Clinicalapplication Of Histological Grading Systems
- Two classification systems the WHO 1973 and the WHO 2004/2016, are currently availablefor routine clinical application.
- The most important parameters, which must be considered for clinical application of anygrading system are its interobserver reproducibility and prognostic value .
- To facilitate the clinical utilisation in daily practice, these guidelines providerecommendations for tumours classified based on both classification systems.
Table 4.2: WHO classification in 1973 and in 2004/2016
|
1973 WHO classification system |
|
2004/2016 WHO classification system |
|
Papillary urothelial neoplasm of low malignantpotential Low-grade papillary urothelial carcinoma High-grade papillary urothelial carcinoma |
Figure 4.1: Stratification of tumoursaccording to grade in the WHO 1973 and 2004/2016 classifications *
|
*1973 WHO Grade 1 carcinomas have beenreassigned to papillary urothelial neoplasm of low malignant potential and low-grade carcinomas in the 2004 WHO classification, and Grade 2carcinomas to LG and high-grade carcinomas. All 1973 WHO Grade 3 carcinomashave been reassigned to HG carcinomas . PUNLMP is a non-invasive neoplasm and thereforeconsidered stage pTa in the AJCC/UICC staging systems. |
Table 4.3: WHO 2004 histological classification for flat lesions
|
Non-malignant lesions Urothelial CIS is always high grade. |
Bcg Dosing For Bladder Cancer: Standard Frequency Schedule Correct
Prof Oliver Grimm speaks to ecancer at the 2020 ASCO GU meeting at San Francisco about the results of the phase III NIMBUS trial looking at BCG dosing for bladder cancer.He explains that the aim was to show that a reduced dosing schedule would be non-inferior to the standard schedule, however the experimental arm was found to be inferior to the standard frequency arm.Prof Grimm states that we should therefore continue using the standard frequency as recommended but that they did make some interesting findings concerning recurrence in the standard frequency arm which can be attributed to the routine use of repeated TUR prior to BCG induction.
- Categories:
Summary Of Evidence And Guidelines Fortransurethral Resection Of The Bladder Biopsies And Pathology Report
|
Summary of evidence |
|
|
Transurethral resection of the bladder tumour followed by pathology investigation of the obtained specimen is an essentialstep in the management of NMIBC. |
|
|
The absence of detrusor muscle in the specimen isassociated with a significantly higher risk of residual disease and tumourunder-staging . |
|
|
In patients with a history of small Ta LG/G1 tumours,fulguration of small papillary recurrences on an outpatient basis is feasibleand safe. |
|
|
A second TURB can detect residual tumours and tumourunder-staging, increase recurrence-free survival, improve outcomes after BCGtreatment and provide prognostic information. |
Also Check: Can Stress Cause Overactive Bladder
Further Improvement Of Bcg Immunotherapy
Epidemiologic and laboratory studies suggest that vitamin supplements may be helpful for the prevention of some cancers, but clinical trials have failed to demonstrate protection with naturally occurring vitamins. Without substantiation of the highly touted benefits of vitamins, few physicians caring for cancer patients have recommended their use.
To evaluate the potential benefit of high-dose vitamins, 65 patients with biopsy-confirmed, resected stage Ta or T1 transitional cell carcinoma were enrolled in a randomized comparison of intravesical BCG with or without percutaneous administration . These patients were also randomized by closed envelope to receive multiple vitamins in the recommended daily allowance versus RDA multivitamins plus 40,000 units of vitamin A, 100-mg vitamin B6, 2000-mg vitamin C, 400 units of vitamin E, and 90-mg zinc .
How Long Does It Last
The aim of maintenance therapy is to try to reduce the risk of bladder cancer recurrence as much as possible.2,3 The length of a patients maintenance therapy with BCG immunotherapy depends on multiple factors, such as the grade of the patients cancer, and the judgment of the healthcare providers on the cancer care team.
Read Also: Does Bladder Cancer Cause Back Pain
Is There A Risk Of Bladder Cancer After Bcg Treatment
Like most cancers, bladder cancer can potentially return after treatment. Statistically, cancer will recur in up to 40% of people who receive BCG treatment. Its important to note, however, that even if the cancer comes back, it may not progress.
Low-grade bladder cancer usually doesnt spread to other areas of your body. But people who have low-grade bladder cancer have a higher risk of developing other low-grade cancers throughout their lifetime.
Less often, aggressive bladder cancer can develop after BCG treatment. If this happens, cystectomy is usually recommended.
Is There Any Preparation Involved
Its important that you follow your doctors instructions for what to do before and after the procedure. Tell your doctor about all the medications you take. Certain immunosuppressants, antimicrobial therapies, and radiation therapies can interfere with BCG treatment.
Youll be advised to limit your fluid intake for four hours prior to the procedure. You might be told to avoid caffeine for a few hours longer than that, because its a diuretic and could make things more difficult.
Youll be asked to urinate just before the procedure so youll be able to hold the medication in your bladder for several hours.
Recommended Reading: Why Does Cranberry Juice Help Bladder Infections
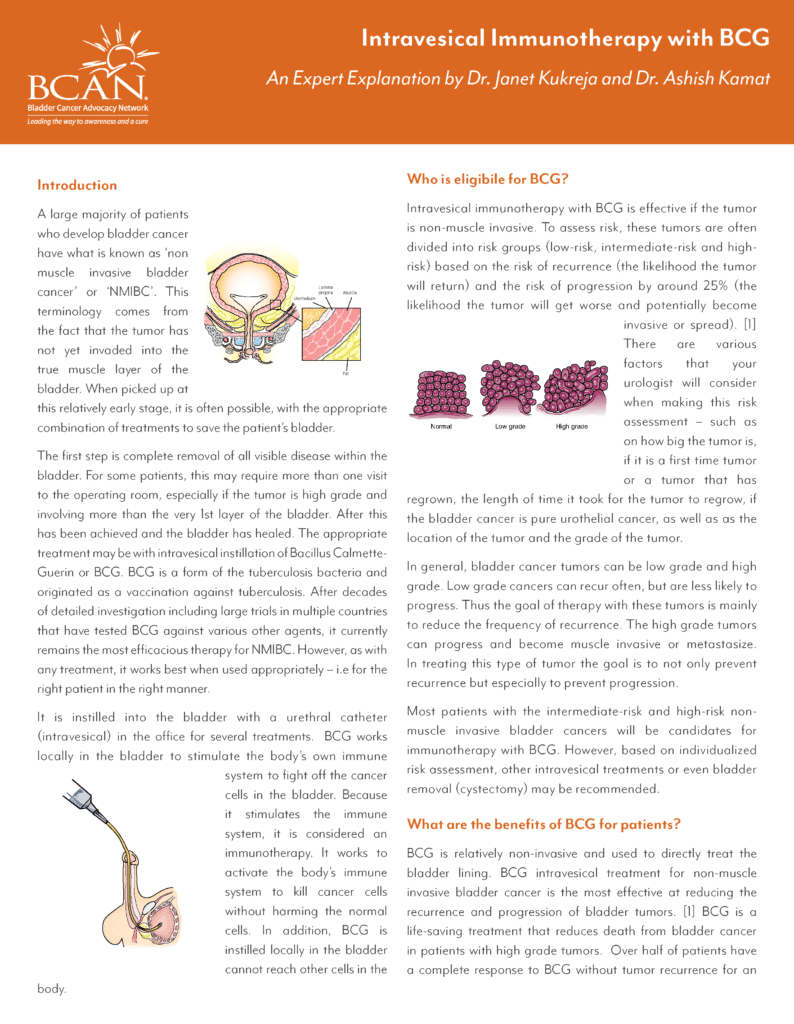
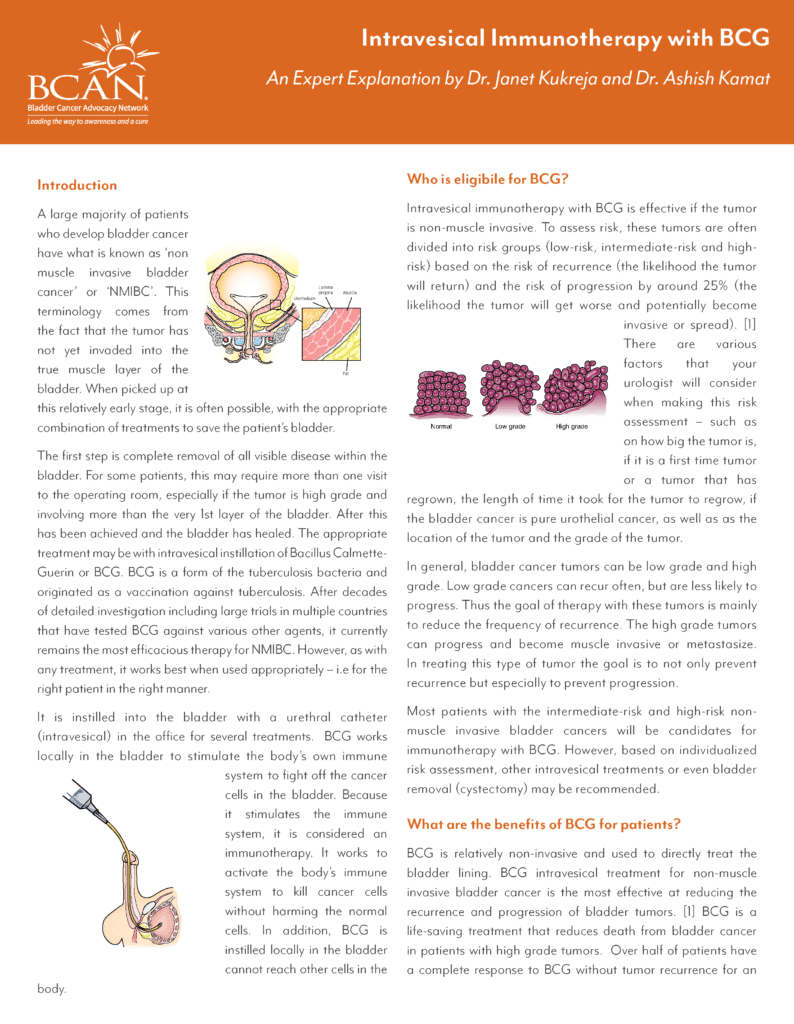
Stage Information For Bladder Cancer
The clinical staging of carcinoma of the bladder is determined by the depth of invasion of the bladder wall by the tumor. This determination requires a cystoscopic examination that includes a biopsy and examination under anesthesia to assess the following:
- Size and mobility of palpable masses.
- Degree of induration of the bladder wall.
- Presence of extravesical extension or invasion of adjacent organs.
Clinical staging, even when computed tomographic and/or magnetic resonance imaging scans and other imaging modalities are used, often underestimates the extent of tumor, particularly in cancers that are less differentiated and more deeply invasive. CT imaging is the standard staging modality. A clinical benefit from obtaining MRI or positron emission tomography scans instead of CT imaging has not been demonstrated.
How Is Bcg Given
The combination of BCG and TURBT is the most effective treatment for high-risk non-muscle-invasive bladder cancer. BCG is given once a week for six weeks, starting 24 weeks after TURBT surgery. It is put directly into the bladder through a catheter. You may be asked to change position every 15 minutes so the vaccine washes over the entire bladder. This is usually done as a day procedure in hospital, and each treatment session takes up to two hours.
Your treatment team will outline some safety measures to follow afterwards at home. This is because BCG is a vaccine that contains live bacteria, which can harm healthy people.
| Let your doctor know of any other medicines or complementary therapies you are using, as they may interfere with how well the bladder cancer responds to BCG. For example, the drug warfarin is known to interact with BCG. |
Read Also: Why Can I Control My Bladder Female
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
Guideline Statement 24
Discussion
Guideline Statement 25
Discussion
Guideline Statement 26
Different Strains Of Bcg
There are several different strains of BCG available. The more commonly used strains include the Tice strain produced by Organon Teknika, the RIVM strain produced by Bilthoven, and the Connaught strain produced by Connaught Laboratories. Morales used a strain of BCG which came from the Institut Armand Frappier in Montreal, in fact BCG-Connaught is derived from this strain.
As there are several commercially available strains of BCG, uncertainty exists in the literature about whether the various strains of BCG have identical immunotherapeutic efficacy and identical clinical effectiveness. Given this fact direct comparison between clinical studies is difficult when different strains of BCG have been used.
You May Like: Sjogren’s Syndrome And Bladder Problems
Box : Prognostic Factors For Recurrence
-
Number of tumours more tumours mean more frequent recurrences.
-
Previous recurrence rate* or a recurrence at three months.
-
Size of the tumour those > 3 cm carry a worse prognosis.
-
Grade of anaplasia.
-
Presence of CIS.
*The recurrence rate being the number of positive cystoscopies per year over the number of cystoscopies performed per year.
For progression, tumour grade is the most important factor. It is also known that T1 tumours have a worse prognosis than Ta tumours. Using these factors patients with superficial bladder cancer can be divided into three groups: the lowest risk group with a single less than 3 cm Ta G1 tumour, and a recurrence rate of less than one tumour per year a high risk tumour of T1 G3, multifocal, large, highly recurrent, and CIS and other tumours of intermediate risk. Recent studies further confirm these criteria.
What Happens During Treatment
A urinary catheter is inserted through your urethra and into your bladder. Then the BCG solution is injected into the catheter. The catheter is clamped off so the solution stays in your bladder. Some doctors may remove the catheter at this time.
You have to hold the medicine in your bladder. Youll be instructed to lie on your back and to roll from side to side to make sure the solution reaches your entire bladder.
After about two hours, the catheter is unclamped so the fluid can be drained. If the catheter was already removed, youll be asked to empty your bladder at this time.
Recommended Reading: Can Chewing Tobacco Cause Bladder Cancer
Optimal Schedule And Duration Of Therapy
The 6-week course of intravesical and percutaneous BCG, which was the first reported schedule, is very effective. Most subsequent studies have failed to demonstrate that alternative schedules provide significant benefits. Early modifications, such as omission of percutaneous vaccination, and quarterly or monthly maintenance, though accepted, only marginally improve convenience or efficacy. Although randomized clinical trials failed to demonstrate improved efficacy of percutaneous BCG against bladder cancer, systemic immune responses are higher after percutaneous vaccination than after intravesical administration alone. This heightened response after immunization is promising and should prompt new RCTs to investigate this application method.
RCTs of quarterly, monthly and repeated 6-week BCG instillations, which aim to maintain the immune response, also failed to show a significant improvement of efficacy . These results led some experts to question the value of maintenance BCG and to abandon its use. By contrast, the 3-week BCG regimen, designed by the Southwest Oncology Group with immunological principles in mind, is sufficiently different that it should not be considered in the same category as other maintenance BCG regimens.
Figure 1: Not all maintenance schedules are equal.
Individual Treatment Strategy In Primary Orrecurrent Tumours After Turb Without Previous Bcg Intravesical Immunotherapy
The type of further therapy after TURB should be based on the risk groupsshown in Section 6.3 and Table 6.1. The stratification and treatment recommendations arebased on the risk of disease progression. In particular in intermediate-risk tumours, the2006 EORTC scoring model may be used to determine a patientsindividual risk of disease recurrence as the basis to decide further treatment on.
Any decisions should reflect the following principles :
- Patients in the low-risk group have a negligible risk of disease progression. The singlepost-operative instillation of chemotherapy reduces the risk of recurrence and isconsidered as sufficient treatment in these patients.
- Patients in the intermediate-risk group have a low risk of disease progression . In these patientsone-year full-dose BCG treatment , or instillations of chemotherapy for amaximum of one year, is recommended. The final choice should reflect the individualpatients risk of recurrence and progression as well as the efficacy and sideeffects of each treatment modality.
- Patients in the high-risk group have a high risk of disease progression . In these patientsfull-dose intravesical BCG for one to three years , is indicated. The additional beneficial effectof the second and third years of maintenance should be weighed against its added costs,side-effects and problems connected with BCG shortage.
Figure 7.1: Treatment strategy in primary or recurrent tumourwithout previous BCG*
You May Like: Can Bladder Leakage Be Fixed
Box : Recommendations For Intravesical Bcg
RCTs and practice pattern research demonstrate that BCG immunotherapy in NMIBC reduces recurrences and progression, and affects mortality
3-week BCG maintenance is confirmed to reduce recurrence rates compared with induction alone, as well as metastasis and mortality compared with maintenance chemotherapy thus, it is the optimal regimen for current practice
BCG maintenance schedules other than the 3-week schedule show no significant benefit in RCTs
In the period of around 1.52 years after the identification of high-grade NMIBC, nonradical alternative treatments for patients experiencing BCG-failure can be explored
After the first BCG failure, patients have several treatment options, including repeated BCG , BCG plus interferon, single-agent intravesical chemotherapy , sequential chemotherapy or device-assisted chemotherapy
After the second BCG failure, or if the disease is BCG-refractory, radical cystectomy should be considered with alternatives considered a matter of investigation by clinical trials
Patients with BCG-refractory disease who are not candidates for cystectomy can be considered for chemoradiation
Abbreviations: NMIBC, non-muscle-invasive bladder cancer RCTs, randomized controlled trials.
The Use Of Intravesical Bcg In Urothelial Carcinoma Of The Bladder
Omar Alhunaidi1,2 and Alexandre R Zlotta1,3,4
1Department of Surgical Oncology, Division of Urology, University of Toronto and University Health Network, Toronto, ON M5G 1L7, Canada
2Department of Surgery, Division of Urology, Al-Amiri Hospital, Kuwait City, PO Box 4077, Safat 13041, Kuwait
3Department of Surgery , Mount Sinai Hospital, Toronto, ON M5G 1X5, Canada
4Lunenfeld-Tanenbaum Research Institute, Mount Sinai Hospital, Toronto, ON M5G 1X5, Canada
Correspondence to: Alexandre R Zlotta. Email:
Recommended Reading: Stage 2 Bladder Cancer Prognosis
Practical Issues Of Bcg Administration
Some practical points need to be considered when using BCG for bladder cancer treatment. BCG manufacturers recommend evaluating the tuberculosis status of the patient with a PPD tuberculosis skin test before initiation of therapy, with some practitioners obtaining chest radiographs in all patients. This procedure has never proven necessary, probably owing to the exceedingly low incidence of tuberculosis in developed nations, where most bladder cancer patients do not meet the criteria for disease screening as recommended by the Centers of Disease Control and Prevention. In fact, patients with a positive PPD test without active disease should not be excluded from BCG therapy, as the presence of a systemic immune response might help augment the antitumour response as noted above. In addition, patients with a positive PPD result were shown to display adverse effect profiles during BCG treatment that are similar to patients with a negative test.
How You Have It
BCG is a liquid. Your doctor or nurse puts the liquid into your bladder through a tube in the urethra . Usually, they then remove the catheter.
You must not pass urine for 2 hours. This gives the BCG time to be in contact with the lining of the bladder. Some hospitals may ask you to change position every now and again to make sure the drug reaches all parts of your bladder lining.
When you do pass urine, you need to be careful for 6 hours after the treatment because the vaccine contains bacteria. Men should sit down to pass urine to reduce the chance of splashing.
After you’ve been to the toilet, pour about half a pint of neat bleach into the toilet bowl and leave it for 15 minutes before flushing.
Wash your hands and genitals immediately with warm soapy water after you pass urine.
Read Also: How Do I Treat A Bladder Infection At Home
When Is Bcg Treatment Used
You may have BCG directly into your bladder after surgery to remove non-muscle-invasive bladder cancer. This type of surgery is called a transurethral resection of a bladder tumour .
This treatment helps prevent the cancer from coming back in the bladder lining. It also reduces the risk of the cancer becoming muscle-invasive. Doctors usually suggest this treatment if you have a high-risk bladder cancer, or sometimes if you have an intermediate-risk bladder cancer.
There is usually at least 2 weeks between the surgery to remove the cancer and the start of BCG treatment. This is to give your bladder enough time to heal from the surgery.
You usually have BCG treatment once a week for 6 weeks. This is sometimes called the induction course. You may be offered more BCG treatments. This is usually called maintenance treatment.
Treatment times vary. Your doctor will explain what is best for you.
Intravesical Bcg Dose And Schedule
To obtain the standard dose, the BCG vaccine powdered vial is usually diluted into 50 ml of normal saline. The diluted BCG is then infused into the bladder through a urethral catheter after complete drainage of the bladder. It should be maintained in the bladder for 2 hours. BCG is administered for 2 to 4 weeks after resection to prevent the risk of systemic toxicity . The schedule of intravesical BCG treatment comprises an induction course and a maintenance course .
We have previously shown that in most patients, the maximal peripheral immune response is already observed after 4 weekly BCG instillations. However, patients not previously immunised against mycobacterial antigens may require 6 weekly instillations to achieve a maximum stimulation level . Following the induction course, several studies have reported that additional BCG treatment may decrease recurrence.
Two decades ago, Zlotta et al showed that intravesical BCG instillations induced a transient peripheral immune activation against BCG antigens. Reactivation was observed in most cases after additional BCG courses . This absence of long-lasting immune activation after a single 6-week course of BCG could be related to the increased clinical efficacy observed with BCG maintenance instillations. However, the optimum period of BCG maintenance is still controversial. The Southwest Oncology Group BCG maintenance regimen was a weekly dose for 3 weeks at 3, 6, 12, 18, 24, 30 and 36 months .
Read Also: Bladder Pain But No Infection