Does Incontinence Affect Your Sexuality
The good news is that a recent study tells us women with incontinence or prolapse report the same amount of sexual activity, comfort, and enjoyment with sex as women without incontinence. There’s more: 80% of the women with either prolapse or incontinence felt their partners were also satisfied with their sexual relationship. Naturally the woman’s feeling about her partner and the relationship has a lot to do with whether she is satisfied sexually or otherwise. But the incontinence and the prolapse turned out to be less important than expected. Incontinent or not, many women stay sexually active well into their seventies and eighties.
However, the same study stated that women with the most severe prolapse or most frequent incontinence did report that their physical condition interfered with their sex lives. As a result, these women were more distressed about their medical situations and were less content. While the women with less severe incontinence did not have a significant problem with sexual satisfaction, those with severe problems found it was a detriment to their sex lives.
Women With Previous Hysterectomy
Laparoscopic Sacrocolpopexy
This is the most common operation performed with access from the abdomen for women who do not have the uterus and present with apical prolapse or prolapse of the top part of the vagina.
After entering the abdomen through small laparoscopic incisions and inserting a camera to be able to see inside the abdomen and pelvis, the surgeon dissects the vagina from the bladder anteriorly and the rectum posteriorly.
A graft fashioned in a Y shape is then sutured to the anterior and posterior aspects of the vagina.
The surgeon then opens the membrane that covers the sacral bone and exposed the promontory which is the uppermost part of the sacrum below the lumbar spine. The graft is the sutured to ligaments over the bone providing support and aiming to bring the top of the vagina to its natural elevated position.
Before Choosing Surgeryexpand All
There is no guarantee that any treatmentincluding surgerywill relieve all of your symptoms. Also, new problems may occur after surgery, such as pain during sexual intercourse, pelvic pain, or urinary incontinence.
More than one type of surgery may be done at the same time to fix multiple problems.
Surgery done through the vagina may take less time to perform than surgery done through an incision in the abdomen. The recovery time is usually shorter.
Surgery done with an abdominal incision may result in less pain during sex than after procedures done through the vagina. But with an abdominal incision, there is a risk of damage to the intestines and a risk of complications from adhesions.
After surgery with mesh placed in the abdomen, there is a small risk that the mesh will erode into the vagina. Mesh erosion can cause scarring and pain that can be long-lasting. Additional surgery may be needed to remove the mesh.
If you are considering a surgery using vaginally placed mesh, ask your health care professional for detailed information about its risks, benefits, and potential complications. POP can be treated successfully without mesh in many cases.
When considering surgery for POP, it is important to weigh your options. Talk with your health care professional about which option is best for your situation.
Article continues below
Recommended Reading: Can Yeast Infection Cause Overactive Bladder
Degrees Of Uterine Prolapse
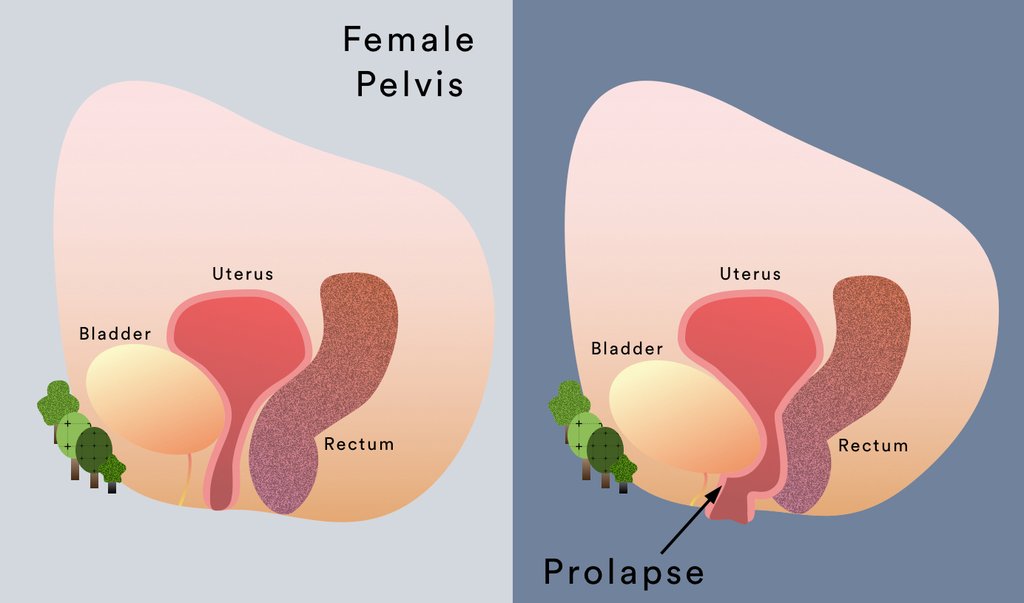
Uterine prolapse is described in stages, indicating how far it has descended. Other pelvic organs may also be prolapsed into the vagina.,. The four categories of uterine prolapse are:
- Stage I the uterus is in the upper half of the vagina
- Stage II the uterus has descended nearly to the opening of the vagina
- Stage III the uterus protrudes out of the vagina
- Stage IV the uterus is completely out of the vagina.
Will Sex Be Better If You Have Surgery
To answer this, a recent American study questioned a group of women before and after surgery to repair a prolapse or incontinence. About half of these women were sexually active. Before surgery, 82% of the sexually active women reported being happy with their sex lives, and after surgery, 89% of the women felt happy with their sexual relationship.
However, a study brought out a number of interesting findings. For one, the frequency of intercourse did not change following surgery. And two, while only 8% of the women had pain with intercourse before surgery, 19% noted pain with intercourse after surgery. About one quarter of the women who had a repair of a bulging rectum developed pain with intercourse. About one third of the women who had repair of a rectocele and a bladder suspension had painful intercourse. Unfortunately, the researchers did not ask these women why they were more satisfied with their sex lives even though more of them had painful intercourse.
Another study performed in Sweden may shed some light. This study found that one third of women noted an increased interest in sex after incontinence surgery, and one half of their male partners were more interested in sex. It could be that knowing the repair for the prolapse or incontinence had been addressed was enough to make the couples feel better about sex.
Don’t Miss: Low Grade Bladder Cancer Recurrence
Can Prolapse Be Treated With Surgery
While prolapse never leads to serious medical illness, it can make some womenâs lives uncomfortable or even miserable. Surgical repair of prolapse can be performed through abdominal incisions, incisions high up inside the vagina or, more recently, through small incisions in the navel and lower abdomen through which a laparoscope and small instruments are placed. It is common for more than one supporting structure of the pelvis to develop weakness or tears, so itâs not uncommon to find more than one area is in need of repair. The surgical repair of prolapse is undergoing a re-evaluation. MRI has recently been used to better define the specific areas of damage to muscles and supporting tissues that often lead to prolapse and incontinence.
Also Check: Bladder Infection And Back Pain
What Happens During Vaginal Prolapse Surgery
Vaginal prolapse surgery is usually performed under general anaesthetic. In some cases, it can be performed as laparoscopic surgery. The length of the procedure will depend on the extent of your prolapse.
Your consultant will make incisions inside your vagina and strengthen the supporting tissues with stitches. They may make repairs to both the back and front vaginal walls. Additional supporting stitches may be needed at the top of your vagina or into your cervix. In some cases, surgical mesh may be used. Any wounds will be closed using dissolvable staples.
At the end of your procedure, they may insert a catheter into your bladder to drain urine and your vagina may be packed with material to prevent bleeding. These will be removed in 1-2 days.
You may need to stay in hospital for 3-5 days. Be sure and let a member of our healthcare team know if you are in any pain. You will be able to go home once you are able to move about confidently and you can pass urine with no problem.
Recommended Reading: When To See A Doctor For A Bladder Infection
Frequently Asked Questions Expand All
- What are the pelvic organs?
The pelvic organs include the vagina, uterus, bladder, urethra, and rectum. These organs are held in place by muscles of the pelvic floor. Layers of connective tissue also give support.
- What is pelvic organ prolapse?
Pelvic organ prolapse occurs when tissue and muscles can no longer support the pelvic organs and they drop down .
- What are the different types of pelvic organ prolapse?
There are several types of prolapse that have different names depending on the part of the body that has dropped.
-
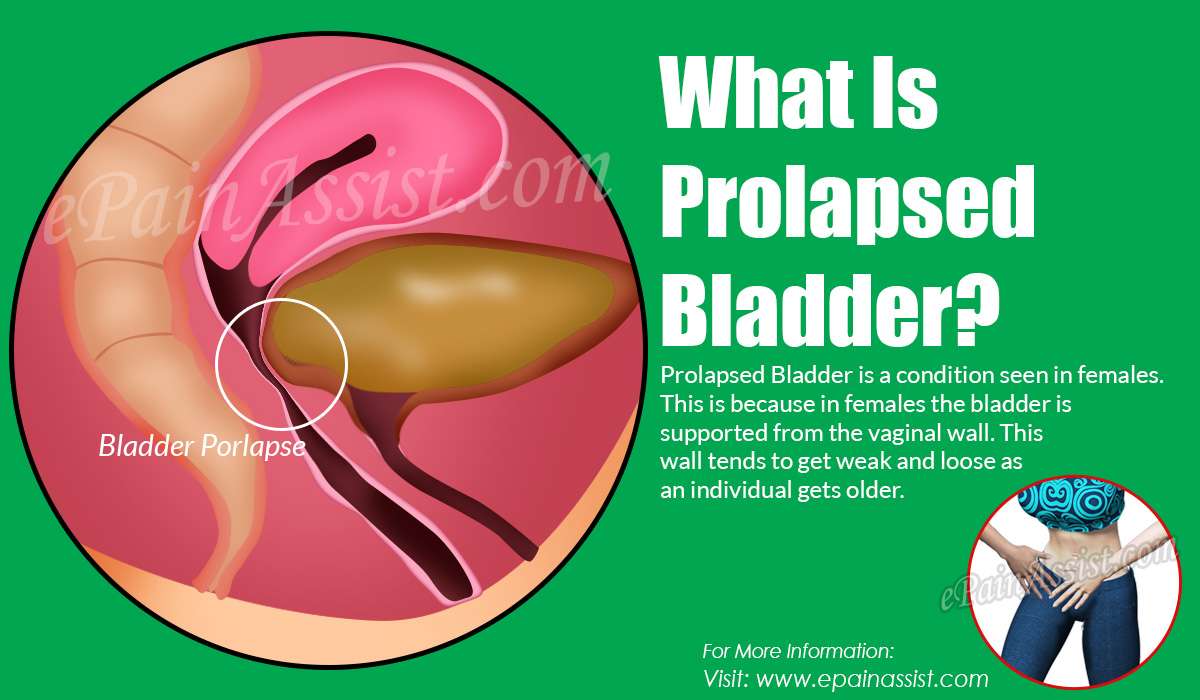
Cystocele. The bladder drops into the vagina.
-
Enterocele. The small intestine bulges into the vagina.
-
Rectocele. The rectum bulges into the vagina.
-
Uterine Prolapse. The uterus drops into the vagina.
-
Vaginal Vault Prolapse. The top of the vagina loses its support and drops.
Symptoms of POP can come on gradually and may not be noticed at first. A health care professional may discover a prolapse during a physical exam. Women with symptoms experience the following:
Feeling of pelvic pressure or fullness
Bulge in the vagina
Will I Need Any Investigations For Pelvic Organ Prolapse
For most women, examination alone is enough to make a diagnosis. If you have any urinary symptoms, as described above, your doctor may ask you to collect a specimen of urine to be sent off to the laboratory to check for signs of infection. They may also suggest that you have a blood test to check your kidney function. They may refer you to a specialist for some more detailed tests on your urine and bladder – for example, some tests known as urodynamic studies. These are tests of your urine flow and they are usually done in a hospital unit. If you have bowel symptoms, a specialist may suggest some special tests to look into these. Occasionally further tests, such as an ultrasound scan, are used.
Recommended Reading: Tens Unit For Overactive Bladder
What To Know Before Doing Kegels
Its harder to find your pelvic floor muscles than, say, your biceps, because they dont show.
- The pelvic floor muscles wrap around and support the uterus, bladder, and bowel.
- To find them, pretend you need to stop peeing in midstream and avoid passing gas at the same time. Thats your pelvic muscles in action.
- When performing Kegels, its important not to hold your breath or squeeze your stomach, thighs, or buttocks.
- Youll feel more comfortable, and avoid dripping urine, if you empty your bladder first.
- Once you get the hang of it, Kegels are simple to do, and they can easily become a habit.
Prolapse Affecting The Front Part Of The Pelvis
- There can be prolapse of the urethra into the vagina. The medical term for this is a urethrocele.
- There can be prolapse of the bladder into the vagina. The medical term for this is a cystocele.
- Or, both the urethra and the bladder can prolapse into the vagina at the same time. The medical term for this is a cystourethrocele. This is the most common type of pelvic organ prolapse.
Read Also: How Long Does It Take For Bladder Cancer To Spread
Side Effects Of Surgery
Your doctor should have an in-depth discussion with you about the risks and benefits of the 4 different types of surgery, including mesh surgery, before you decide together whether one of them could be an option.
Doctors must also keep detailed records about the type of surgery they do, including any complications you get after you have had your surgery.
You should be given a copy of this record.
Possible side effects of all 4 types of surgery, including mesh surgery, include:
- bleeding, which may require a blood transfusion
- damage to the surrounding organs, such as your bladder or bowel
- an infection â you may be given antibiotics to take during and after surgery to reduce the risk
- changes to your sex life, such as discomfort during intercourse â but this should improve over time
- vaginal discharge and bleeding
- experiencing more prolapse symptoms, which may require further surgery
- a blood clot forming in 1 of your veins, such as in your leg â you may be given medicine to help reduce this risk after surgery
If you have any of the following symptoms after your surgery, let your surgeon or a GP know as soon as possible:
- a high temperature
What Else Can Help Prevent Leaking During Sex
Another way to prevent leaking during sex is to keep your bladder reasonably empty during intercourse. Try to avoid drinking fluids for an hour or so before you expect to have intercourse. This will keep the bladder from filling up too quickly once you get into bed. If you empty your bladder just before you begin lovemaking, leaking is much less likely.
Read Also: Where Do You Feel Bladder Pain
Causes Of A Prolapsed Uterus
The cause of uterine prolapse is the weakening of the pelvic muscles. If they are not strong enough, they cant hold the uterus in place, and it drops down into the vagina. Specific causes can include:
- Multiple pregnancies and vaginal deliveries
- Constipation paired with regular straining to pass stool
- Chronic cough
Laparoscopic Pelvic Organ Prolapse Surgery
Laparoscopic pelvic organ prolapse surgery is a minimally invasive procedure used to treat pelvic organ prolapse, a condition in which the pelvic organs drop down and press against the vagina, causing a bulge or protrusion.
Pelvic organ prolapse surgery is used to restore the normal structure and function of these pelvic organs, relieving symptoms that include pain, discomfort, pressure, and urinary and bowel dysfunction.
Laparoscopic pelvic organ prolapse surgery uses very small, specialized surgical instruments inserted through tiny incisions in the abdomen, allowing the surgeon to see and operate on the pelvic organs without having to use a long incision.
This minimally invasive approach offers several advantages over a vaginal approach or traditional open surgery, including:
- Shorter hospital stays
- Faster recovery and return to normal activities
- Fewer complications
- Better view of the pelvic organs and support defects during surgery
- Better suspension of the vagina, through greater visibility and access
- Lower risk of recurrence
Recommended Reading: What Is The Best Medicine For Bladder Control
Surgical Treatment Of Pelvic Organ Prolapse
The most common symptom of pelvic prolapse is constipation, but others include painful intercourse, bleeding from the vagina, incontinence, pelvic pressure, and pain in the groin or lower back. If symptoms are severe, or if prolapse interferes with the urinary or reproductive systems, surgery may be needed to correct the problem. Surgical treatments for pelvic prolapse include:
Who Gets Uterine Prolapse
Uterine prolapse is most likely to happen in women who:
- Have had one or more vaginal deliveries.
- Are post-menopausal.
- Have family members who have had prolapse.
Menopause occurs when your ovaries stop producing the hormones that regulate your monthly menstrual cycle . When you havent had a period for 12 straight months, you are considered menopausal. One of the hormones that stops during menopause is estrogen. This particular hormone helps keep your pelvic muscles strong. Without it, you are at a higher risk of developing a prolapse.
Donât Miss: Ways To Help Overactive Bladder
Recommended Reading: Will A Bladder Infection Go Away On Its Own
Diagnosis For A Prolapsed Uterus
To diagnose a prolapsed uterus, your doctor will perform a vaginal exam. They may ask you to bear down as though you are pushing out a bowel movement. They will look to see how much tissue is prolapsed into or out of the vagina.
After examination, your doctor will determine your degree of prolapse, giving it a grade from 1 to 4. A grade of 1 means that the uterus has descended into the upper vagina. A grade of 4 means that the uterus and the cervix have exited the vagina.
What You Need To Know
- When pelvic muscle, tissue and ligaments weaken, the uterus can drop down into the vaginal canal, causing uterine prolapse.
- Nearly one-half of all women between ages 50 and 79 have some degree of uterine or vaginal vault prolapse, or some other form of pelvic organ prolapse.
- Factors that increase your risk of uterine prolapse include childbirth, age, obesity, chronic constipation and having a hysterectomy.
- Many women with uterine prolapse have no symptoms. If symptoms are present, they may include bulging in the vagina, feeling pressure in the pelvis or vagina, and lower back pain accompanied by bulging in the vagina.
- There is no definitive way to prevent uterine prolapse. Losing weight, eating a fiber-rich diet, quitting smoking and performing pelvic floor exercises can help to reduce the risk of this condition.
Also Check: Can A Prolapsed Bladder Cause Lower Back Pain
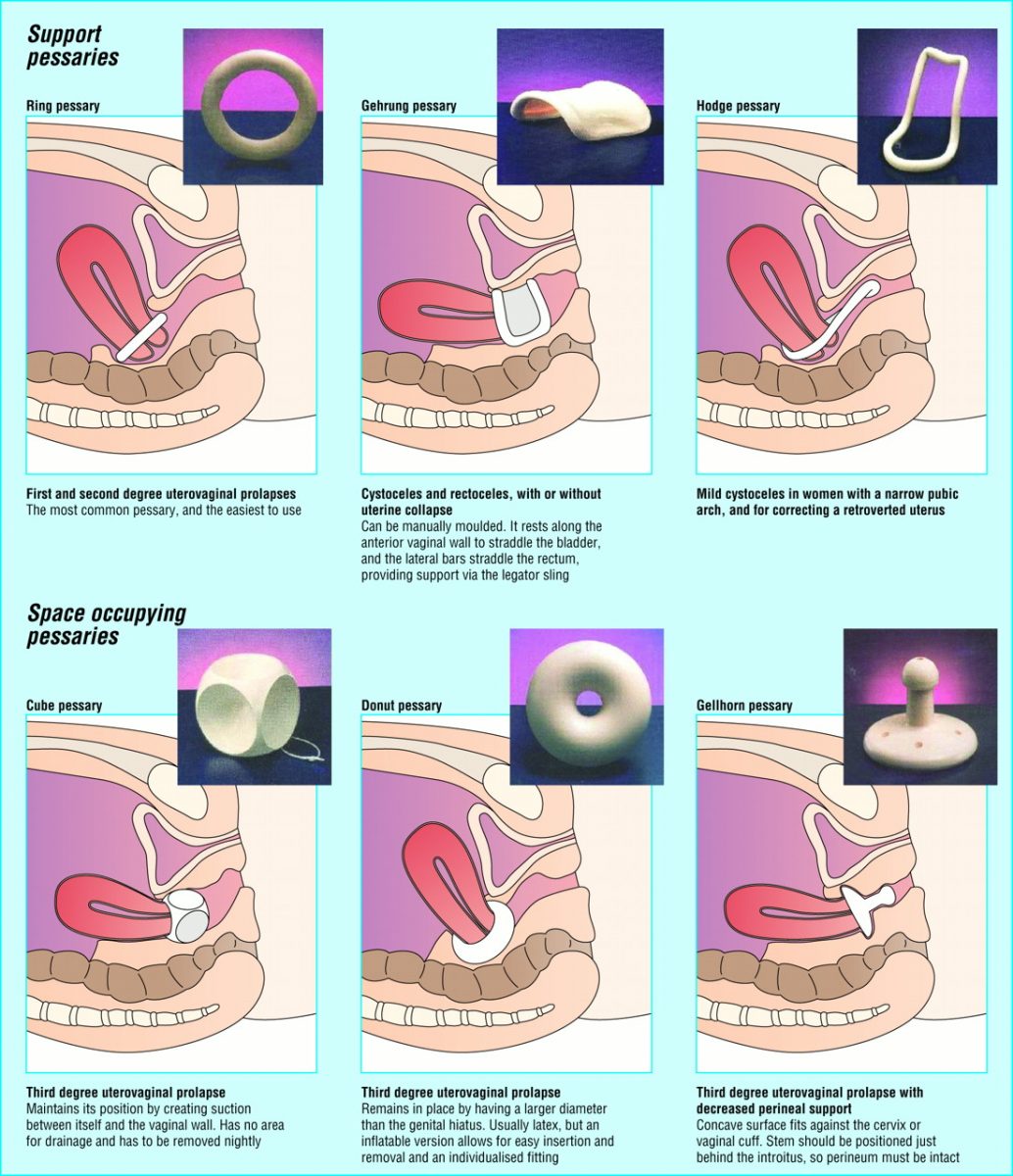
Treatment Of Vaginal Prolapse
In patients with a mild cystocele, treatment using a ring with support, a dish with support, a Hodge with support or a donut pessary will suffice. To manage a large prolapse of the anterior vaginal wall, the Gellhorn pessary may be the best choice, although insertion and removal can be difficult. Inflatable and cube pessaries are also useful in patients with a larger cystocele. In patients with rectoceles and enteroceles, the use of a Gellhorn, donut, inflatable or cube pessary is usually required to provide the necessary support.
Treatments For A Prolapsed Uterus
To diagnose a prolapsed uterus, your doctor will perform a vaginal exam. They may ask you to bear down as though you are pushing out a bowel movement. They will look to see how much tissue is prolapsed into or out of the vagina.
After examination, your doctor will determine your degree of prolapse, giving it a grade from 1 to 4. A grade of 1 means that the uterus has descended into the upper vagina. A grade of 4 means that the uterus and the cervix have exited the vagina.
Treatments for a prolapsed uterus
There are a variety of treatment options for a prolapsed uterus. What works for you may depend on your lifestyle, preferences, and medical history. You may not need medical treatment if your symptoms are mild or not causing you discomfort.
Medications
A pessary is a device inserted into the vagina to help hold the uterus in place. They come in different shapes and sizes to help women with varying severities and types of prolapses. Your doctor can show you how to insert and remove a pessary as needed. A combination of pessary and pelvic floor exercises may help women with uterine prolapse avoid surgery.
Home care
Doctors often recommend pelvic floor exercises for minor cases of a prolapsed uterus. You should work with a physical therapist who focuses on strengthening the pelvic floor. They will give you exercises that can help to strengthen the pelvic muscles so they can hold the uterus in its proper place again.
Surgery
Read Also: Harmony Urinary Tract And Bladder Support