Frequency Dependence Of Tns Effects
When CMGs were stable, 30 min of stimulation at 10 Hz on the tibial nerve significantly inhibited bladder activity in the unanesthetized rats. As shown in Fig. , stimulation at 10 Hz frequency resulted in a significant increase in BC and VV to 144.1±5.07% and 147.5±4.24% of pre-stimulation respectively, as well as a significantly longer duration of effects on ICI to 135.3±4.60% of pre-stimulation. However, no significant difference in VP before and after stimulation was found. By contrast, TNS at 50 Hz resulted in a significant excitation in bladder activity after 30 min of stimulation. Though BC and VP at 50 Hz showed no change compared to the pre-stimulation results, significant decreases in both ICI and VV were observed as shown in Fig. .
Figure 1
The pre- and post-stimulation effects of the 30 min 10 Hz TNS. Representative CMG traces of pre- and post-stimulation of 30 min at 10 Hz. bladder capacity, voiding pressure, inter-contraction interval, voiding volume. The normalized data are presented as a mean with the standard error. The significance of the differences between the pre- and post-stimulation results were determined by the Students t-test .
How Frequent Are Ptns Sessions
Peripheral Tibial Nerve Stimulation therapy is usually divided into two phases: induction and maintenance. Patients begin with induction treatment consisting of 12 weekly sessions. Most people begin to see improvement by session 6 but the full 12 sessions may be necessary for many patients to see satisfactory improvement. If the twelve induction treatments have been successful in controlling OAB symptoms, treatment then moves to a maintenance phase, which is less frequent. Treatments are typically every 3-4 weeks, though some patients are able to space these out even more. The maintenance treatments have to be maintained to continue to see the positive effects on bladder symptoms.
What Is Malaria And How To Prevent It
Malaria is a very common infection and can be life-threatening but it is preventable. Here are a few tips on prevention of malaria. Malaria is caused by the bite of the female Anopheles mosquito. In Pregnancy, Malaria infection carries significant risks to mother and baby. Miscarriage, stillbirth and premature labour are the main complications of malaria. What are the measures to prevent malaria? The ABCD of malaria prevention is as follows: Awareness of risk Bite prevention Chemoprophylaxis Diagnosis and treatment must be prompt Education about the cause and symptoms of malaria is useful. How can I prevent mosquito bite that causes malaria? Use skin repellentsKnock-down mosquito sprayInsecticide-treated bed netsClothing and room protection The anopheline mosquito has different preferred biting times in different parts of the world. But the maximum risk period is from dawn to dusk. Therefore the mosquito bite prevention measures need to be applied 24 hours a day. Skin repellents containing 20% DEET Have been used and there are no apparent adverse effects Knock-down mosquito sprays Permethrin and Pyrethroids sprays kill resting and flying mosquitoes. A can of insect spray active against mosquitoes is useful to help clear the room of mosquitoes.
Don’t Miss: What Can You Do For An Overactive Bladder
Ptns For Overactive Bladder
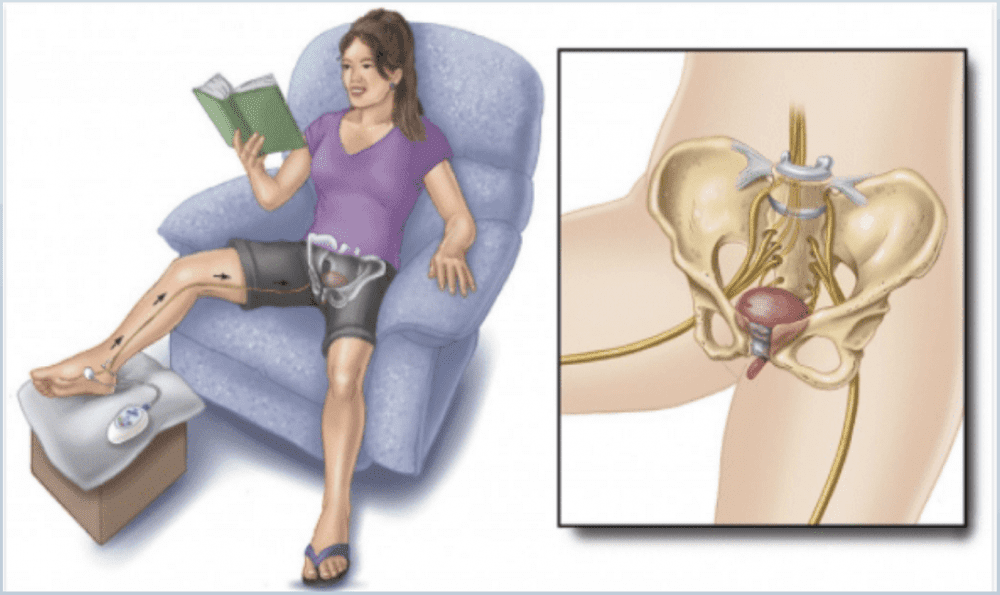
What is PTNS for OAB? Percutaneous Tibial Nerve Stimulation, or PTNS, is a non-surgical treatment for OAB. Medication isnt always effective against the symptoms of Overactive Bladder, and sometimes the side effects interfere with quality of life. PTNS can help reduce OAB symptoms by relaxing the bladder muscles.
How does PTNS for OAB work?PTNS therapy works by stimulating nerves through gentle electrical impulses, called neuromodulation. During the PTNS procedure, your foot is elevated and a slim needle electrode is placed by the tibial nerve in the ankle. Mild electrical impulses are sent to the sacral nerve via the tibial nerve. The sacral nerve plexus is responsible for bladder function.
PTNS can change bladder activity. You will receive a series of 12 weekly treatments that usually last 30 minutes each. After the 12 treatments, your response to PTNS will be assessed. Additional treatments may be needed to continue OAB symptom improvement.
How effective is PTNS for OAB?Studies report that between 60 and 80 percent of patients see OAB symptom improvement with PTNS. This includes reduction in the number of leakages and urgency episodes per day. Many also reported quality of life improvements.
Symptoms like these can mean youre planning your life around having access to a bathroom and no longer participating in the activities you love. You may find yourself worrying about OAB every day.
- Bruising or bleeding where the needle is inserted
- Tingling
What Works Best To Help Men With Overactive Bladder
HealthDay Reporter
TUESDAY, Jan. 14, 2020 Learning how to control the urge to urinate may be all the therapy men need to treat an overactive bladder, a new study suggests.
A combination of drugs and behavioral therapy seems to work better than drugs alone, but behavioral therapy alone also worked better than drugs, the researchers found.
The trial of 204 men with overactive bladder suggests behavioral therapy may be a good way to start treatment, the study authors said.
The study provides good evidence that for the group of men with overactive bladder, symptoms without obstruction from an enlarged prostate can be successfully managed with behavioral therapy alone, said Dr. Manish Vira, who was not involved with the study, but reviewed the findings. Hes vice chairman of urologic research at Northwell Healths Arthur Smith Institute for Urology in Lake Success, N.Y.
Many medications typically prescribed for overactive bladder have significant side effects, especially in older men using multiple medications, Vira added.
For the trial, Kathryn Burgio, associate director of research at the Birmingham VA Medical Center in Alabama, and colleagues randomly assigned men to six weeks of behavioral therapy alone, drug therapy alone, or combined drug and behavioral therapy. After the initial six weeks, all of the men received combination therapy for another six weeks.
Show Sources
Don’t Miss: Over The Counter Bladder Control Meds
Pelvic Floor Exercises Can Help Immensely
You cant see your pelvic floor muscles however, just like other muscles in your body they lose their strength if they are not put to use.
Pelvic floor exercises help strengthen the pelvic floor when done consistently at least twice a day. How are they done?
- Imagine you are holding back gas or urine.
- Squeeze and lift the rectal area without tightening your buttocks or belly. Try and hold it for a count of three before relaxing. Repeat this cycle 10 times. Do 10 sets of Kegel exercises, at least 3 times a day.
- Increase your contractions as your doctor recommends.
- Do not hold your breath when you do Kegel exercises. Keep your stomach, back, and leg muscles relaxed.
- Dont use Kegel exercises to start and stop your urine stream which can lead to incomplete emptying of the bladder and an increased risk of a urinary tract infection.
Review our information about Kegel exercises for both women and men to learn more about the techniques.
Ptns Compared With Transvaginal Stimulations And Pelvic Floor Muscle Training
It is thought that pelvic floor muscle stimulation leads to reflex contraction of the striated paraurethral and periurethral muscles with simultaneous reflex inhibition of the detrusor muscle. Ugurlucan et al. compared the effects of transvaginal electrical stimulation and PTNS in a randomized controlled trial. The study demonstrated that there was no statistically significant difference between the two groups in objective measurements. Quality of life assessments showed improvements in both groups but only a significant difference in the social limitations domain between ES and PTNS .
Another randomized controlled trial compared PTNS and ES with pelvic floor muscle training in 60 women with OAB with 30 participants allocated to each arm . The PTNS group demonstrated a significant reduction in frequency, nocturia and urge incontinence. When the two groups were compared after treatment, women treated with PTNS showed statistically significant improvement compared with those treated with ES and PFMT. Quality of life assessment comparing post-treatment data also showed patients treated with PTNS had better results than those treated with ES and PFMT.
You May Like: How To Control Bladder Leakage
The Science Behind Sacral Neuromodulation
One way the brain controls our bodys muscles and movements is through electrical messages, which are carried by nerves. These nerves have major routes with smaller pathways running off them.
One major route runs from the brain, along the spinal cord and through the lower back called the sacral area. Here, nerve paths split off and go in different directions, some to the pelvic area. The muscles in the pelvic area, such as the pelvic floor, urethral sphincters, bladder and anal sphincter muscles are controlled by the brain through nerves that run from the sacral area. Our sensations, such as fullness in the bladder or rectum, are also relayed to the brain via these nerve routes.
Sacral Neuromodulation helps to correct inappropriate, unwanted or even erroneous messages sent along these nerve pathways.
Benefits Of Sacral Nerve Stimulation
SNS has a myriad of benefits!
1. Minimal Side Effects
Though SNS requires a surgical implant placed through an invasive procedure, the side effects are considered minimal. In fact, most people do not have any side effects.
The most common side effect is infection at the device implantation site this occurs in approximately 3% to 4% of cases. It is important to note that any surgical procedure carries a risk of infection.
Occasionally, mechanical failure can occur. If this occurs, the device can typically be reprogrammed.
Technical problems, lead movement and adverse stimulations can occur. However, these side effects are considered rare and can easily be resolved.
Pain at the insertion site is not expected, though slight soreness may occur for several weeks postoperatively.
2. Reversible Treatment
Though most people find that any benefits outweigh the possible side effects, the system is reversible. This means that the system can be removed through a minor surgical procedure. SNS can be discontinued without any permanent damage to the nerves.
3. Safe for MRIs
Magnetic resonance imaging has been contraindicated with SNS implants in the past. This was because older models of SNS used lead. New models are considered MRI-safe. However, there are other treatments that are still considered incompatible with SNS, such as diathermy.
4. Lengthy Battery Life
5. Reduction in Symptoms
You May Like: High Grade Non Invasive Bladder Cancer
Percutaneous Tibial Nerve Stimulation
PTNS is a nonsurgical option that uses electrical stimulation to control an OAB.
With PTNS, a small-sized electrode is fixated on the lower part of your leg, close to your ankle. This electrode sends signals to your tibial nerve, which runs all the way to your lower back. Often, PTNS requires an average of 12 treatments to work properly.
One of the latest models of these stimulators is no larger than a nickel and can be implanted under the skin of your lower leg. This implant is a simple procedure that can be done under local anesthetic in a urologists office.
Transcutaneous Tibial Nerve Stimulation
Posterior tibial nerve stimulation is given via two 50 mm×50 mm electrode pads. The live pad is placed posterior and superior to the medial malleolus and the ground pad is placed approximately 10 cm cephalad to this. Continuous stimulation at a pulse width of 200 ls and a frequency of 10 Hz is used. The amplitude was set to produce a sensory stimulus in the ipsilateral foot, at an intensity tolerable to the patient. Stimulation is given for 30 min.
Read Also: Stage 3 Bladder Cancer Symptoms
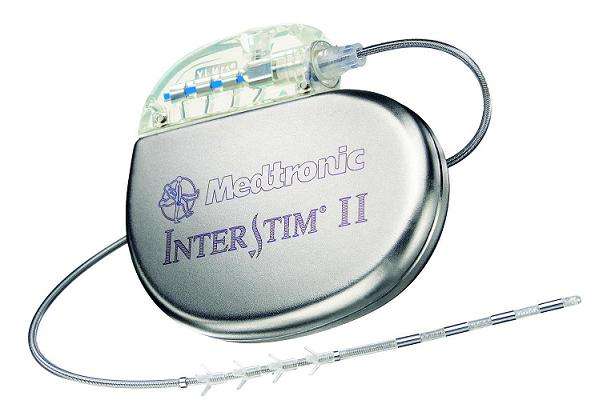
How Does Sacral Nerve Stimulation Actually Work
Sacral nerve stimulation therapy uses a small device that is implanted under the skin in the upper buttock area. The device sends mild electrical impulses through a lead that is positioned close to a nervelocated in the lower back , which influences the bladder,the sphincter and the pelvic floor muscles.
A neurotransmitter device, implanted under the skin in the upper buttock area, transmits mild electrical impulses through a lead wire close to the sacral nerve. The impulses, in turn, influence the bladder sphincter and pelvic floor muscles providing bladder control.
How Big Is The Device
Medical technology has made significant advances in recent years, and implantable medical devices have gotten smaller. The current device, which is about the size of a thumbnail drive, is smaller than most pacemakers. A new version is available that has a rechargeable battery that lasts about 15 years. These devices also are MRI-safe so you can have scans of your hips, back or legs in the future, if needed.
Also Check: Apple Cider Vinegar And Bladder Infection
Testing For Overactive Bladder
A number of tests may be performed during or after your visit, depending on the patients history and evaluation. These can be done right in the same office, most often at the same time as your appointment. All of the information from your history is important and will also be used to make an accurate diagnosis.
Recommended Reading: Best Foods To Eat For Bladder Infection
What Are The Various Pregnancy Myths All Over The World
Most of us have certain notions and beliefs that may or may not be right. Pregnancy is one such issue where myths are common, and vary from region to region and culture to culture. These are the common old wives tales that are the subject of discussions in kitty parties. Let me discuss some of them here. Myth: One should not eat papaya in pregnancy. You can consume papaya. Hundreds of years ago papaya seeds were consumed to bring about termination. Ripe papaya is good for you and the baby. Myth: When you are pregnant you need to eat for two. Please dont. Remember you will have to work double to lose that weight. It is important to just eat well balanced, healthy small frequent meals. Myth: If you crave for salty foods, then you have a baby boy. Cravings in pregnancy have nothing to do with the sex of the child. There is no scientific explanation for the cravings and they probably are just secondary to the hormonal changes in the body. Myth: It is best to avoid sex during pregnancy. It is alright to have sex during pregnancy. You should avoid it only in case the doctor specifically
Also Check: What Can Be Done For Bladder Leakage
Recommended Reading: Best Vitamins For Overactive Bladder
Top 6 Pregnancy Myths
Most of us have certain notions and beliefs that may or may not be right. Pregnancy is one such issue where myths are common, and vary from region to region and culture to culture. Here are half a dozen pregnancy myths around the world. These are the common old wives tales that are the subject of discussions in kitty parties. Let me discuss some of them here. Myth: One should not eat papaya in pregnancy. Fact: You can consume papaya. Hundreds of years ago papaya seeds were consumed to bring about termination. Ripe papaya is good for you and the baby. Myth: When you are pregnant you need to eat for two. Fact: Please dont. Remember you will have to work double to lose that weight. It is important to just eat well balanced, healthy small frequent meals. Myth: If you crave salty foods, then you have a baby boy. Fact: Cravings in pregnancy have nothing to do with the sex of the child. There is no scientific explanation for the cravings and they probably are just secondary to the hormonal changes in the body. Myth: It is best to avoid sex during pregnancy. Fact: It is alright to have
Also Check: Superficial Bladder Cancer Survival Rates
What Are The Risks Of Peripheral Tibial Nerve Stimulation
An important advantage of PTNS is that the risks and side effects are minimal. Some patients experience discomfort from the stimulation but this can usually be fixed by turning down the stimulation setting or moving the needle. Discomfort very rarely prevents treatment from being completed. There can be some slight bleeding at the insertion site but the needle used is so fine that any bleeding quickly stops without intervention. One important note, PTNS is not intended for patients with a pacemaker or defibrillator as there is concern that this type of stimulation may interfere or trigger the cardiac device.
An unfortunate obstacle to PTNS therapy is the need for an office visit to receive the therapy. After completion of the 12-week induction phase the average patient will need to repeat therapy every 4 weeks. For people who do not live near a provider who is experienced with PTNS, this may limit their access to the treatment. There are several solutions to this dilemma under investigation that will hopefully expand access to this therapy in the future.
You May Like: How To Strengthen Your Bladder
Posterior Tibial Nerve And Oab
- Percutaneous tibial nerve stimulation, requiring needle-tip electrodes which are invasive and expensive.
- Transcutaneous tibial nerve stimulation , which requires just a basic TENS machine and standard electrodes. TTNS is much more cost effective than percutaneous tibial nerve stimulation, and much simpler to administer.
You May Like: How To Empty Your Bladder With A Uti
Weight Loss May Reduce Incontinence
Study Shows Losing Weight Can Help Women Who Have Urinary Incontinence
Jan, 27, 2009 For obese and overweight women, losing weight can dramatically reduce episodes of incontinence, according to a study published in the New England Journal of Medicine.
Study participants included 338 women, all overweight or obese, who leaked urine at least 10 times in a week. The women were recruited from Birmingham, Ala., and Providence, R.I.
Participants were randomly divided into two groups. One group was put on an intensive weight loss program that included diet, exercise, and behavior modification. The other group was given educational information about weight loss, healthy eating, and physical activity, but no hands-on support.
All participants received an educational booklet about urinary incontinence, behavioral techniques, and pelvic floor muscle exercises.
At six months, the women in the intensive weight loss program lost an average 8% of their body weight and reduced weekly urinary incontinence episodes by 47%. Women in the information-only group lost an average 1.6% of body weight and had 28% fewer episodes.
Women in the weight loss program reported feeling that incontinence was less of a problem compared to the other group. More were moderately to very satisfied with the change in their incontinence.
Show Sources
Dont Miss: Malignant Neoplasm Of Bladder Unspecified Icd 10
Recommended Reading: Antimuscarinic Medications For Overactive Bladder