What Happens After Bladder Surgery
The specifics of recovering from bladder surgery depend a lot upon the type of bladder surgery that you have. For example, in a transurethral resection much less tissue is removed or changed in the surgery than during a radical cystectomy where the entire bladder is removed. Thus, the recovery time after your procedure can vary. Your healthcare provider will help guide you through the recovery process including a voiding trial and catheter care instructions.
Not long after your surgery, youll need to get checked out again by your healthcare provider. Report any problems youve had since your procedure. If youve had bladder cancer, they might need to insert a camera into your bladder to check it.
Dont Miss: Pictures Of Prolapsed Uterus And Bladder
What Is The Colposuspension Procedure
This is a more invasive operation which requires a 45-60 minute procedure and a hospital stay of 3-4 nights. Longer recovery times and resulting scarring, much like a caesarean section scar, means this procedure is less common in modern times. A more popular treatment option now is the newer mid-urethral tape procedures, which have a shorter operating time, fast recovery and minimal scarring.
However, colposuspension may be recommended by a subspecialist urogynaecologist if a previous continence operation has failed.
Dietary Tips For Managing Constipation
Try to drink at least 4-6 glasses of fluid a day and increase your fibre intake from a wide variety of foods. Fibre is classified as either soluble or insoluble. Most plant foods contain a combination of both types of fibre. Insoluble fibre such as wheat bran, wholegrain breads and cereal helps increase the dry weight and ability of bowel motions to hold moisture. Soluble fibre such as in fruits, vegetables and legumes help to soften the poo and make it easier to pass.
Processed foods such as biscuits, cakes, pastries and fast foods are generally low in fibre and will contribute to constipation. Fruit and vegetable juice contain little fibre and are not a good substitute for whole fruit and vegetables.
Read Also: Why Do I Keep Getting Bladder Infections
How Is It Treated
Children with true fecal incontinence lack the ability to voluntarily have a bowel movement, so they require daily interventions to empty the colon of stool. However, there are two different types of true fecal incontinence and treatment for each varies:
- Children with a slow colon with constipation. This group represents the majority of children with true fecal incontinence. These are patients typically have:
- Hirschsprung disease
- Spinal disorders
They will require a daily enema that cleans the colon , but many children wont need a special diet or medicines.
- Children with a fast colon and loose stools. Loose stools can be a problem with some children who have had anorectal surgery and can also occur in some patients with Hirchsprung disease. In addition to a daily enema, these children will also need a constipating diet, and medicine to slow the colon.
Physicians are usually able to predict which children with these issues will go on to have fecal incontinence so that parents can set expectations for potty training. In some cases, parents are asked to try typical potty training around the age of three. If that isnt successful, the child can begin a bowel training bootcamp. Potty training can be tried again during vacation or summer breaks to assess bowel control. As a child with true fecal incontinence ages, they typically become more engaged with managing their condition.
Treatments For Bowel Incontinence
Treatment can help improve bowel incontinence and reduce the impact it has on your life. The best treatment for you depends on what’s causing the problem.
Treatments for bowel incontinence include:
- incontinence products such as pads you wear in your underwear or small plugs you put in your bottom
- changes to your diet such as avoiding foods that make diarrhoea worse
- medicines to reduce constipation or diarrhoea
- pelvic floor exercises to strengthen the muscles used to control your bowels
Surgery may be considered if other treatments do not help.
Recommended Reading: Best Dog Food To Prevent Bladder Stones
Incontinence And Continence Problems Are Common
Incontinence and continence problems affect people of all ages, gender, cultures and backgrounds. Despite popular beliefs, older people are not the only ones affected.Some incontinence facts include:
- One in three women who have had a baby experience loss of bladder control.
- One in five children wet the bed at some time.
- One in 100 adults never achieve bladder control at night.
- One in 20 adults experience bladder and bowel control problems.
Bladder and bowel control problems are not an inevitable part of ageing. Visit your doctor to discuss treatment and management options.
What Does Incontinent Mean
Incontinent in an adjective used to describe a person who suffers from bowel or bladder control problems. There are a number of possible reasons why a person may have incontinence. Muscle weakness, hormonal imbalances, prostate problems, infections, medications, obesity and medical conditions can all cause incontinence.
Read Also: What Vitamins Are Good For Bladder Health
Read Also: Spinal Cord Injury Bladder Training
When To Get Medical Advice
See a GP if you have difficulty controlling your bowels. Do not be embarrassed about talking to someone about it.
Remember that:
- it’s not something to be ashamed of
- it’s common and GPs are used to seeing people with it
- it’s not something you have to put up with
- it will probably not get better on its own
- it can be treated
If you’d prefer not to see a GP, you may be able to make an appointment at an NHS continence service instead. Call your local hospital for details of your nearest service.
Medications For Overactive Bladder
Drugs used to treat OAB block the abnormal contractions of the bladder muscle and can therefore also help ease the symptoms of urge urinary incontinence in both men and women. Youll find a list of OAB medications available in Canada on page 20. Generally speaking, these drugs fall into three categories:
Anticholinergics
Anticholinergic medications block the action of acetylcholine, a chemical messenger that tells the muscles of the bladder wall to contract. Unfortunately, acetylcholine acts in other parts of the body as well, so medications that block it can cause unwanted side effects like dry mouth, blurred vision, impaired cognition and constipation. New extended or prolonged release versions of anticholinergic medications reduce the incidence of side effects and improve compliance because they only need to be taken once a day to produce a steady absorption rate and constant blood levels of the drug.
Dont Miss: Bladder Cancer After Prostate Radiation
Don’t Miss: Bcg Used In Bladder Cancer
Is Snm Therapy Effective At Treating Urinary And Bowel Incontinence
GI Associates & Endoscopy Center proudly offers sacral neuromodulation as an effective, safe, and long-lasting approach to treating bladder or fecal incontinence in Jackson, MS individuals. SNM is clinically proven to treat urinary incontinence, urinary retention, OAB, and fecal incontinence. Studies performed show that sacral neuromodulation therapy produces a high rate of patient satisfaction and treatment success for both urinary and bowel incontinence concerns, and also has a very high safety profile. It has proven successful in adults for whom a conservative approach to therapy was ineffective, can allow for significant quality of life enhancements, and is linked to considerably lower rates of incontinence events.
How Do I Know If I Have Incontinence
If youre not sure, its best to talk to your doctor first. However, we do have a few questions you can ask yourself to decide if incontinence may be affecting you.
Do you ever:
- Accidentally soil your underwear or pants with urine or feces without being able to hold it back and control when its time to go?
- Experience leakage of feces or bed-wetting at night ?
- Leak when you exercise, cough, sneeze, or laugh?
- Stay nervous or experience social anxiety because youre afraid of having another accident?
- Stay home and avoid social activities so you can be near your own bathroom in case of an urgent need to use the bathroom or fear of losing control of your bowels or bladder?
If you answered yes to any one of these questions, you may have urinary incontinence or fecal incontinence.
Next, we suggest talking to your doctor because theyre the best source for diagnosing and treating this situation.
Recommended Reading: Drugs Used To Treat Overactive Bladder
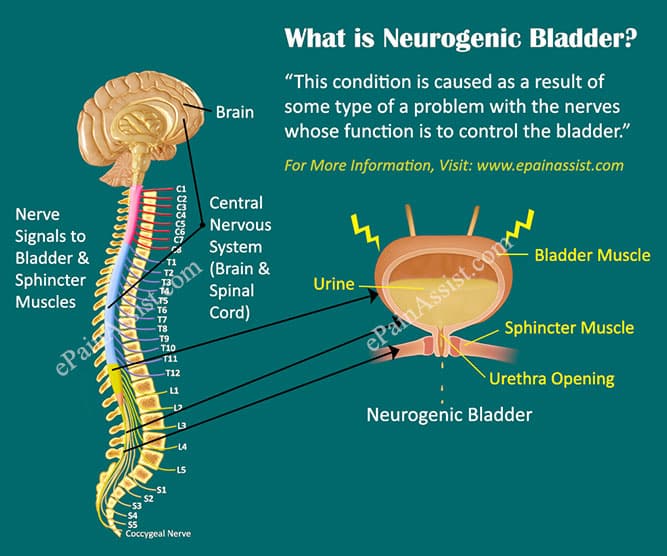
How Does Interstim Therapy Work
InterStim therapy works by stimulating the sacral nerves with tiny electrical pulses. In individuals experiencing urinary or fecal incontinence, the brain and the sacral nerves are unable to communicate properly. InterStim therapy attempts to better regulate the sacral nerves function, so the nerves can interpret signals from the brain and pass them on to the surrounding pelvic floor muscles. Mild electrical pulses help the nerves to function normally, much in the same way that a pacemaker uses electrical impulses to keep the heart beating on a steady, predictable rhythm. This restores normal bladder and bowel function.
As a result of the pulses from InterStim devices, the symptoms of an overactive bladder or bowel incontinence are effectively eliminated.
These devices are an option for patients who have not responded to more conservative treatments such as changes to diet, medication and physical therapy.
Bladder Incontinence In Women
Bladder incontinence is more common in women than in men. Other than the possible causes listed above, some things that may increase risk of bladder incontinence in women are:
- Changes to urinary or vaginal tissue from hormone therapy, surgery, chemotherapy, or targeted therapy
- Hormonal changes from menopause
- Pelvic prolapse – the bladder, uterus, and or rectum may slip backward or downward into the vaginal canal because of weak pelvic wall muscles
Recommended Reading: Bladder Cancer Treatment With Tuberculosis Bacteria
Types Of Bladder Control Problems
Urinary incontinence and continence problems may include:
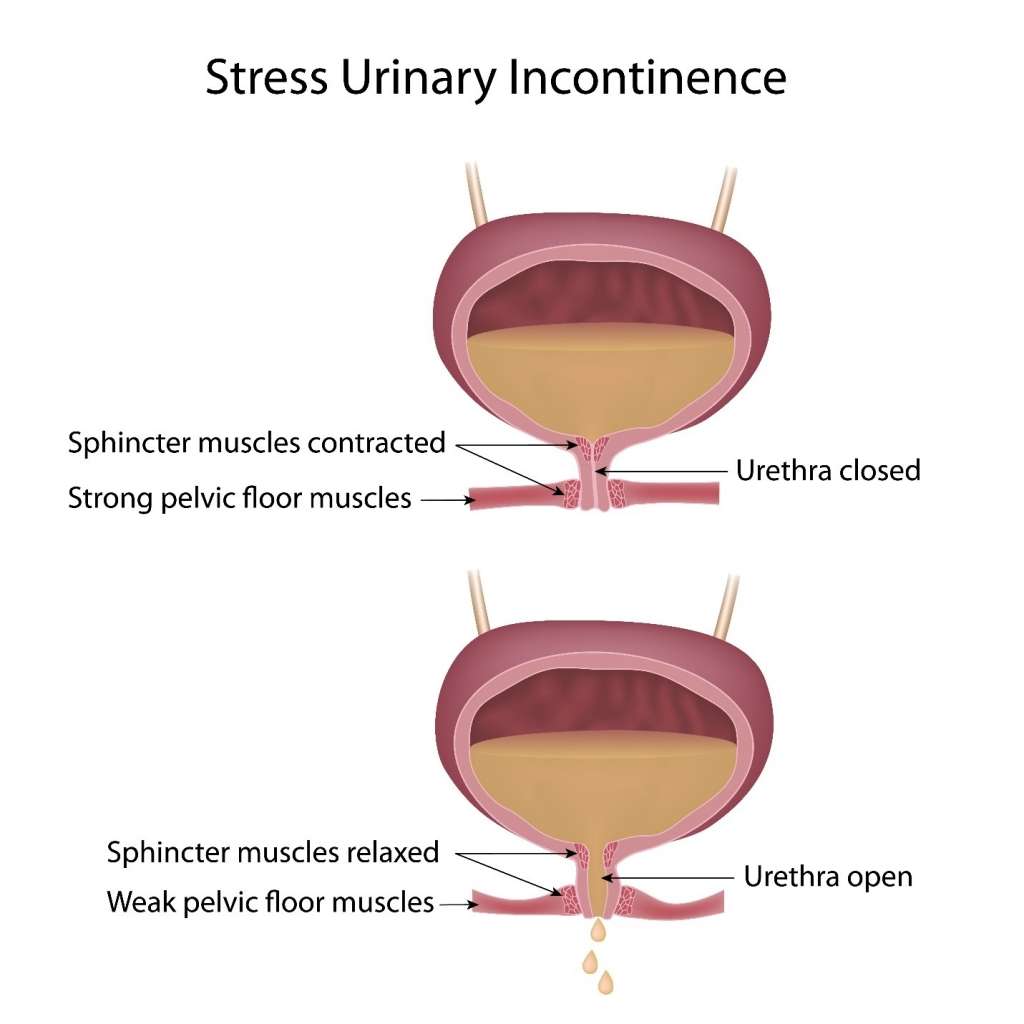
- stress incontinence leakage of small amounts of urine with exertion. Causes include childbirth, being overweight and prostate surgery
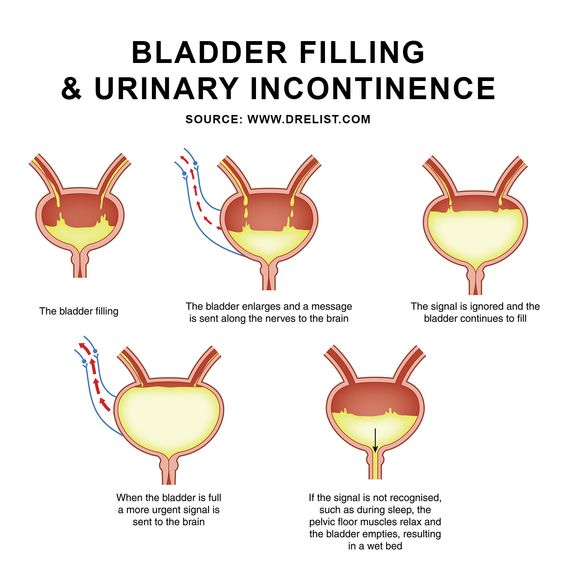
- urge incontinence leakage following a sudden urge to urinate. Causes include stroke, enlarged prostate gland and Parkinsons disease, but often the cause is unknown
- overflow incontinence leakage because the bladder does not empty well and overfills. Causes include multiple sclerosis, an enlarged prostate gland and diabetes
- functional incontinence leakage of urine because a person was unable to get to or use the toilet due to a physical disability, a barrier in their environment or because of an intellectual or memory problem. Causes include dementia and poor mobility.
Why Is Bladder Suspension Surgery Done
Bladder suspension surgery is a procedure that can be used to treat urine leakage that occurs when a person sneezes, laughs, or coughs a condition called stress incontinence. Childbirth, as well as hormonal changes that come with menopause, can cause a woman to lose muscle tone along the pelvic floor. That can lead to stress incontinence.
Recommended Reading: What Happens When A Bladder Infection Goes Untreated
Behavioral And Lifestyle Changes
Changing your lifestyle may help with bladder problems. Losing weight, quitting smoking, saying no to alcohol, choosing water instead of other drinks, and limiting drinks before bedtime can help with some bladder problems. Preventing constipation and avoiding lifting heavy objects may also help with incontinence. Even after treatment, some people still leak urine from time to time. There are bladder control products and other solutions, including disposable briefs or underwear, furniture pads, and urine deodorizing pills that may help.
Visit the National Institute of Diabetes and Digestive and Kidney Diseases for more information on urinary incontinence in men and urinary incontinence in women.
Interstim Therapy Trial Period
InterStim II and InterStim Micro offer a trial device that simulates the actual, implanted device. This is called InterStim Stage 1. Receiving the trial device is a 15-minute, minimally invasive outpatient procedure where the doctor places a lead connected to a small, externally worn device. The external device is worn underneath the patients clothing.
Patients typically wear the trial device between 5-14 days to determine candidacy for a permanent device. During this time, patients log their symptoms to discuss with their doctors. They can continue about their normal activities and experience what it would be like to live with InterStim therapy, how it feels when activated, and if the permanent device will be able to reduce or eliminate their symptoms.
You May Like: Can Sitting Too Much Cause Bladder Problems
Psychosocial Burden And Association With Behavioural And Neuropsychiatric Disorders
The social stigma of persistent wetting and bowel accidents is a common problem faced by children with BBD and can lead to self-esteem issues, shame, isolation, poor school performance, aggressiveness, and other behavioural changes. In cases of intractable BBD, the involvement of a psychologist or psychiatrist must be considered. The relationship between bladder dysfunction and neuropsychiatric disorders is well-documented. Mental illness does increase the risk of both bowel and bladder incontinence. The mental condition may interfere with the child/teenagers ability to reach the toilet on time because of disorganized thinking, confusion, or inattention. More importantly, medications used to treat anxiety or obsessive compulsive disorders can directly affect the bladder and bowel, making the person less aware of the need to void.
Frequently Asked Questions Expand All
- What is stress urinary incontinence ?
Stress urinary incontinence is the leakage of urine with physical activity, such as exercise, or when coughing, laughing, or sneezing. It is a common problem in women. SUI can be treated with both nonsurgical and surgical treatment methods.
- What causes SUI?
SUI is a pelvic floor disorder. These disorders occur when tissues and muscles that support the urethra, bladder, uterus, or rectum are damaged.
In SUI, the sphincter muscle that controls the flow of urine from the bladder to the urethra may weaken. Or the muscles that support the position of the bladder and the urethra may weaken. Weakness in these muscles may occur from pregnancy, childbirth, or aging.
- What nonsurgical treatments may help with SUI?
If you have SUI and your symptoms bother you, your health care professional may suggest nonsurgical treatments first. Lifestyle changes, such as drinking less fluid, limiting caffeine, stopping smoking, and losing weight, can help decrease the number of times you leak urine.
Other nonsurgical options include pelvic muscle exercises , physical therapy and biofeedback, or use of a pessary. Another option is an over-the-counter product that is inserted into the like a tampon. If these treatments do not improve the problem, surgery may help.
- What are the surgical treatments for SUI?
Surgery improves SUI symptoms in most women. There are different types of surgery for SUI:
-
Colposuspension
Don’t Miss: How Do You Diagnose Overactive Bladder
Better Bladder And Bowel Control: Practical Strategies For Managing Incontinence
Most people take bladder and bowel control for granted until something goes wrong. An estimated 32 million Americans have incontinence, the unintended loss of urine or feces that is significant enough to make it difficult for them to maintain good hygiene and carry on ordinary social and work lives. The good news is that treatments are becoming more effective and less invasive. This Special Health Report, Better Bladder and Bowel Control, describes the causes of urinary and bowel incontinence, and treatments tailored to the specific cause.
What Is Overactive Bladder
Overactive bladder is a group of urinary symptoms with the most common being an extreme urge to urinate thats challenging to control. You may not be able to stop the urge, which may lead to involuntary urine loss. Other overactive bladder symptoms include frequent urination during the day, the need to get up frequently to urinate at night and leakage when there is an urge to urinate.
You May Like: Bladder Feels Full All The Time
Living With Bowel Or Bladder Incontinence
There is no single, right way to cope with bladder or bowel incontinence. The challenge is to find what is best for your situation, so you can get the help you need and return to a normal daily life. Talk with your health care team if you notice a change in bowel or bladder habits, and about the best ways to manage incontinence, if it is a problem. You might find it helpful to talk with other people who are dealing with incontinence, too. Ask a member of your cancer care team about support groups in your area.
Here are some things you can do that may help make incontinence less of a problem:
- Empty your bladder every 3 to 4 hours while awake, to avoid accidents.
- Empty your bladder before bedtime or before strenuous activity.
- Limit drinks with caffeine, or and avoid alcohol and citrus juices, which can irritate the bladder and make you have to go more often.
- Avoid hygiene products that may irritate you Women should avoid feminine spray or over-the-counter vaginal suppositories.
- Because belly fat can push on the bladder, avoiding weight gain or losing needed weight sometimes helps improve bladder control.
- Avoid tobacco use which can cause coughing and bladder irritation due to harmful substances in tobacco products.
- Talk to your doctor about all medicines, vitamins, herbs, and supplements youre taking. Some may affect urine control.
What To Expect During A Surgical Bladder Suspension
A bladder suspension procedure is typically performed in a hospital setting under general or spinal anesthesia. Depending upon how much bladder support is needed, your doctor will determine the type of procedure that will be used.
Surgical options include:
- Open retropubic suspension surgeryDuring an open procedure, your doctor will make a large incision in the abdomen to access the bladder. Once the area is open, your doctor will locate the bladder and urethra, pull the bladder neck up and sew it into the nearby bone or tissue.
- Laparoscopic retropubic suspensionDuring a laparoscopic procedure, your doctor will make two to three smaller incisions into the abdomen and above the pubic bone. Small surgical instruments will be used to perform the procedure. Although laparoscopic retropubic suspension allows for a quicker recovery and shorter hospital stay, results show higher complication rate.
- Transvaginal procedureDuring a transvaginal bladder suspension, a small incision is made in the front of the vaginal wall to access the bladder and urethra. Once accessed, your surgeon will lift the bladder neck and sew it into the surrounding bone or tissue.
- Sling surgeryDuring a sling surgery procedure, your doctor will create a hammock-like structure that will cradle the bulging bladder. The sling will support the bladder and urethra to help relieve the symptoms of stress incontinence. In many cases, your doctor can use your own tissue from your abdominal wall or use donor tissue.
Read Also: Va Decision On Agent Orange And Bladder Cancer