Start And Spread Of Bladder Cancer
The wall of the bladder has many several layers. Each layer is made up of different kinds of cells .
Most bladder cancers start in the innermost lining of the bladder, which is called the urothelium or transitional epithelium. As the cancer grows into or through the other layers in the bladder wall, it has a higher stage, becomes more advanced, and can be harder to treat.
Over time, the cancer might grow outside the bladder and into nearby structures. It might spread to nearby lymph nodes, or to other parts of the body.
You May Like: What Is Infiltrating Ductal Carcinoma
Followup And Quality Of Life
- âQuality of life in the form of a validated patient-reported outcome measure or QoL instrument should be captured for all patients at each visit.
- âFollowup schedules should be tailored to final pathological TNM staging.
- âFollowup visits after RC should include a metastatic survey, including an investigation for upper tract recurrence, assessment for hydronephrosis, and laboratory studies to detect metabolic complications of diversion .
- âIn patients at high risk for urethral or upper tract recurrence, urethral washings +/â urethroscopy and urine should be collected for cytological examination at interval followup visits.
- âPatients treated with a bladder preservation approach should also receive, in addition to the same investigations performed for RC patients, long-term cystoscopic evaluation at each followup visit to survey the remaining urothelium.
- âIntravesical recurrences after bladder preservation may be managed as per primary bladder tumors based on pathological assessment after TURBT.Careful consideration for RC should occur for high-risk recurrences.
- âEndoscopic biopsy is recommended following TMT to assess response.
Stage Iv Bladder Cancer Treatment
Only a small fraction of patients with stage IV bladder cancer can be cured, and for many patients, the emphasis is on palliation of symptoms. The potential for cure is restricted to patients with stage IV disease with involvement of pelvic organs by direct extension or metastases to regional lymph nodes.
Also Check: Harbor Freight Drain Cleaning Bladder
What Is The Prognosis For Someone With Prcc
The estimate of how a disease will affect you long-term is called prognosis. Every person is different and prognosis will depend on many factors, such as
- Where the tumor is in your body
- If the cancer has spread to other parts of your body
- How much of the tumor was taken out during surgery
If you want information on your prognosis, it is important to talk to your doctor. NCI also has resources to help you understand cancer prognosis.
Doctors estimate survival rates by how groups of people with PRCC have done in the past. Because there are so few people with PRCC, these rates may not be very accurate. They also cant consider newer treatments being developed.
In general, type 2 papillary renal cell carcinoma has a poorer prognosis than type 1.
Related Resources
Also Check: How Often Does Squamous Cell Carcinoma Spread
Non Muscle Invasive Bladder Cancer
In non muscle invasive bladder cancers, the cancer is only in the lining of the bladder. It has not grown into the deeper layers of the bladder wall. Non muscle invasive bladder cancer is also called superficial bladder cancer, or early bladder cancer.
Early bladder cancer usually appears as small growths, shaped like mushrooms. These grow out of the bladder lining. This is called papillary bladder cancer. Your surgeon can remove these growths and they may never come back.
But some types of early bladder cancer are more likely to come back. These include carcinoma in situ and high grade T1 tumours. T1 stands for the size of the tumour.
Carcinoma in situ
Unlike other early bladder cancers, areas of CIS are flat. They do not grow out of the bladder wall. In CIS the cancer cells look very abnormal and are likely to grow quickly. This is called high grade. It is more likely to come back than other types of early bladder cancer.
High grade T1 tumours
T1 tumours are early cancers that have grown from the bladder lining into a layer underneath, called the lamina propria. High grade T1 tumours are early cancers, but they can grow very quickly.
Risk groups
Doctors divide early bladder cancer into 3 risk groups. These risk groups describe how likely it is that your cancer will spread further or come back after treatment. Your risk group depends on several factors including the size of the tumour , what the tissue looks like under the microscope and type of bladder tumour.
Read Also: How To Treat Overactive Bladder
Cancerous Tumours Of The Bladder
A cancerous tumour of the bladder can grow into nearby tissue and destroy it. It can also spread to other parts of the body. Cancerous tumours are also called malignant tumours.
Bladder cancer is often divided into 3 groups based on how much it has grown into the bladder wall.
- Non-invasive bladder cancer is only in the inner lining of the bladder .
- Non–muscle-invasive bladder cancer has only grown into the connective tissue layer .
- Muscle-invasive bladder cancer has grown into the muscles deep within the bladder wall and sometimes into the fat that surrounds the bladder.
Urothelial Carcinoma With Trophoblastic Differentiation
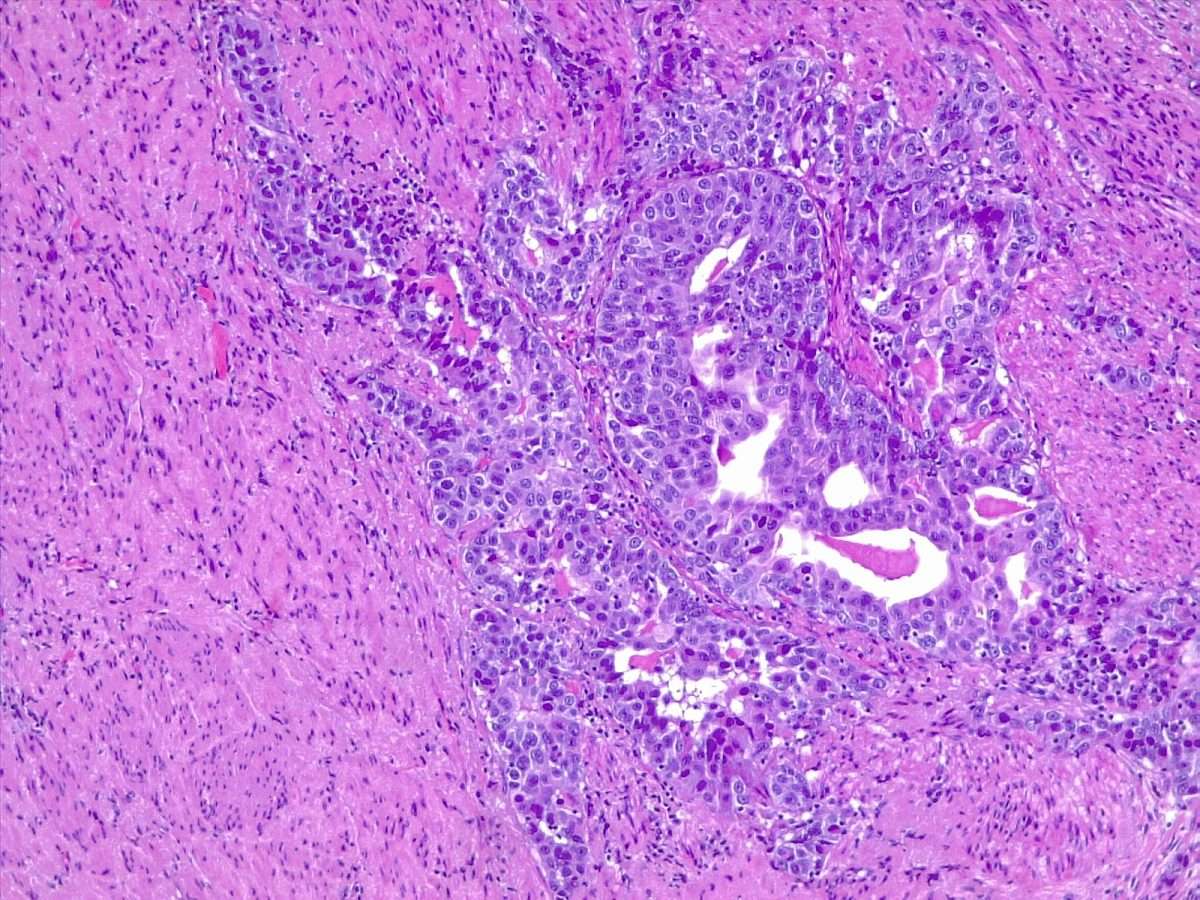
More than 30 cases of urothelial carcinoma with areas of trophoblastic differentiation have been reported and a small subset has had symptoms related to excess human chorionic gonadotropin production including gynecomastia., , , , Although some of the early reports have described tumors that apparently were composed solely of tissue resembling choriocarcinoma, most tumors reported in the last three decades or so have been composed of a mixture of urothelial carcinoma with trophoblastic elements. A single case of micropapillary carcinoma with trophoblastic elements has been reported.
Figure 11
Also Check: Can Merkel Cell Carcinoma Be Cured
Also Check: Do You Bleed With A Bladder Infection
Cellular Classification Of Bladder Cancer
More than 90% of bladder cancers are transitional cell carcinomas derived from the uroepithelium. About 2% to 7% are squamous cell carcinomas, and 2% are adenocarcinomas. Adenocarcinomas may be of urachal origin or nonurachal origin the latter type is generally thought to arise from metaplasia of chronically irritated transitional epithelium. Small cell carcinomas also may develop in the bladder. Sarcomas of the bladder are very rare.
Pathologic grade of transitional cell carcinomas, which is based on cellular atypia, nuclear abnormalities, and the number of mitotic figures, is of great prognostic importance.
References
Stage Groups For Bladder Cancer
Doctors assign the stage of the bladder cancer by combining the T, N, and M classifications .
Bladder cancer
Stage 0a: This is an early cancer that is only found on the surface of the inner lining of the bladder. Cancer cells are grouped together and can often be easily removed. The cancer has not invaded the muscle or connective tissue of the bladder wall. This type of bladder cancer is also called noninvasive papillary urothelial carcinoma .
Stage 0is: This stage of cancer, also known as a flat tumor or carcinoma in situ , is found only on the inner lining of the bladder. It has not grown in toward the hollow part of the bladder, and it has not spread to the thick layer of muscle or connective tissue of the bladder . This is always a high-grade cancer and is considered an aggressive disease because it can lead to muscle-invasive disease.
Stage I: The cancer has grown through the inner lining of the bladder and into the lamina propria. It has not spread to the thick layer of muscle in the bladder wall or to lymph nodes or other organs .
Stage II: The cancer has spread into the thick muscle wall of the bladder. It is also called invasive cancer or muscle-invasive cancer. The tumor has not reached the fatty tissue surrounding the bladder and has not spread to the lymph nodes or other organs .
Stage IV: The tumor has spread into the pelvic wall or abdominal wall, or the cancer has spread to lymph nodes outside of the pelvis or to other parts of the body.
Recurrent cancer
Also Check: Non Muscle Invasive Bladder Cancer Ppt
What Is Bladder Cancer
Bladder cancer starts when cells that make up the urinary bladder start to grow out of control. As more cancer cells develop, they can form a tumor and, with time, spread to other parts of the body.
The bladder is a hollow organ in the lower pelvis. It has flexible, muscular walls that can stretch to hold urine and squeeze to send it out of the body. The bladders main job is to store urine. Urine is liquid waste made by the 2 kidneys and then carried to the bladder through 2 tubes called ureters. When you urinate, the muscles in the bladder contract, and urine is forced out of the bladder through a tube called the urethra.
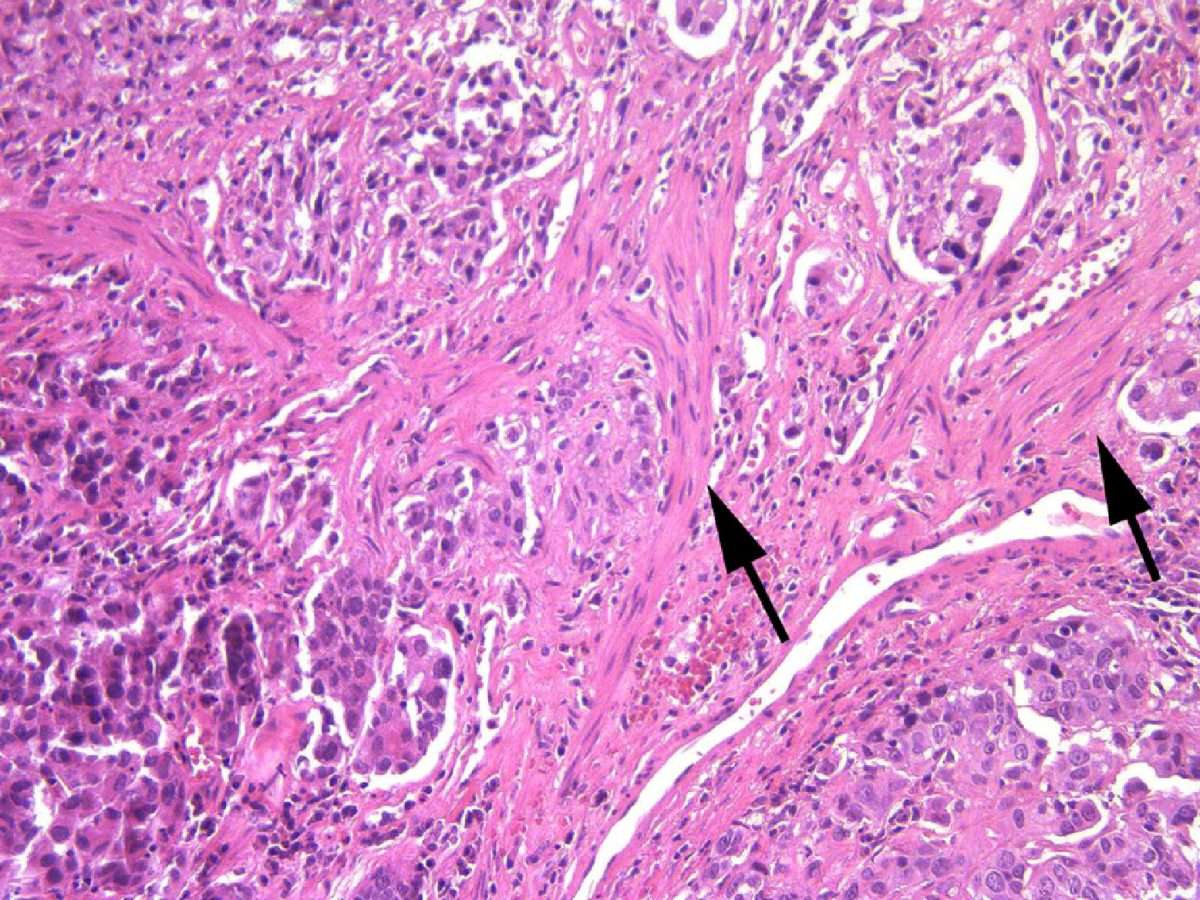
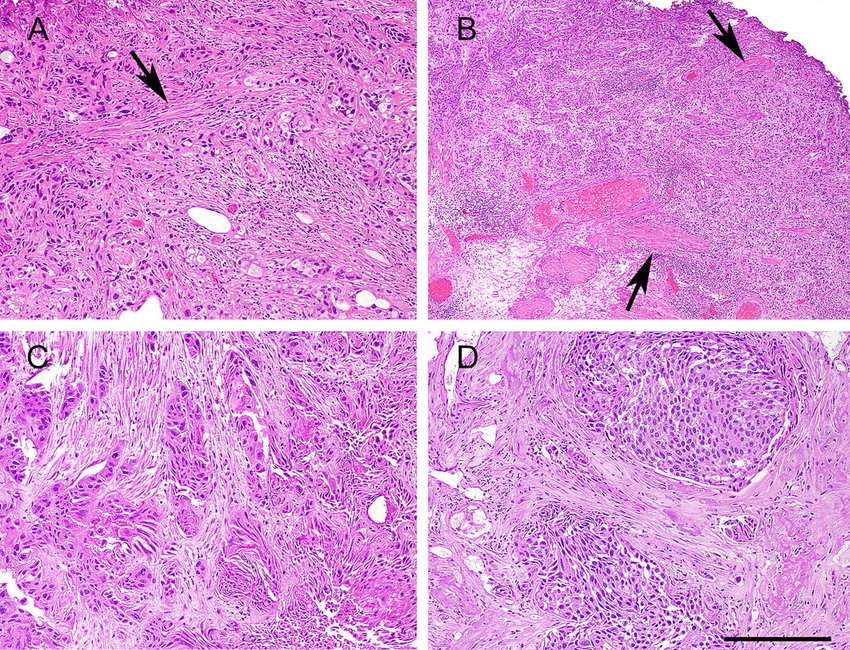
Muscularis Propria Invasion In The Urinary Bladder
The presence or absence of muscularis propria invasion in the urinary bladder is a very important determination, as the clinical management changes between T1 and T2:
- T1: usually conservative treatment .
- T2: radical treatment .
A thin layer of discontinous muscularis mucuosae is present and, especially if hypertrophic, may be confused with muscuaris propria .
Staging of bladder cancer is dealt with in the bladder cancer staging article.
Muscle invasive bladder cancer redirects to this article and refers to invasion of the muscularis propria.
Bladder muscularis propria invasion and urinary bladder muscularis propria invasion redirect to this article.
You May Like: Ways To Stop Bladder Leakage
Morphologic Variants Of Urothelial Carcinoma
Some cases of urothelial carcinoma show morphologic patterns that are recognized as variants morphology. Those include nested variant, micropapillary, lymphoepithelioma-like, sarcomatoid, small cell carcinoma, and adenocarcinoma. These are frequently under-recognized in bladder biopsies and could have therapeutic implications with different criteria for surgery and different chemotherapy regimens.
Dont Miss: What Do Melanoma Spots Look Like
Treatment Of Bladder Cancer By Stage
Most of the time, treatment of bladder cancer is based on the tumors clinical stage when its first diagnosed. This includes how deep its thought to have grown into the bladder wall and whether it has spread beyond the bladder. Other factors, such as the size of the tumor, how fast the cancer cells are growing , and a persons overall health and preferences, also affect treatment options.
Dont Miss: How To Take Care Of A Bladder Infection At Home
Read Also: If I Have A Bladder Infection What Should I Do
Treating Stage 0 Bladder Cancer
Stage 0 bladder cancer includes non-invasive papillary carcinoma and flat non-invasive carcinoma . In either case, the cancer is only in the inner lining layer of the bladder. It has not invaded the bladder wall.
This early stage of bladder cancer is most often treated with transurethral resection with fulguration followed by intravesical therapy within 24 hours.
Prognosis And Life Expectancy
In general, papillary urothelial cancers have a better prognosis than other types of bladder cancer. Your specific outlook depends on the stage and grade of your cancer. High-grade cancers can spread. Low-grade papillary cancers are less likely to spread. Papillary cancers can also return after theyve been treated.
Read Also: What Is Merkel Cell Skin Cancer
You May Like: Can Bladder Cancer Cause Bowel Problems
Other Ways Of Describing Bladder Cancer
In addition to its cell type, bladder cancer may be described as noninvasive, non-muscle-invasive, or muscle-invasive.
-
Noninvasive. Noninvasive bladder cancer includes noninvasive papillary carcinoma and carcinoma in situ . Noninvasive papillary carcinoma is a growth found on a small section of tissue that is easily removed. This is called stage Ta. CIS is cancer that is found only on or near the surface of the bladder, which is called stage Tis. See Stages and Grades for more information.
-
Non-muscle-invasive. Non-muscle-invasive bladder cancer typically has only grown into the lamina propria and not into muscle, also called stage I. Non-muscle-invasive cancer may also be called superficial cancer, although this term is being used less often because it may incorrectly suggest that the cancer is not serious.
-
Muscle-invasive. Muscle-invasive bladder cancer has grown into the muscle of the bladder wall and sometimes into the fatty layers or surrounding tissues or organs outside the bladder.
It is important to note that non-muscle-invasive bladder cancer has the potential of spreading into the bladder muscle or to other parts of the body. Additionally, all cell types of bladder cancer can spread beyond the bladder to other areas of the body through a process known as metastasis.
The Impact Of Tumor Invasion To Muscularis Mucosaevascular Plexus On Patient Outcome In Pt1 Bladder Urothelial Carcinoma
- Ahmet SahanKartal Dr. Lutfi Kirdar Training and Research Hospital, Department of Urology, Istanbul, Turkey.
- Fatma GerinMarmara University, Department of Pathology, Istanbul, Turkey.
- Asgar GarayevMarmara University, Department of Urology, Istanbul, Turkey.
- Emine BozkurtlarMarmara University, Department of Pathology, Istanbul, Turkey.
- Alkan Çubuk | Kartal Dr. Lutfi Kirdar Training and Research Hospital, Department of Urology, Istanbul, Turkey.
- Orkunt OzkaptanKartal Dr. Lutfi Kirdar Training and Research Hospital, Department of Urology, Istanbul, Turkey.
- Kasm ErtasYuzuncu Yl University, Department of Urology, Van, Turkey.
- Yloren TandrMarmara University, Department of Urology, Istanbul, Turkey.
- Haydar Kamil CamMarmara University, Department of Urology, Istanbul, Turkey.
- Ilker TnayMarmara University, Department of Urology, Istanbul, Turkey.
Don’t Miss: Weak Bladder Control After Childbirth
Treatment Of Stage Iv Bladder Cancer
In This Section
Chemotherapy alone or as an adjunct to local treatment
Cisplatin-based combination chemotherapy regimens are the standard of care for first-line therapy for stage IV bladder cancer in patients who can tolerate it. The only chemotherapy regimens that have been shown to result in longer survival in randomized controlled trials are MVAC, dose-dense MVAC, and CMV. GC was compared with MVAC in a randomized controlled trial and neither regimen was associated with a statistically significant difference in response rate or survival. The two regimens are generally considered equivalent, but they have never been compared in a noninferiority trial. Of note, patients with good performance status and lymph node-only disease have a low but significant rate of achieving a durable complete remission with MVAC or GC. In the large, randomized, controlled trial comparing MVAC with GC, for example, 5-year OS in patients with lymph node-only disease was 20.9%. Dose-dense MVAC and standard-dose MVAC were compared in a randomized controlled trial, and dose-dense MVAC was associated with longer survival.
Ongoing studies are evaluating new chemotherapy combinations.
Evidence :
Immunotherapy
Pembrolizumab
Evidence :
Evidence :
Low Grade And High Grade
Bladder cancer can also be described as either low grade or high grade.
Low grade bladder cancer means that your cancer is less likely to grow, spread and come back after treatment. High grade means your cancer is more likely to grow spread and come back after treatment.
For example, if you have early bladder cancer but the cells are high grade, youâre more likely to need further treatment after surgery. This is to reduce the risk of your cancer coming back.
Low grade is the same as grade 1. High grade is the same as grade 3. Grade 2 can be split into either low or high grade. Carcinoma in situ tumours are high grade.
You May Like: How Deadly Is Squamous Cell Carcinoma
Don’t Miss: How Long Should A Bladder Infection Last
Treatment Of Stage I Bladder Cancer
In This Section
TUR with fulguration followed by an immediate postoperative instillation of intravesical chemotherapy
TUR and fulguration are the most common and conservative forms of management. Careful surveillance of subsequent bladder tumor progression is important. Because most bladder cancers recur after TUR, one immediate intravesical instillation of chemotherapy after TUR is widely used. Numerous randomized, controlled trials have evaluated this practice, and a meta-analysis of seven trials reported that a single intravesical treatment with chemotherapy reduced the odds of recurrence by 39% .
TUR with fulguration
Staging a bladder cancer via TUR is based on the extent of invasion. To assess whether cancer has invaded the muscle, muscularis propria must be present in the resected tissue. While a repeat TUR is generally considered mandatory for T1 and high-grade noninvasive bladder cancers if no muscularis propria is present in the resected tissue from the first TUR, many experts recommend that a second TUR be routinely performed within 2 to 6 weeks of the first TUR to confirm staging and achieve a more complete resection. The rationale for this derives from numerous findings, including the following:
Evidence :
Evidence :
Evidence :
Evidence :
Evidence :
Evidence :
What Is Muscle Invasive Bladder Cancer
Muscle invasive bladder cancer is a cancer that spreads into the detrusor muscle of the bladder. The detrusor muscle is the thick muscle deep in the bladder wall. This cancer is more likely to spread to other parts of the body.
In the U.S., bladder cancer is the third most common cancer in men. Each year, there are more than 83,000 new cases diagnosed in men and women. About 25% of bladder cancers are MIBC. Bladder cancer is more common as a person grows older. It is found most often in the age group of 75-84. Caucasians are more likely to get bladder cancer than any other ethnicity. But there are more African-Americans who do not survive the disease.
What is Cancer?
Cancer is when your body cells grow out of control. When this happens, the body cannot work the way it should. Most cancers form a lump called a tumor or a growth. Some cancers grow and spread fast. Others grow more slowly. Not all lumps are cancers. Cancerous lumps are sometimes called malignant tumors.
What is Bladder Cancer?
When cells of the bladder grow abnormally, they can become bladder cancer. A person with bladder cancer will have one or more tumors in his/her bladder.
How Does Bladder Cancer Develop and Spread?
The bladder wall has many layers, made up of different types of cells. Most bladder cancers start in the urothelium or transitional epithelium. This is the inside lining of the bladder. Transitional cell carcinoma is cancer that forms in the cells of the urothelium.
Also Check: Types Of Pessaries For Bladder Prolapse