Treatment Of Pelvic Organ Prolapse
The first treatment your doctor might recommend is pelvic floor physical therapy, which may include . You squeeze and release the muscles you use to hold in gas, which strengthens the muscles that help to support the pelvic organs.
Its important to do Kegels the right way, Dr. Wakamatsu says. A physical therapist can use techniques like biofeedback to help you find the right muscles to squeeze. Physical therapy with Kegels may be enough to relieve prolapse symptoms.
Surgery is an option for women who arent comfortable with the idea of using a pessary, or who have tried it and found it didnt relieve their symptoms. There are several different types of surgery, based on the location and severity of the prolapse and other health issues. For women who have uterine prolapse, often a hysterectomy is recommended. Women who are at high risk for repeated prolapse may have a procedure called sacrocolpopexy, in which the surgeon works through small incisions in the abdomen to reposition the pelvic organs back where they should be.
Dont Miss: Causes Of Weak Bladder Muscles
Instructions For Modified Kegel Exercises
Vaginal muscle control is best obtained when sitting. While sitting, tighten the vaginal and abdominal muscles, then quickly release them. Repeat ten times, quickly tightening and then releasing the vaginal and abdominal muscles. Next, tighten the vaginal and abdominal muscles, but this time hold it for ten seconds. Repeat ten times, tightening and holding the muscles for ten seconds each time. Completing both exercises takes about ten minutes. Perform these exercises three times a day, morning, noon, and night. If you are using a pessary, remove it before starting the exercises. The exercises cannot be done effectively while wearing a pessary.
Most women see an improvement from these simple exercises within a couple of weeks, or, with a more significant prolapse, within a couple of months. They can be done while sitting at a desk, sitting on a couch, or while commuting. And because exercise is non-invasive and there is a good chance it will improve or reverse a first-degree or second degree prolapse, it is well worth the minimal time and effort to do them three times a day.
It is important that these exercises be performed for 10 minutes three times a day, every day. If you do not experience significant improvement within two to three months, the modified Kegel exercises are probably not going to resolve your prolapse.
How Is Uterine Prolapse Treated
There are surgical and non-surgical options for treating uterine prolapse. Your healthcare provider will pick your treatment path based on the severity of your prolapse, your general health, age and whether or not you want children in the future. Treatment is generally effective for most women. Treatment options can include:
Non-surgical options
- Exercise: Special exercises, called Kegel exercises, can help strengthen the pelvic floor muscles. This may be the only treatment needed in mild cases of uterine prolapse. To do Kegel exercises, tighten your pelvic muscles as if you are trying to hold back urine. Hold the muscles tight for a few seconds and then release. Repeat 10 times. You may do these exercises anywhere and at any time .
- Vaginal pessary: A pessary is a rubber or plastic doughnut-shaped device that fits around or under the lower part of the uterus . This device helps prop up the uterus and hold it in place. A healthcare provider will fit and insert the pessary, which must be cleaned frequently and removed before sex.
Surgical options
You May Like: Oregano Oil For Bladder Infection
Increased Pressure Inside The Tummy
Anything that causes an increase in the pressure inside a woman’s abdomen and pelvis can also be a risk factor for the development of pelvic organ prolapse. This can occur because of the strain put on the supporting ligaments and muscles. The most common reason for this increased pressure is during pregnancy and childbirth. However, the same increase in pressure can also occur in:
- Women who are overweight.
- Women who have persistent lung problems, such as a chronic cough.
- Women who frequently strain due to constipation.
- Women who do heavy lifting as part of their job.
What Is A Vaginal Mesh Suspension
This mesh operation is called a sacral colpopexy and is most often performed through an abdominal incision. However, recent innovations now allow this procedure to be performed laparoscopically by experienced laparoscopic surgeons. In some centers the addition of the Da Vinci Robot has assited with laparoscopic support surgery. As with other laparoscopic procedures, the hospital stay is shorter and the recovery faster.
Also Check: Does Azo Bladder Control Help With Incontinence
Will You Use Transvaginal Synthetic Mesh
The FDA has issued several documents on the use of reconstructive materials for pelvic floor surgery. The conclusions to date have been that transvaginal placement of these materials are of uncertain effectiveness and are associated with safety risks. In contrast, use of synthetic mesh for sacral colpopexy or for full-length retropubic or transobturator midurethral slings was considered safe and effective.
Make sure to ask your surgeon plans to use transvaginal mesh and in what way. This way you can weigh the benefits against the risks.
The Major Types Of Pelvic Organ Prolapse And Their Differences
Its been reported that 23.7% of women experience some form of pelvic floor disorder. Common issues range from urinary incontinence to several kinds of pelvic organ prolapse . A prolapse is the slipping down or forward of a part or Read More
Its been reported that 23.7% of women experience some form of pelvic floor disorder. Common issues range from urinary incontinence to several kinds of pelvic organ prolapse . A prolapse is the slipping down or forward of a part or organ, often as a result of weakened or stretched connective tissue. Prolapses happen for both men and women, but women have several more types of prolapse that may affect the pelvic region of their bodies. This may cause pressure, pain during sex, incontinence, stretching sensations or lower back pain, an odd bulging sensation like sitting on a ball and in severe cases the prolapsed organ may sink so that parts are exposed outside of the body. Taking preventative measures, such as doing pelvic floor exercises, may help prevent these issues in women.
Recommended Reading: Turbt Treatment For Bladder Cancer
Also Check: How To Stop Bladder Infection Pain
Pelvic Organ Prolapse Symptoms
You can have a pelvic organ prolapse and not have any symptoms from it. It may just be noticed by a doctor when you are examined for another reason – for example, when you have a cervical smear test.
However, it is common for women to have some symptoms. There are certain symptoms that women with all types of prolapse can have. Symptoms include:
- Sex may be uncomfortable or painful.
- Symptoms are usually worse after long periods of standing and they improve after lying down.
Other symptoms that you may experience can depend on the type of prolapse that you have. They can include the following:
Can Kegel Exercises Prevent Leaking During Sex
Kegel exercises can certainly help. Women who learn to do Kegels correctly and do them regularly have less leaking during intercourse. A recent study from Norway found that women who were taught by a physical therapist the correct way of performing Kegels were more likely to have more satisfying sex than a group of women who were not properly taught these exercises. These women had fewer problems with their sex life and less discomfort with intercourse. We encourage you to do Kegel exercises on a regular basis.
Recommended Reading: How To Insert Catheter In Bladder
How Do I Prevent A Vaginal Prolapse
To reduce your risk of having vaginal prolapse, follow these few tips
- Exercise regularly
If the prolapse is left untreated – over time, it may stay the same or slowly get worse.
In rare cases, severe prolapse can cause obstruction of the kidneys or urinary retention. This may lead to kidney damage or infection.
Vaginal prolapse can happen again even after treatment, however, most treatment procedures provide promising results.
Prolapse Of The Uterus
-
Partly through the opening
-
All the way through the opening, resulting in total uterine prolapse
How far down the uterus drops down determines how severe symptoms are.
Total uterine prolapse can cause pain during walking. Sores may develop on the protruding cervix and cause bleeding, a discharge, and infection.
Constipation Constipation in Adults Constipation is difficult or infrequent bowel movements, hard stool, or a feeling that the rectum is not totally empty after a bowel movement . (See also Constipation read more can occur.
Read Also: Can Weak Bladder Muscles Be Fixed
How To Diagnose And Treat A Prolapsed Bladder
This article was medically reviewed by Lacy Windham, MD. Dr. Windham is a board certified Obstetrician & Gynecologist in Tennessee. She attended medical school at the University of Tennessee Health Science Center in Memphis and completed her residency at the Eastern Virginia Medical School in 2010, where she was awarded the Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, and Most Outstanding Resident Overall.There are 12 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 96% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 129,113 times.
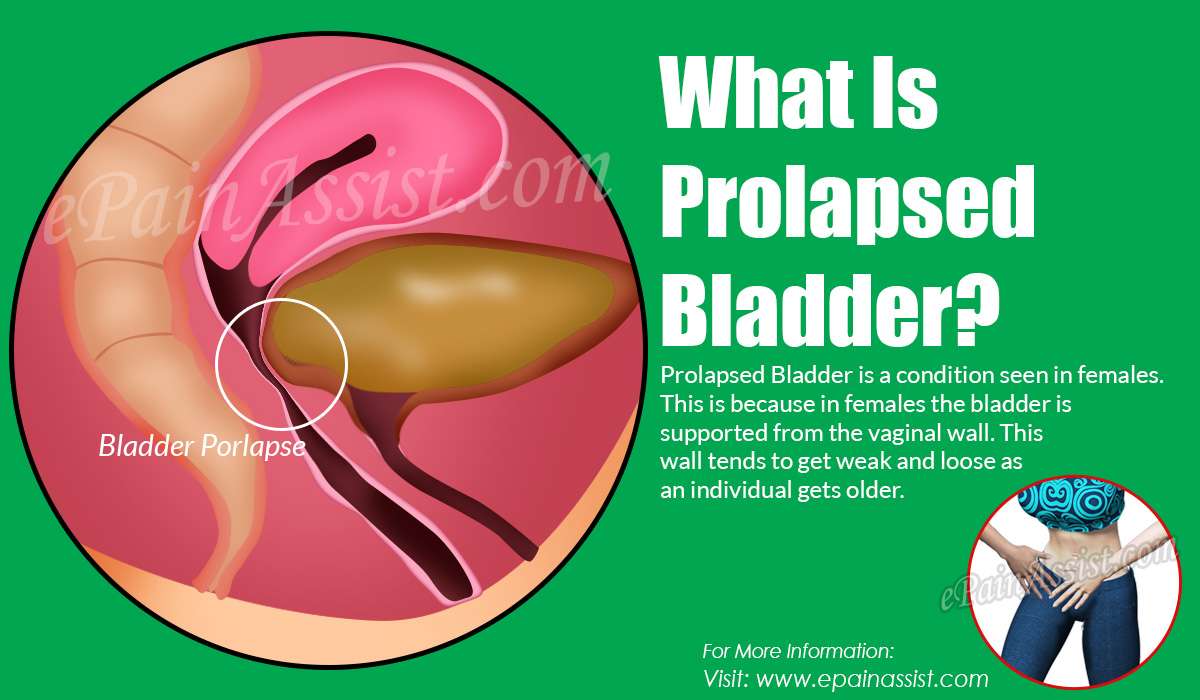
Experts say that your bladder may fall from it’s normal position in your pelvis if your pelvic floor becomes too weak or there’s too much pressure on it.XTrustworthy SourceMayo ClinicEducational website from one of the world’s leading hospitalsGo to source When this happens, your bladder presses on your vaginal wall, which is called a prolapsed bladder. Research suggests that as many as 50% of women have some form of bladder prolapse after pregnancy, so it’s a fairly common problem.XTrustworthy SourceHarvard Medical SchoolHarvard Medical School’s Educational Site for the PublicGo to source If you’re worried you have a prolapsed bladder, talk to your doctor because you have a range of treatment options.
Ring With Knob Pessary
This pessary is used to treat urinary incontinence caused by bladder prolapse.
PEV001
Copyright 2021 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information.
This information is designed as an educational aid for the public. It offers current information and opinions related to women’s health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOGâs complete disclaimer.
Don’t Miss: Can Leukemia Cause Bladder Problems
How To Check Yourself For Prolapse:
Wash your hands. Sit comfortably on a toilet, or on the floor with your hips and knees bent. Make sure you’re in a well-lit room, and have a handheld mirror handy. Gently part your labia and use a handheld mirror to look inside the vaginal canal.
Do you see anything? If you see a “bulge” that protrudes to the level of or outside of the vaginal entrance, then you probably have pelvic organ prolapse . Make an appointment with your healthcare provider for further evaluation.
If you DO NOT see a significant bulge, but you still think that something feels off, or if it looks like something is out of place, then gently bear down. You can also try coughing and see what happens. If gently bearing down and/or coughing produces a bulge, then you might have pelvic organ prolapse.
Finish by checking the same things standing up. After all, we live our life in upright positions… Not lying down on an examination table! It’s important to check for prolapse in functional positions such as sitting and standing.
Real quick Wondering about grades of prolapse? The following is adapted from WebMD, and applies to prolapsed bladders since this is the most common type of prolapse.
Prolapsed bladders are separated into four grades. The grades are based on how much the bladder presses into the front vaginal wall. Please note that a prolapsed bladder does not actually protrude through vaginal wall, it simply presses into it, which is what causes the protrusion or bulge.
What You Need To Know
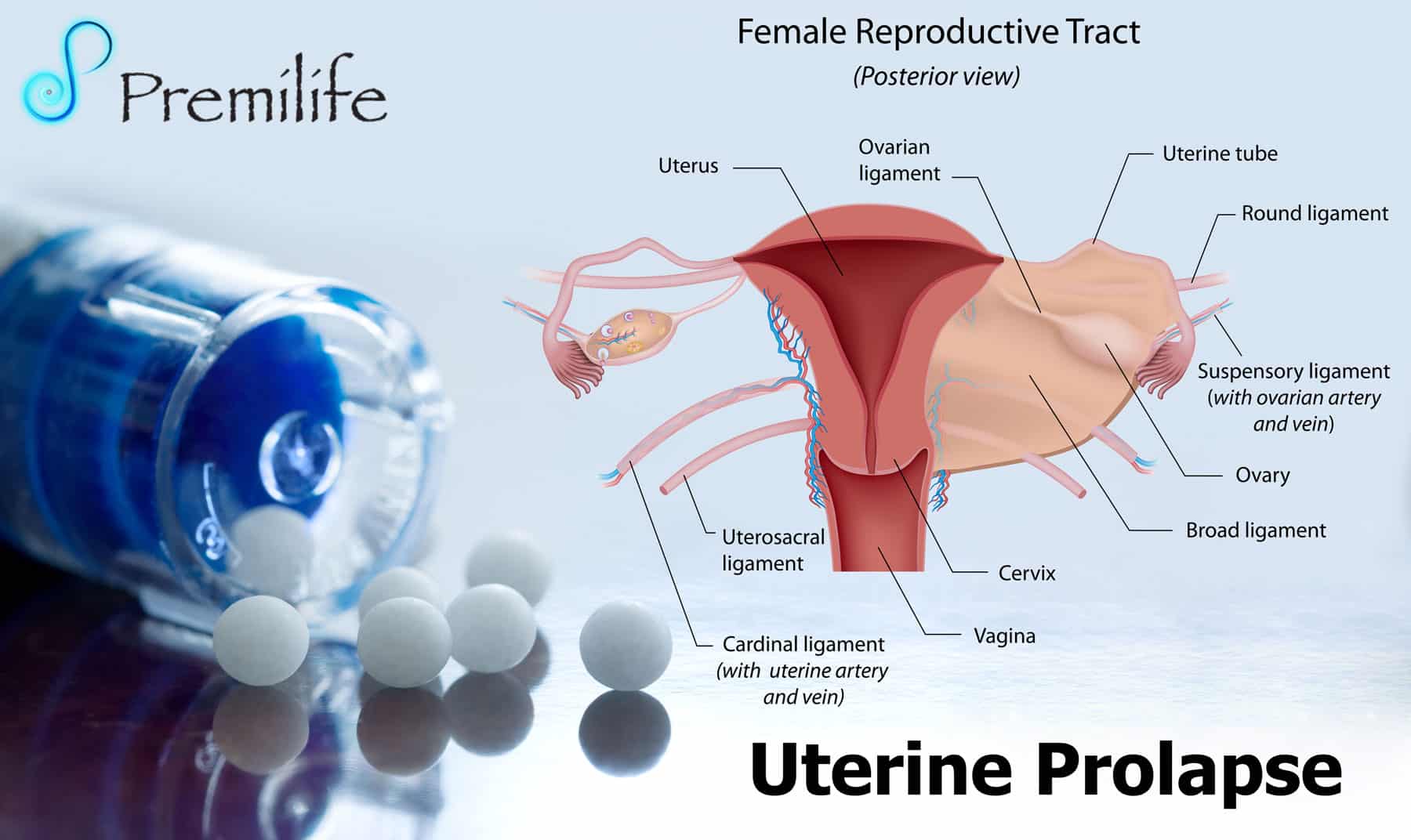
- When pelvic muscle, tissue and ligaments weaken, the uterus can drop down into the vaginal canal, causing uterine prolapse.
- Nearly one-half of all women between ages 50 and 79 have some degree of uterine or vaginal vault prolapse, or some other form of pelvic organ prolapse.
- Factors that increase your risk of uterine prolapse include childbirth, age, obesity, chronic constipation and having a hysterectomy.
- There is no definitive way to prevent uterine prolapse. Losing weight, eating a fiber-rich diet, quitting smoking and performing pelvic floor exercises can help to reduce the risk of this condition.
You May Like: Pain In My Bladder Uterus Area
How Is Uterine Prolapse Diagnosed
If your healthcare provider thinks that you have a prolapsed uterus, he or she will probably do a physical exam to check your pelvis. If you also have urinary incontinence or a feel like you cant empty your bladder, your doctor may do a procedure called a cystoscopy to examine your bladder and urethra.
Your healthcare provider might also order an MRI . This procedure uses a magnet and radio waves to create images. This will allow your healthcare provider to get a good look at your kidneys and other pelvic organs.
When Is Surgery Needed For A Prolapsed Bladder
Severe prolapsed bladders that cannot be managed with a pessary and/or behavioral therapy usually require surgery to correct them. There are several different types of surgery depending on the severity of the prolapse and whether or not other organs are affected.
- The bladder is repaired with an incision in the vaginal wall.
- The prolapsed area is closed and the wall is strengthened. This may be done primarily using one’s own tissues or through the use of grafts, which may be biologic or synthetic .
- If one has stress urinary incontinence, this is also corrected.
- Depending on the procedure, surgery can be performed while the woman is under general, regional, or local anesthesia. Most women are discharged home on the same day of surgery.
- Various materials have been used to strengthen pelvic weakness associated with prolapsed bladder. A surgeon should explain in detail the risks, benefits, and potential complications of these materials, and he or she should explain the procedure itself before proceeding with the surgery. Complications related to surgery may include bleeding, infection, pain, urinary incontinence, recurrent prolapse, trouble urinating, and injury to the bladder.
- The cost of surgical treatment will vary with the procedure performed, the length of hospitalization, and the presence/absence of other medical conditions.
- After surgery, most women can expect to return to a normal level of activity after 6 weeks.
Recommended Reading: Types Of Pessaries For Bladder Prolapse
Will Sex Be Better If You Have Surgery
To answer this, a recent American study questioned a group of women before and after surgery to repair a prolapse or incontinence. About half of these women were sexually active. Before surgery, 82% of the sexually active women reported being happy with their sex lives, and after surgery, 89% of the women felt happy with their sexual relationship.
However, a study brought out a number of interesting findings. For one, the frequency of intercourse did not change following surgery. And two, while only 8% of the women had pain with intercourse before surgery, 19% noted pain with intercourse after surgery. About one quarter of the women who had a repair of a bulging rectum developed pain with intercourse. About one third of the women who had repair of a rectocele and a bladder suspension had painful intercourse. Unfortunately, the researchers did not ask these women why they were more satisfied with their sex lives even though more of them had painful intercourse.
Another study performed in Sweden may shed some light. This study found that one third of women noted an increased interest in sex after incontinence surgery, and one half of their male partners were more interested in sex. It could be that knowing the repair for the prolapse or incontinence had been addressed was enough to make the couples feel better about sex.
Causes And Risk Factors Of Uterine Prolapse
The most common cause of vaginal prolapse is traumatic or lengthy childbirth. Pregnancy puts significant stress on the pelvic floor, and it can be further exacerbated by trauma during labor.
In addition to that, various risk factors can increase the likelihood of developing uterine prolapse. They include:
Physical or emotional trauma
Scar tissue and fascial adhesions
Hormonal shifts and imbalances
Biomechanic and genetic differences that determine the natural elasticity of your tissues
Obesity or significant weight gain
Chronic constipation and diet that leads to frequent constipation
Poor nutrition
Prior history of pelvic floor dysfunction such as pelvic floor tightness
Multiple pregnancies
Pregnancies carrying more than one baby
Frequent pregnancies with little recovery time between them
Lack of adequate recovery postpartum
Carrying heavy loads
Delivery thats performed by unskilled birth attendants
Varying health conditions
History of pelvic surgery
Menopause is another significant risk factor. As muscles and tissues lose their tone and elasticity, the chances of developing uterine prolapse increase.
Diagnosis
You may have pelvic prolapse if your symptoms resemble the ones described and demonstrated in these pelvic organ prolapse photos. However, if you want a more accurate assessment of whether you have pelvic prolapse, you need to undergo a pelvic exam.
Also Check: What Can I Do For An Overactive Bladder
Should You Discuss Sexual Problems With Your Doctor
If many women have problems talking to their partners about sex, isn’t it even more difficult for them to broach the subject with their doctors? To complicate things even further, doctors are often uncomfortable about discussing sex and are rarely well trained to do so. Adding incontinence to a conversation may make both a woman and her doctor even more reluctant to pursue further discussion.
To illustrate what a significant problem this is, interviews with 324 sexually active women found that only 2 women had volunteered information about having incontinence during sex. However, when specifically asked about this symptom, 77 additional women acknowledged that they had incontinence during intercourse.
Patients and doctors need to do a better job communicating about incontinence and sexuality. If your doctor doesn’t ask about incontinence, it is important for you to bring it up if there is a problem. If your doctor seems uncomfortable with the subject, ask for a referral to someone who regularly deals with incontinence. If you are having a problem with incontinence and sexuality, more than likely you will need to bring this up as well. If your doctor is not equipped to discuss this with you, ask for the name of a knowledgeable therapist who can help.
If your doctor doesn’t know such specialists, make an effort to find someone on your own. The important thing is to get what you need. You’re not alone with this problem.