How Is It Diagnosed
Thereâs no test for interstitial cystitis. If you go to your doctor complaining about bladder pain along with frequency and the urgency to pee, the next step is to rule out what else it could be.
Both men and women would first need to rule out urinary tract infections, bladder cancer, sexually transmitted diseases, and kidney stones.
In women, endometriosis is another possibility. For men, IC can be mistaken for an inflamed prostate or chronic pelvic pain syndrome.
These tests can rule out other conditions:
- Urinalysis and urine culture. Youâll be asked to pee in a cup. Itâll be sent to a lab to check for infection.
- Postvoid residual urine volume. Using an ultrasound, this test measures the amount of pee that remains in your bladder after you go to the bathroom.
- Cystoscopy. A thin tube with a camera is used to see the inside of the bladder and urethra. This is usually done only if there is blood in your pee or if treatment doesnât help.
- Bladder and urethra biopsy. A small piece of tissue is taken and tested. This is usually done during cystoscopy.
- Bladder stretching. Your bladder is filled with liquid or gas to stretch it out. Youâll be asleep under anesthesia. Sometimes this is also used as a treatment. This is done with a cystoscopy.
- Prostate fluid culture . Your doctor will need to press on your prostate and milk a sample to test. This is not commonly done.
Antibiotics Started A Vicious Cycle
Whilst on my honeymoon I got my first urinary tract infection. Honeymoon cystitis they called it. When we returned from our honeymoon I had another first, I found out I was pregnant. Nine months later my daughter was born by emergency cesarean. Intravenous antibiotics were given to me to prevent an infection which, unfortunately, led to me developing vaginal thrush. Over the following years, I had a couple more UTIs and continued to get thrush sporadically.
Two more daughters were born by cesarean over the following four years which meant two more lots of intravenous antibiotics. At the time of my third pregnancy, I was suffering from enormous stress due to poverty and a failing business. It was after my third childs birth, that my urinary tract infections really started to become an issue. I was visiting the doctor regularly with depression, thrush and UTIs. It seemed to be a vicious cycle. The more UTIs I got the more antibiotics I got the more thrush I got the more depressed I got. Worse was to follow.
Finally A Diagnosis Of Interstitial Cystitis
Back in New Zealand, I found a pelvic floor physiotherapist. I realised through this therapy, that my pelvic floor was clenched on all of the time, creating more issues. With the therapy I learned to relax those muscles which, in turn, decreased some of the pain. After completing a second cystoscopy with yet another urologist, I was diagnosed with Interstitial cystitis with Hunners ulcers. I was so excited to have a name for this condition. Finally!!! This was good news. The bad news? There was no cure for Interstitial Cystitis.
The doctor put me on a low-grade anti-depressant which would dull my pain sensors in the vagina and bladder and hopefully give me some relief. This did relieve some of the pain, but I still had a swollen belly, lower pain in the abdomen, recurring UTIs and cystitis. Fantastic! Next, he lasered my bladder , hoping that the new skin that would grow would be healthier. This, although painful, had very little effect. Déjà Vu, I was starting to feel like a guinea pig and wondering when my Interstitial Cystitis would get manageable.
Recommended Reading: Why Do I Get Frequent Bladder Infections
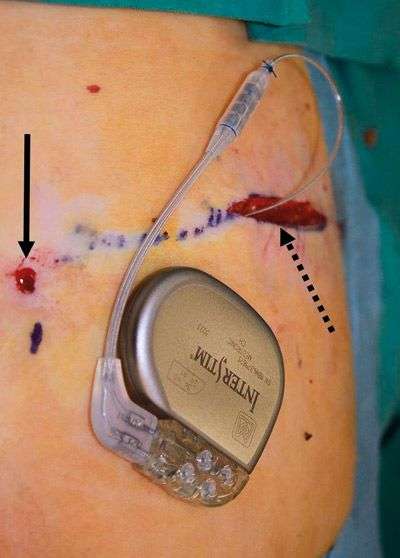
Medtronic Bladder Control Therapy Delivered By The Interstim System
THE RELIEF YOUVE BEEN WAITING FOR
When lifestyle changes and medications fail, Medtronic bladder control therapy delivered by the InterStim systems can help. This therapy is simple and discreet, and it delivers the kind of relief that lets you enjoy the activities you love without a second thought.
- Targets the nerves that control your bladder to help it function normally again
- 85% of people using the InterStim system achieved success in the rst year,4
- 3X greater improvements in quality of life compared to medications6
- Lets you see if it works before you and your doctor decide
- Allows you to get full-body MRI scans if you need them
- Hundreds of thousands of people have experienced relief with this safe, FDA-approved and minimally invasive therapy
THE CHOICE IS YOURS
- The recharge-free InterStim II system may be best for most people because its simple, convenient, and low maintenance.
- The rechargeable InterStim Micro system is smaller, lasts longer, and requires regular recharging sessions.
Wake Forest Baptist Health Urology Named Interstim Center Of Excellence For Overactive Bladder Care
Wake Forest Baptist Health Urology has been named an InterStim Center of Excellence, making it one of a few in the country to earn this prestigious designation for treating overactive bladder and incontinence.
The InterStim Center of Excellence, awarded by Medtronic, recognizes physicians who demonstrate exemplary use of the InterStim System and a commitment to patient care for those suffering from symptoms associated with overactive bladder, accidental bowel leakage and urinary incontinence. As many as 30 percent of men and 40 percent of women in the United States live with overactive bladder symptoms, according to the Urology Care Foundation.
Robert J. Evans, MD, a board certified urologist and professor of urology and obstetrics and gynecology, is one of a few urologists in the state to offer and implant the MRI compatible InterStim neuromodulation lead. Evans has also been named the Interstitial Cystitis /Bladder Pain Syndrome Doctor of the Year for the last seven years, based on world-wide polls of interstitial cystitis patients.
InterStim Therapy, also known as sacral neuromodulation, uses an implantable device to send mild electrical impulses to stimulate the sacral nerves. Those nerves control the bladder and the muscles related to urinary and bowel function.
The Center of Excellence designation is awarded based on several criteria, including:
Also Check: Bladder Infection Clear Up On Its Own
Complication Rates By Type Of Sling
Before undergoing bladder sling surgery, women should ask their doctors about the technique they plan to use. Complication rates may vary depending on the type of mesh sling and technique.
A 2010 study of bladder sling procedures by Z. Chen and colleagues published in Urologia analyzed the outcomes of 187 women who received bladder slings to treat stress urinary incontinence. Authors found that transobturator vaginal tape inside-out and transobturator vaginal tape out-inside are simpler techniques with fewer complications compared to tension-free vaginal tape .
Women who used TVT had an average hospital stay of five days versus about two days for the TOT group.
The complication rate in the study was:
- 15.6 percent for tension-free vaginal tape
- 9.20 percent for transobturator vaginal tape inside-out
- 8.90 percent for transobturator vaginal tape out-inside
Complications from the procedures included discomfort with urinating, bleeding outside blood vessels and dysfunction of lower limbs. TVT was the only procedure associated with bladder perforation. Despite the complication rate, doctors found the slings safe.
The three tension-free urethral suspension techniques have similar efficacy, all of them are safe and effective procedures for the treatment of female SUI, authors wrote.
Changes To Your Lifestyle
It is likely that you will be recommended to make some changes to your lifestyle, especially your diet. Certain foods and drinks can irritate the lining of your bladder and make your symptoms worse. These may include alcohol, tomatoes, spices, chocolate, caffeinated and citrus drinks and acidic foods. It may be worthwhile making a food diary to try to assess which foods aggravate and worsen your symptoms.
The simplest way to find out whether any foods bother your bladder is to try an elimination diet for one to two weeks. On an elimination diet, you stop eating all foods that could irritate your bladder. If your bladder symptoms improve while you are on the elimination diet, this means that at least one of the foods was irritating your bladder. The next step is to find out exactly which foods cause bladder problems for you. You should then try eating one food from the list of foods you stopped eating. If this food does not bother your bladder within 24 hours, this food is likely safe and can be added back into your regular diet. The next day, try eating a second food from the list, and so on. In this way, you will add the foods back into your diet one at a time and your bladder symptoms will tell you if any food causes problems for you.
Some people look at ways to reduce their stress levels, as this can actually improve their symptoms.
Don’t Miss: What Is The Best Exercise For The Bladder
Sacral Nerve Stimulation For Pain Relief In Interstitial Cystitis
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Rent for 48h to view
- Buy Cloud Access for unlimited viewing via different devices
- Synchronizing in the ReadCube Cloud
- Printing and saving restrictions apply
USD 8.50
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Can Bladder Endometriosis Be Treated By Minimally Invasive Techniques
Yes, but only by an experienced surgeon. To resect a portion of the bladder and repair the bladder by video-assisted laparoscopy or robotic-assisted laparoscopy requires a high level of skill with those instruments. As mentioned, Drs. Nezhat were the first to perform minimally invasive surgeries for the treatment of all forms of endometriosis, including bladder endometriosis. After nearly 3 decades, Drs. Nezhat have now performed among the most, if not the most, endometriosis surgeries in the world using minimally invasive and robotic techniques.
A cystoscopy, as shown above, is a procedure in which a camera is placed inside of your bladder to help your doctor visualize your bladder and provide an accurate diagnosis.
However, even a cystoscopy can sometimes miss endometriosis that affects only the outside of the bladder. Therefore, multiple diagnostic tools are sometimes required to achieve an accurate diagnosis.
With the bladder so close to the uterus, its sometimes difficult for patients to determine from which organ the pain is emanating.
Thats why a careful examination is required so that your doctor can properly treat each area.
A common symptom of bladder endometriosis is urinary frequency. However, urinary frequency can also be a symptom of many other disorders.
Thats why its important that you receive a very careful examination to rule out other disorders.
Read Also: Homeopathic Cure For Bladder Infection
Neuromodulation Modalities In Urology
The spectrum of neuromodulation modalities in urology has evolved yet focuses around two manners that correspond to our understanding of the innervation of the lower urinary tract and pelvic floor muscles: sacral neuromodulation, by sacral anterior root stimulation, sacral nerve modulation and recently pudendal nerve stimulation and its derivatives, and less invasive neuromodulators and peripheral nerve stimulators, the most studied of which is posterior tibial nerve stimulation.
When To See A Gp
You should see a GP if you have persistent pelvic pain or you notice a change in your usual peeing pattern.
These symptoms can have a number of causes, so it’s a good idea to get a proper diagnosis.
The GP can refer you to a hospital specialist like a urologist, a specialist in conditions affecting the urinary system, for further tests, such as a cystoscopy. A cystoscopy is a procedure to examine the inside of the bladder.
Don’t Miss: Best Supplement For Overactive Bladder
Concerns About Neural Damage Due To Sacral Nerve Stimulation
There has long been the concern that activation of electrodes near peripheral nerves could cause neurologic damage. Recent advances in electrode design and surgical implant technique have enhanced the safety of long-term peripheral nerve stimulators. In animal experiments conducted in the 1970s, prolonged high-frequency stimulation was shown to be associated with early axonal degeneration. On biopsy this appeared as salt and pepper lesions, showing a mix of damaged and normal axonal fibers. The damaged fibers were generally large-caliber Aa- and Ab-type axons, innervating muscle spindles and carrying tactile and proprioceptive inputs .
Detection Of Cytokines Present In The Urine Of Ic/bps Patients With Or Without Hunner Lesions

Urine cytokines in the present study were detected using the mesoscale discovery U-plex assay: a highly sensitive electrochemiluminescence plate assay. Nine cytokines were selected for testing based on previous literature and their roles in the immune system: IFN-γ, TNF-α, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-12p70, and IL-13.
IL-6 is a key cytokine involved in B cell activation and the results from the cytokine assay indicated that patients with IC/BPS-HL, when compared to their age and sex matched IC/BPS-NHL counterparts, displayed significantly higher average urinary concentrations of IL-6 . A significant difference in average urinary IL-6 concentrations was not observed between the IC/BPS-HL population and UC population .
Urinary Cytokine concentrations in patients with Interstitial Cystitis/Bladder Pain Syndrome , and unaffected controls . Nine cytokines -1β, IL-2, IL-4, IL-6, IL-8, IL-12p70, IL-13, and Tumor Necrosis Factor-α) were assessed using a MSD U-plex 10 spot assay . Individual and average cytokine concentrations for A IL-6, B TNF-α, C IL-12p70, and D IL-13 from patients with Interstitial Cystitis/Bladder Pain Syndrome without Hunner Lesions , patients with Interstitial Cystitis/Bladder Pain Syndrome without Hunner Lesions , and UC research participants. Data are expressed as mean±SEM
Don’t Miss: Can A Bladder Infection Cause Bleeding
Neuromodulation & Nerve Stimulation For Ic/bps
Neuromodulation is Step Four in the AUA Treatment Guidelines for the treatment of interstitial cystitis. It uses a mild electrical impulse on various nerves to help maintain nerve function. Two different forms of neuromodulation are available, Urgent PC® and Interstim® . Both devices are approved for urinary frequency, urgency, incontinence and overactive bladder. Neither is approved for interstitial cystitis however they are frequently suggested for symptom management, hence their inclusion in the AUA Guidelines.
What Is The Outlook
You may need to try different treatments until you have relief of your symptoms. It is important to know that none of the treatments usually works right away. It can often take weeks to even months before you notice an improvement in your symptoms. Even with successful treatment, your IC/PBS may not be completely cured.
However, most patients can have significant relief of their symptoms and lead a normal life with the right treatment. You may find that you still experience some symptoms, however, and may find that you constantly have to pass urine more frequently. It is likely that you will always have to avoid certain types of food that have made your symptoms worse in the past.
You May Like: Cure A Bladder Infection In As Little As 6 Hours
Overlap With Other Chronic Pain Syndromes
Interstitial cystitis has also been associated with other poorly defined extra-pelvic pain syndromes that may involve neurogenic inflammation. In a large survey of patients with IC, there was a strong association with irritable bowel syndrome and high frequencies of atopia, fibromyalgia, and migraine headache . When Clauw et al. compared age-matched patients with fibromyalgia, IC, and healthy controls, a commonality of reported symptoms was seen between the groups with fibromyalgia and IC, leading the investigators to conclude that similar disorders in pain processing were present . Compared with normal controls, individuals with IC are 100 times more likely to have inflammatory bowel disease and 30 times more likely to have systemic lupus. In addition, allergies, irritable bowel syndrome, atopia, and fibromyalgia have an increased incidence among patients with IC .
Medtronic Bladder Control Therapy Delivered By The Nuro System
- Targets the tibial nerve to help you regain control of your bladder
- Does not cause unpleasant side eects like many oral medications can10
- Does not require self-catheterization, unlike injectable medications8
- Helps you live with less worry and more condence
The NURO system only treats the symptoms of OAB, not retention.
Most common side eects of PTNM are temporary and include mild pain or skin inammation at or near the stimulation site.
Don’t Miss: How Much Does A Bladder Scanner Cost
Who Gets Interstitial Cystitis
As many as 90% of people with IC are women. Somewhere between about 3% to 6% of adult women have some form of IC. Thatâs about 3 million to 8 million American women. About 1.3% of American men also have it.
On average, people first start having problems in their 40s. The risk of getting it goes up as you get older.
Sacral Nerve Stimulation Can Increase Bladder Control Decrease Pain
Very little is known about the mechanism of action of SNS despite numerous scientific investigations.
The majority of clinicians studying and practicing this therapy believe that the beneficial effect is brought about by modulating the reflexes involved in bladder function .
A major objective of the therapy is to ensure the patients sensation of a pulsating current in the perineal region .
Losing this sensation or shifting its location means the electrode has moved and is in the wrong place, which reduces the efficacy of the therapy. If this occurs, the electrode should be re-positioned. Once the electrode is properly and permanently implanted, the patient has the capability of controlling the stimulation parameters through a remote control device in order to ensure a persistent sensation.
With the patients input, the clinician can adjust the parameters of stimulation according to the patients needs. The therapy is geared to the life span of the internal battery of the pulse generator implanted under the skin which averages 5 – 7 years, depending on the usage. Once the battery stops functioning, the implant is surgically removed and replaced with a new one. If a patient ever wishes to cease the therapy, both electrode and battery can be surgically removed.
Please note: This information should not be used as a substitute for medical treatment and advice. Always consult a medical professional about any health-related questions or concerns.
Recommended Reading: How To Fix Bladder Leakage Naturally