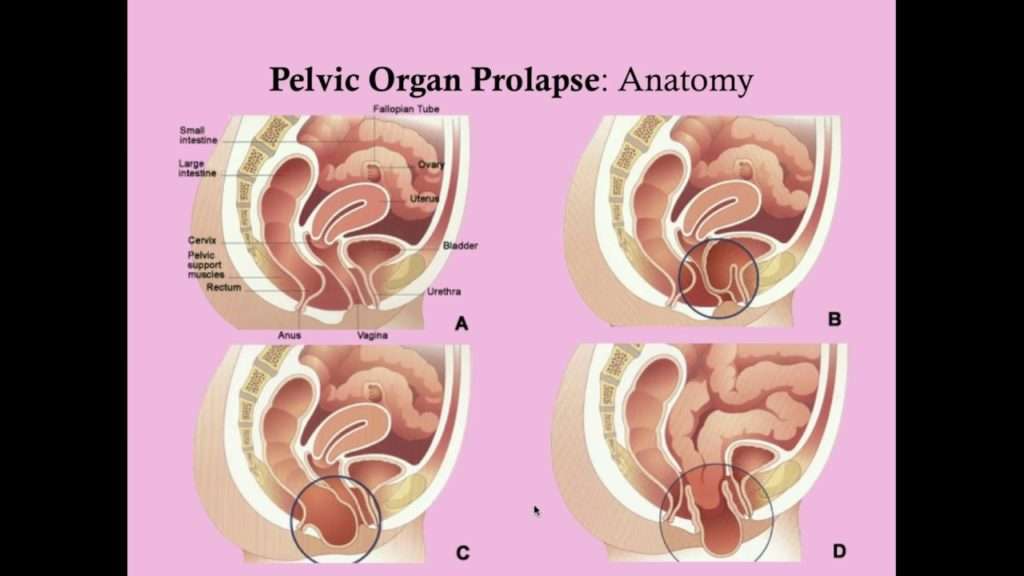
Types of Pelvic Organ Prolapse
Prolapse happens when one or more pelvic organs descend from their normal positions, causing a bulge and discomfort from the vagina or anus.
There are four types of prolapse based on the area where the condition occurs:
1. Cystocele / Urethrocele
When the protrusion affects the front part of the vagina and bladder, the condition is called a Cystocele or Urethrocele. Cystocele – the bladder drops into the vagina often resulting in urinary incontinence. Urethrocele – the urethra protrudes into your vagina. Cystourethrocele – both the bladder prolapse and urethra prolapse are present.
2. Rectocele
When the back part of the vagina and rectum are involved, it is called Rectocele.
3. Enterocele
4. Uterine
You May Like: Does Azo Help Bladder Spasms
What You Can Do For Vaginal Prolapse
They make devices called pessaries, which one can insert into the vagina and serve to keep the pelvic structures in their proper position. Avoiding strenuous lifting can help prevent and treat prolapse.
You can also do pelvic floor exercises, called Kegel exercises. These are simple exercises your doctor can teach you that will strengthen the pelvic floor muscles so that the supporting muscles will better hold up the pelvic structures. It can take several months of daily Kegel exercises to see an effect on urinary incontinence.
I can recommend The Bathroom Key , a book that presents an 8 to 12-week program with specific exercises to strengthen the pelvic floor muscles and that will help you to regain bladder control. It provides step by step instructions on how you can cure urinary incontinence without resorting to medication or surgery
If the prolapse after hysterectomy is severe, often surgery is the only real option, depending on how much the tissues affect you. With surgery, they aim to reconstruct the pelvic floor and to bring back the pelvic organs in their original position.
Recommended Reading: How Can I Treat A Bladder Infection At Home
Surgical Technique To Support The Vagina
The top of the vagina is known as the vaginal apex. The tissues that help hold up the vaginal apex are removed during a hysterectomy.
If the top of the vagina is not suspended or stitched to surrounding structures once the uterus is removed, the risk of future prolapse may be increased.
The process of stitching the top of the vagina to supporting tissues to prevent a prolapse is known as prophylactic apical suspension of the vagina. During your preoperative appointment you may wish to discuss the measures your surgeon intends to perform in order to suspend your vagina and reduce your risk of future prolapse.
You May Like: Ways To Cure Bladder Infections At Home
Who Gets Uterine Prolapse
Uterine prolapse is most likely to happen in women who:
- Have had one or more vaginal deliveries.
- Are post-menopausal.
- Have family members who have had prolapse.
Menopause occurs when your ovaries stop producing the hormones that regulate your monthly menstrual cycle . When you havent had a period for 12 straight months, you are considered menopausal. One of the hormones that stops during menopause is estrogen. This particular hormone helps keep your pelvic muscles strong. Without it, you are at a higher risk of developing a prolapse.
Donât Miss: Ways To Help Overactive Bladder
Women Who Still Have The Uterus
A few options are available and the main decisions to be made are whether to remove or preserve the uterus and whether to use a synthetic graft or not.
If a hysterectomy is indicated, some of the possible operations are:
Laparoscopic hysterectomy + uterosacral ligament suspension
This procedure does not use synthetic grafts . Once the uterus is removed with a standard laparoscopic hysterectomy, the top of the vagina is sutured to the uterosacral ligaments to provide support and keep it in position.
Laparoscopic hysterectomy + Sacrocolpopexy
This operation is similar to the sacro-colpopexy. The hysterectomy can be total, where the cervix is removed and the mesh is sutured to the top of the vagina and to the ligaments over the sacral promontory, or subtotal where the body of the uterus is removed and the cervix is preserved and used to place the vaginal portion of the mesh.
If the uterus is preserved, the main option is a Sacro-hysteropexy.
The mesh is passed and sutured around the lower portion of the uterus and then sutured to the sacral promontory in the same manner as with the sacro-colpopexy.
Also Check: Natural Ways To Help A Bladder Infection
What Types Of Surgery Are Available To Treat Pelvic Organ Prolapse
There are many different options available to treat pelvic organ prolapse. The best way to treat one womans prolapse is not necessarily the best way to fix another womans prolapse.
The many options available for treatment of prolapse mean that there is not a right or wrong choice for each woman. The decisions are often complex because the prolapse can involve many compartments or sections of the vagina and cause many symptoms.
Some of the surgical approaches to treating vaginal prolapse include :
- Vaginal surgery such as:
- Anterior repair which corrects a cystocele
- Posterior repair- which corrects a rectocele
- Vaginal suspension surgery which corrects prolapse of the uterus or top of the vagina after hysterectomy including:
- Sacrospinous suspension
- Manchester repair
More specific and detailed information regarding the different types of prolapse surgery will be provided by Dr McKertich on an individual basis after a full assessment.