Who Performs Incontinence Sling Surgery For Women
The following specialists perform incontinence sling surgery:
-
Obstetrician-gynecologists specialize in womens health and pregnancy.
-
Urologists specialize in diseases and conditions of the urinary tract and the male reproductive organs.
-
Female pelvic medicine and reconstructive surgeons are urologists or gynecologists who have completed specialized training in womens pelvic floor disorders. Another name for this specialty is urogynecology.
What Happens After The Male Sling Procedure
Following your surgery, you may have a catheter exiting from the urethra for a short period of time. The catheter is in place to allow you to empty your bladder since there may be swelling after surgery that makes it difficult to urinate. After the swelling goes down, you will gradually be able to urinate on your own and empty your bladder well. However, your normal pattern of urination may not return for a few weeks. You can resume a normal diet after surgery.
What To Expect The Day Of Your Incontinence Sling Surgery
The day of your surgery, you can generally expect to:
-
Talk with a preoperative nurse. The nurse will perform an exam and ensure that all needed tests are in order. The nurse can also answer questions and will make sure you understand and sign the surgical consent form.
-
Remove all clothing and jewelry and dress in a hospital gown. It is a good idea to leave all jewelry and valuables at home or with a family member. Your care team will give you blankets for modesty and warmth.
-
Talk with the anesthesiologist or nurse anesthetist about your medical history and the type of anesthesia you will receive.
-
A surgical team member will start an IV.
-
The anesthesiologist or nurse anesthetist will start your general or regional anesthesia. Your surgeon will perform local anesthesia.
-
A tube may be placed in your windpipe to protect and control breathing during general anesthesia. You will not feel or remember this or the surgery as they happen.
-
A team member will insert a catheter into your bladder to collect urine.
-
The surgical team will monitor your vital signs and other critical body functions. This occurs throughout the procedure and your recovery until you are alert, breathing effectively, and your vital signs are stable.
You May Like: Pictures Of Bladder Cancer Tumors
Constructing A Sling During Prolapse Surgery Drops Incontinence Risk
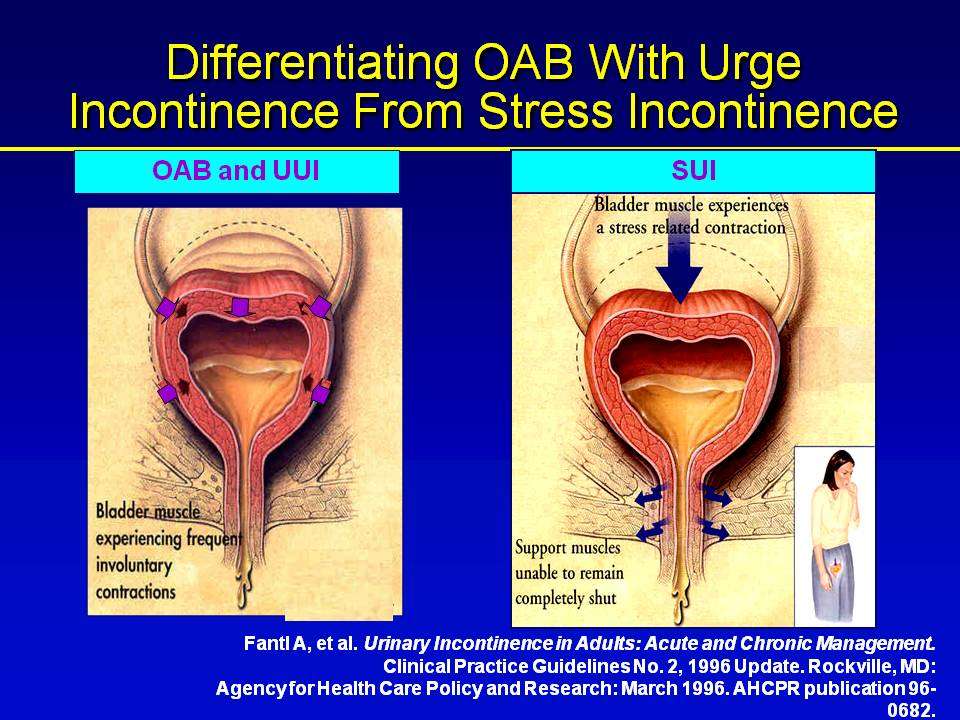
A midurethral sling during surgery to repair pelvic organ prolapse reduces the risk of developing stress incontinence, but also poses greater risks.
Research from the University of Alabama at Birmingham and other medical centers published in the June 21, 2012, New England Journal of Medicineshows that adding a midurethral sling to lift and support the urethra during surgery to repair pelvic organ prolapse reduces the chances of developing stress urinary incontinence. However, the procedure carries greater risk of complications than previous techniques.
Pelvic organ prolapse occurs when organs, such as the bladder or uterus, protrude through the pelvic wall due to weakened musculature and can cause stress urinary incontinence, the leakage of urine brought on by laughing, sneezing or running. It is fairly common, and often is caused by pregnancy or childbirth. According to the study, one in five women is a candidate for surgical repair of the condition.
Previous research looked at women who had abdominal repair for pelvic organ prolapse. Some women who did not have stress urinary incontinence also received a procedure called bladder-neck suspension to try to stave off incontinence in those women, the risk of developing stress urinary incontinence was significantly reduced.
At least a quarter of the women who have surgery for pelvic organ prolapse will develop incontinence as a result of the surgery, the study says.
Risks Of Bladder Sling Surgery
There are known risks associated with the mesh implants used in sling surgery. One of the main concerns is that pelvic meshes can break into fragments that embed into your tissue, become dislodged, and potentially perforate neighboring organs. When this happens, not only does the incontinence continue, but women experience intense pain and discomfort, often ending up worse than before the surgery. These complications frequently require followup surgeries to fix the mesh or even remove the device entirely.
In 2019, the FDA ordered a halt to the sale of transvaginal surgical mesh implants for certain pelvic procedures, and in many countries, pelvic meshes have been outlawed completely. Recently, in-depth media coverage and large class-action lawsuits have shed light on the dangers of bladder sling surgery. However, many women dont know about the alternative, nonsurgical treatment options.
Recommended Reading: Best Way To Treat Bladder Infection
You May Like: Hx Of Bladder Cancer Icd 10
How Is Bladder Sling Surgery Performed
There are many different types of sling procedures used to treat stress urinary incontinence .
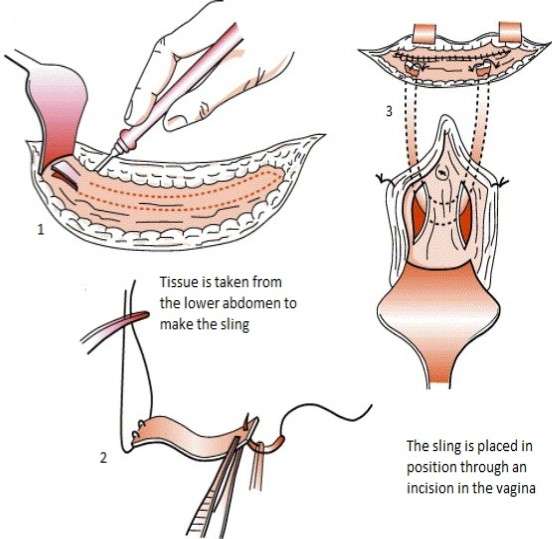
During the most common sling procedure, your surgeon will take a strip of your body tissue, either from your stomach or your thigh to make the sling. Slings might also be made from donor tissue or plastic material that is compatible with body tissues. Then they make a small cut between the scrotum and anus and put the sling around part of the urethral bulb .
As it heals the scar tissue forms around it to hold the sling in its place. The sling will squeeze and lift the urethra, which helps prevent leaks.
This type of surgery can also be used to treat urinary incontinence in women. The surgeons make two cuts, one in the vagina and one in the belly. The sling will be stretched through the cut in the stomach, then stitched to the inside of the stomach wall. It will support the urethra behind the pubic bone.
These procedures are usually performed under anesthesia.
Your surgeon will take a strip of your body tissue, either from your stomach or your thigh to make the sling. Slings might also be made from donor tissue or plastic material that is compatible with body tissues. Then they make a small cut between the scrotum and anus and put the sling around part of the urethral bulb.
What Should Women Do If They Have Concerns
Drs. Harmanli and Rickey say they have received numerous phone calls from past and current patients anxious about the news they have been hearing about pelvic mesh. If a woman was treated transvaginally with mesh for pelvic organ prolapse and has no complaints, she shouldnt worry and does not need to take any action, Dr. Harmanli says.
The word mesh shouldnt scare women, Dr. Rickey adds. There are other options to treat these disorders, and mesh is but one tool in a tool box with many others. Any treatment is a shared decision between doctor and patient, and we discuss the benefits and risks very carefully.
Don’t Miss: Does Azo Help Bladder Spasms
Complications During Or Shortly After Surgery
Intraoperative or perioperative complications occur during surgery or shortly after. In general, these are rarer. Complication rates range from less than 1 percent to 14 percent, according to Costantini and colleagues. Major complications such as vascular and nerve injuries and gut lesions occurred in less than 1 percent of women. Minor bladder injuries had rates from 0.5 to 14 percent. Significant blood loss occurred in about 2.7 percent to 3.3 percent of women.
Do Bladder Slings Need To Be Replaced
If your bladder sling is placed improperly or shifts over time, it may need to be removed or replaced.As with any operation, its important to weigh the pros and cons, and consult your doctor for advice. For many women, bladder sling surgery provides powerful relief to chronic stress-induced incontinence, and can be a safe, minimally invasive procedure.
Don’t Miss: Do Bladder Infections Go Away On Their Own
Potential Risks And Complications
Although laparoscopic colposuspension has proven to be very safe, as in any surgical procedure there are risks and potential complications. Potential risks include:
-
Bleeding: Although blood loss during this procedure is relatively low compared to open surgery, a transfusion may still be required if deemed necessary either during the operation or afterwards during the postoperative period.
-
Infection: All patients are treated with intravenous antibiotics, prior to the start of surgery to decrease the chance of infection from occurring within the urinary tract or at the incision sites.
-
Adjacent Tissue / Organ Injury: Although uncommon, possible injury to surrounding tissue and organs including bowel, vascular structures, pelvic musculature, and nerves could require further procedures. Transient injury to nerves or muscles can also occur related to patient positioning during the operation.
-
Hernia: Hernias at the incision sites rarely occur since all keyhole incisions are closed under direct laparoscopic view.
-
Conversion to Open Surgery: The surgical procedure may require conversion to the standard open operation if extreme difficulty is encountered during the laparoscopic procedure . This could result in a standard open incision and possibly a longer recuperation period.
Top Things To Look For
Find a doctor who:
-
Is board certified and who specializes in pelvic prolapse surgery
-
Has experience treating patients with your specific condition
-
Practices at a hospital known to have high-quality outcomes in pelvic prolapse surgery or gynecologic surgery in general
-
Accepts your insurance
-
You are comfortable talking with and who fully answers your questions
Here are five steps to finding the best doctor to perform your pelvic prolapse surgery.
Don’t Miss: I Feel A Lot Of Pressure On My Bladder
What Are The Different Types Of Sling Surgery
The two most common types of bladder slings are midurethral and traditional.Midurethral: This sling is inserted during an outpatient procedure that only takes about 30 minutes. Typically, a strip of synthetic mesh is inserted through a single incision in your vagina, and cradles the urethra like a hammock. The procedure may also involve a retropubic method in which two additional incisions are made near the pubic bone to secure the mesh. The transobturator method is another midurethral option in which small incisions are made in the vagina and the labia to secure your sling.Traditional: A traditional, or conventional, bladder sling is inserted during an inpatient procedure, which means you will likely spend a night in the hospital afterward. Traditional bladder sling surgery may use synthetic mesh, or tissue from your own body . With this method, one incision is made in your vagina and one in your belly, in order to connect the sling using tension under the bladder neck. Conventional bladder sling recovery can take longer and may involve more complications.
What You Should Know:
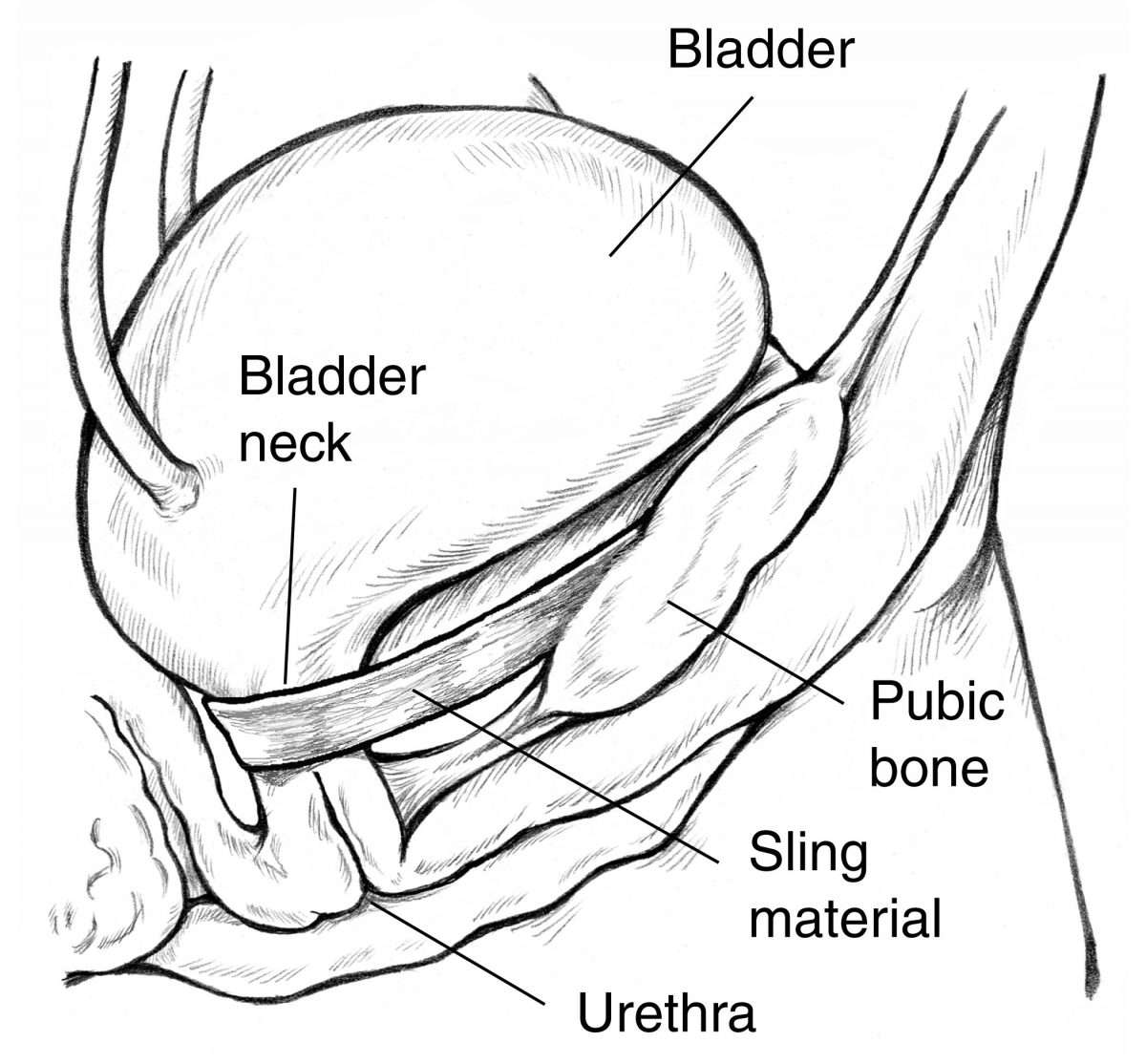
- A bladder sling procedure is done to treat women who have urinary incontinence. Urinary incontinence occurs when urine leaks out of your bladder. Your bladder is an organ at the bottom of your abdomen where urine is stored. Urine leaves your bladder through a tube called your urethra. Strong muscles around your urethra keep urine from leaking out. If these muscles weaken, you may have trouble controlling your urine flow. Urine leakage occurs most often when you cough, sneeze, laugh, or lift objects.
- A bladder sling procedure may be done through a cut in your vagina only. The procedure may also need to be done through a cut in your abdomen and vagina. A strip of body tissue is used as a sling to hold your urethra in place and make it stronger. Part of the thick covering of your abdominal muscles may be used for your sling. Your sling also may be made from a strip of your vaginal tissue, donor body tissue, or man-made. The sling helps keep your urethra closed even when your bladder is full. Having a bladder sling procedure may help you control your urination. The bladder sling procedure may decrease or resolve your urinary incontinence.
Read Also: What Is A Bladder Tuck
What Kind Of Doctor Is Best
Start with your primary care doctor. Your doctor may recommend a specialist with certification in Female Pelvic Medicine and Reproductive Surgery , such as a gynecologist, a urologist or a urogynecologist, also known as a urogyn. A urogynecologist is a medical doctor who has completed a residency in obstetrics and gynecology or urology. He or she has received additional training and experience in evaluating and treating conditions that affect the female pelvic organs, as well as the muscles and connective tissue that support them. Common problems treated by a urogynecologist include urinary incontinence or leakage, pelvic organ prolapse and overactive bladder.
How Is Incontinence Sling Surgery For Women Performed
Your incontinence sling surgery will be performed in a hospital or surgery clinic. The procedure varies depending on the type of incontinence sling. The sling can be made of tissue from your own body, someone elses body, or from a synthetic material. The surgery generally involves looping the sling under your urethra to provide support and compress it to control urination. Your surgeon then attaches the sling to strong tissues in your lower abdomen.
Recommended Reading: Can You Have A Bladder Infection Without Uti
How Does Sling Surgery Work
A woman who has pelvic organ prolapse may be a candidate for sling surgery.
During the procedure, the doctor makes an incision in the vagina to see where the problem areas are.
The doctor then pulls up the vaginal lining and supportive structures through this incision.
The doctor then places a piece of graft material over these structures to support them while they heal.
The doctor then makes another incision in the lower abdomen to access the inside of your pelvis and create a tunnel into your vagina where the graft material can be anchored.
The doctor then threads the graft material through this tunnel into the vaginal space, where it is then secured in place with stitches, clips, or both. After reinforcing the area with the graft material, the doctor closes up the incisions.
What Should I Expect After A Bladder Sling Procedure
- Medicines may be given to prevent or treat pain or a bacterial infection.
- You may have some pelvic discomfort after your surgery.
- You may find it hard to urinate, or it may feel different than it did before surgery. You may urinate more slowly than you did before surgery. You may need to use a catheter to empty your bladder a few times a day until your function returns. You may have a Foley catheter for a short period of time to drain your urine.
- You will need to avoid any activity that can strain your surgery area. This includes heavy lifting, strenuous exercise, or straining for a bowel movement.
Don’t Miss: Women’s Bladder Control Underwear
How Common Is The Use Of Surgical Mesh To Repair Pelvic Organ Prolapse And Stress Urinary Incontinence
About 300,000 women in the United States underwent surgery to repair POP in 2010. Surgical mesh was used in about one out of three procedures. About 250,000 women in the U.S. underwent surgery to repair SUI in 2010, with mesh placement being used in over 80% of the procedures. The mesh sling has been the most widely studied procedure for stress incontinence in the history of stress incontinence surgery. All of the major urologic and gynecologic societies in the U.S. have supported its continued use as of 2019.
Changes In Health Status And Symptoms
The changes from baseline in urinary symptoms as measured on the Pelvic Floor Distress Inventory, including the Urinary Distress Inventory stress subscale, and the Incontinence Severity Index at 3 months were greater in the sling group than in the sham group . At 12 months, only the changes from baseline for the stress urinary incontinence subscale and Incontinence Severity Index were greater in the sling group than in the sham group. There were no significant between-group differences at 3 and 12 months in changes in generic health , other pelvic-floor symptoms, effect on quality of life, sexual function, or pain .
Read Also: What Do They Give You For Bladder Infection
General Principles Of Management Of Mesh And Graft Complications
Approaches to management of mesh-related complications in pelvic floor surgery include observation, physical therapy, medications, and surgery. Table 1 presents an overview of specific mesh and graft complications and management options. There may be settings in which observation of exposed mesh is reasonable 4. Surgical intervention or referral is not always necessary for type 1 mesh exposures into the vagina. Asymptomatic exposures of monofilament macroporous meshes can be managed expectantly. For women with symptoms, a trial of vaginal estrogen can be attempted for small mesh exposures. Topical estrogen may improve or resolve the mesh exposure, though there is little prospective, comparative evidence supporting this approach. A period of 612 weeks is a reasonable period to try topical estrogen.
One multicenter study of mesh complications after reconstructive surgery found that 60% of women required two or more interventions and that the first intervention was surgical in approximately one half of cases 5. These procedures are complex and should be approached with caution. Surgeons who are unfamiliar with the original index procedure or the management issues that follow should refer the patient to a surgeon who is familiar with these types of repairs.
What Are The Advantages Of The Male Sling Procedure
The male sling procedure is not a major surgery. One of the advantages is that the male sling procedure only requires a small incision in the perineum . Because of this small incision, the recovery time is fairly short. Most patients have their catheters stay in for one to three days depending on surgeon preference.
Recommended Reading: T1 Bladder Cancer Life Expectancy
Where Can Someone Get More Information On Prolapsed Bladders
- Urologic conditions that can occur around the time a woman goes through menopause include
- bladder control problems,
- bladder prolapse , and
- urinary tract infections.