Remission And The Chance Of Recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having no evidence of disease or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
If the cancer returns after the original treatment, it is called recurrent cancer. It may come back in the same place , nearby , or in another place .
If a recurrence happens, a new cycle of testing will begin again to learn as much as possible about it. After this testing is done, you and your doctor will talk about the treatment options.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence.
How Is Systemic Chemo Different From Intravesical Chemo
Although systemic chemotherapy drugs target cancer cells, all of the cells in a patients body are exposed to the medicine. In this way, systemic chemotherapy is different than another way that chemotherapy medicine can be delivered, called intravesical chemotherapy. In intravesical chemotherapy for treating early stage or non-muscle-invasive bladder cancer, the medicine is delivered directly into the bladder where it only has an effect on the cancer cells located in the lining of the bladder.
What Type Of Chemotherapy Is Used For Bladder Cancer
Cisplatin-based chemotherapy has been the best standard treatment for bladder cancer since the 1970s. Based on the results of clinical trials from the 1990s, the two regimens most commonly used are dose-dense MVAC and GC. Chemotherapy goes into the body through a vein. It may be infused with a catheter into a vein or through a port that is placed under the skin, usually in the right side of the chest.
MVAC uses four drugs: methotrexate , vinblastine , doxorubicin , and cisplatin . We no have effective anti-nausea medication and injections that can keep immune systems from being depleted by chemotherapy. This has have improved our ability to give MVAC safely on an accelerated dose-dense schedule. The National Comprehensive Cancer Network now recommends MVAC be given according to the dose-dense or DD schedule due to improved toxicity and suggested improvement in efficacy compared with the standard schedule. Click here to view the NCCN Guidelines.
A clinical trial conducted in the late 1990s showed that the combination of gemcitabine , plus cisplatin , gives similar anticancer effects to standard MVAC combination. Both GC and DD MVAC have been useful in bladder cancer in delaying recurrence, extending life and sometimes achieving a cure, and both regimens are routinely used in the neoadjuvant and metastatic settings. Clinical trials are underway to assess whether the addition of another agent to these regimens improves outcomes.
Don’t Miss: What Does Bladder Pain Feel Like
Chemotherapy In Bladder Preservation Protocols For Muscle
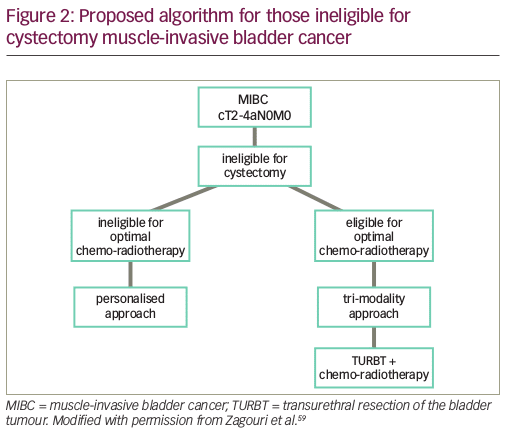
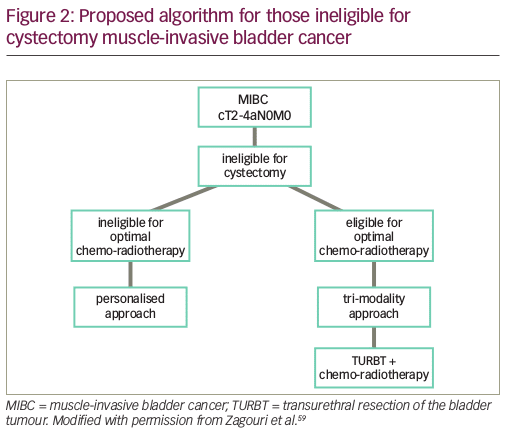
In appropriately selected patients, bladder preservation with trimodal therapy is a potential alternative to cystectomy for the treatment of MIBC. This approach combines radiotherapy, chemotherapy, and a complete transurethral resection of the bladder tumor. Earlier studies using cisplatin alone or in combination with fluorouracil and radiation have an average response rate around 75% with 5-year survival of 50%60%, similar to cystectomy. Cisplatin and paclitaxel have also been given with radiation, however, with additional adjuvant cisplatin and gemcitabine with 5-year OS of 50%. Twice weekly gemcitabine in combination with radiotherapy has been used in a Phase 1 study with a reported 5-year bladder-intact survival of 62%, OS 76%. A Phase 2 study }NCT01495676 is recruiting for concurrent GC with radiation. The BC2001 is a Phase 3 RCT that compared radiotherapy alone to concurrent chemoradiotherapy with 5-FU and mitomycin C. Around 30% of patients underwent NACT before enrollment. The chemotherapy group had a statistically significant improvement in 2-year locoregional DFS 67% versus 54% , with a trend toward improvement in OS at 5 years were 48% versus 35% . Results are awaited from the closed Radiation Therapy Oncology Group trial }NCT00777491 comparing cisplatin and 5-FU to gemcitabine in combination with radiation. Other alternatives to cisplatin that have been reported on include capecitabine, paclitaxel, and docetaxel .
How Many Rounds Of Chemo Do You Need For Bladder Cancer
Sometimes, intravesical chemotherapy is used to treat high risk noninvasive bladder cancers. The more aggressive the cancer, the more aggressive the treatment.
A person with a fast-growing cancer may be advised to go through several intravesical chemotherapy treatments for 1 to 3 years, depending on how their bladder cancer responds to treatment.
Also Check: Bladder Control Products By Mail
Side Effects Of Chemotherapy
Chemo drugs attack cells that are dividing quickly, which is why they work against cancer cells. But other cells in the body, such as those in the bone marrow , the lining of the mouth and intestines, and the hair follicles, also divide quickly. These cells are also likely to be affected by chemo, which can lead to side effects.
The side effects of chemo depend on the type and dose of drugs given and how long they are taken. When chemo and radiation are given at the same time, side effects tend to be worse. Common side effects of chemo include:
- Nausea and vomiting
- Increased risk of infections
- Easy bleeding or bruising, even after minor cuts or injuries
These side effects usually go away over time after treatment ends. There are often ways to lessen these side effects, some can even be prevented. For instance, drugs can be used to help prevent or reduce nausea and vomiting. Ask your health care team about the side effects your chemo drugs may cause and what can be done to prevent and/or treat them.
Some chemo drugs can cause other, less common side effects. For example, drugs like cisplatin, docetaxel, and paclitaxel can damage nerves. This can sometimes lead to symptoms such as pain, burning or tingling, sensitivity to cold or heat, or weakness. This is called peripheral neuropathy.
What Are The Possible Side Effects Of Chemotherapy
Systemic chemotherapy drugs are very powerful and they can affect cells in the entire body.1 Chemotherapy drugs can have a negative effect on cells that are healthy but multiply quickly, like the cancer cells that chemotherapy drugs target. This can cause side effects related to bone marrow, hair follicles, the inside of the mouth, and the intestinal lining.
People treated with systemic chemotherapy experience different side effects depending upon their overall health, the type of chemotherapy drug, and how long the treatment lasts. Side effects that are common include:
- Nausea and vomiting
While side effects from systemic chemotherapy can be difficult, they tend to go away after the treatment is over. Your healthcare providers will talk with you about what types of side effects that you might experience from chemotherapy and about ways to potentially reduce those effects. This is not an exhaustive list of all potential side effects of systemic chemotherapy. Talk to your doctor for further information about your specific treatment.
Patients receiving systemic chemotherapy should talk to their doctor about any other medications , herbal remedies, and any supplements they are taking, as well as any other health conditions.
Read Also: Does Roundup Cause Bladder Cancer
When Is Systemic Chemotherapy Used
Systemic chemotherapy for non-muscle-invasive bladder cancer is used:
- before surgery to shrink the cancer and make it easier to remove it can also reduce the risk of the cancer coming back
- after surgery if there is a high risk of the cancer coming back.
Systemic chemotherapy can sometimes be combined with radiation therapy as part of trimodal therapy. Systemic chemotherapy may also be used for bladder cancer that has spread to other parts of the body.
Systemic Treatment Of Stage Iv Bladder Cancer
Before the development of effective chemotherapy, the average survival of patients with stage IV bladder cancer was only 3-6 months from diagnosis. Bladder cancer, however, is sensitive to chemotherapy and may respond to treatment frequently and rapidly. Although long-term survival has been reported in some patients, chemotherapy is administered primarily to improve the symptoms of bladder cancer. Patients in good clinical condition should enter treatment with curative intent because some patients have prolonged remissions without cancer recurrences.
Combinations of chemotherapy agents are usually used for treatment of bladder cancer, as no single chemotherapy agent will produce a complete response in more than an occasional patient. Two commonly used chemotherapy regimens are GC and MVAC. GC is the combination of Gemzar® and cisplatin. MVAC is the combination of methotrexate, vinblastine, doxorubicin, and cisplatin. A phase III trial that compared these two regimens suggested that they were similarly effective, but that GC produced fewer side effects.1,2
Also Check: Papillary Bladder Cancer Survival Rates
What Is Intravesical Chemotherapy
When it comes to treating cancers, chemotherapies remain a popular option.
Chemotherapies involve putting strong drugs that stop cancer cells from reproducing, growing, and spreading into your body for a period of time.
Most chemotherapies are administered intravenously or orally with tablets. The type of chemotherapy someone might receive differs depending on the type of cancer, its severity, and a persons overall health.
Intravesical chemotherapy is one such treatment, which involves putting chemotherapy drugs directly into the bladder using a catheter through the urethra, which transports urine out of the body.
Rule : Randomized Trials Prove More Than Historical Comparisons Development Of Neoadjuvant Chemotherapy
More than 30 years ago, we began to develop combined modality approaches, incorporating systemic chemotherapy with definitive local treatments, based on the following concepts :
-
systemic chemotherapy may reduce the extent of local tumor
-
it allows clinical assessment of chemo-responsiveness of the tumor, thus allowing more rational decisions to be made regarding continuation of chemotherapy
-
it may control occult micro-metastases
-
if radiotherapy is planned, it may cause enhanced radiation responsiveness via synergistic effects between some cytotoxics and the biological impact of radiation.
In the mid-1980s, the MVAC and CMV regimens were shown to be highly active against metastatic bladder cancer with apparently superior results to single agent therapy , an improvement confirmed in an international randomized trial . With emerging understanding of the molecular complexity of bladder cancer, it was logical to test these complex regimens in the neoadjuvant setting and initial results were again very encouraging .
Although the North American Intergroup trial of neo-adjuvant MVAC revealed a very dramatic difference in median survival , the absolute improvement in long-term survival and potential increment of cure rate was also of the order of 7 percent . This improvement is consistent with the Nordic cooperative group trial 1 and most cisplatin-based combination regimens, as summarized in our meta-analysis .
Read Also: Bladder Frequent Urination At Night
Chemotherapy For Invasive Bladder Cancer: Five Simple Rules Learned Over 30 Years
Article type: Review Article
Authors: Raghavan, Derek*
Affiliations: President, Levine Cancer Institute, Carolinas HealthCare System, Charlotte, NC, USA
Correspondence: Correspondence to: D. Raghavan, Levine Cancer Institute, Carolinas HealthCare System, PO Box 32861, Charlotte, NC, 28232-2861, USA. Tel.: +1 980 442 3115 Fax: +1 980 442 3101
Keywords: Invasive, bladder cancer, chemotherapy, neo-adjuvant, adjuvant, chemo-radiation, bladder preservation, geneexpression, P53, gemcitabine, paclitaxel, MVAC, CMV, PD-L1, c-MET gene
DOI: 10.3233/BLC-150010
Journal: Bladder Cancer, vol. 1, no. 1, pp. 3-13, 2015
Abstract
Invasive bladder cancer represents a useful metaphor for the treatment strategies for all solid tumors. The past thirty years has seen the evolution of increased understanding of the molecular biology of this disease, and the application of this knowledge to the design of clinical trials. In parallel, different modalities of treatment have been added to the therapeutic armamentarium, reflecting the natural history of the disease, and the limitations of each treatment. Randomized trials have identified clear progress in improving median survival and cure rates, but the clinical application of these advances has been marred by some missteps. This review considers approaches for the future, integrating knowledge gained from the past three decades, and proposes rules for the rational development of future treatment strategies.
Rule : Understand The Complex Biology Of Invasive Bladder Cancer When Designing Trials
Invasive, clinically non-metastatic bladder cancer, representing about 20% of new cases, includes tumors that penetrate through lamina propria into muscle and beyond. Thus more than 17,000 new cases occur each year in the USA, and also some cases of non-invasive bladder cancer eventually become invasive, but are not reflected in national incidence figures for invasive disease. In the USA, a reasonable estimate is that more than 20,000 patients require treatment for invasive bladder cancer per year . Most bladder cancers are urothelial carcinomas , formerly termed transitional cell carcinomas , which is the focus of this review. Other cell types include squamous cell carcinoma, adenocarcinoma, small cell carcinoma and very rarely sarcoma, lymphoma, or melanoma . Invasive bladder tumors are usually moderately to poorly differentiated . Our xenograft studies suggested the existence of a stem cell tumor of origin in bladder cancer, explaining why urothelial carcinoma may coexist with (and perhaps give rise to squamous and glandular patterns ofcancer . We have also demonstrated in these models clonal heterogeneity, reflected in histology and ultrastructure, tumor growth kinetics, expression of growth factors and their receptors, and response to treatment .
Don’t Miss: Catheterizing The Female Urinary Bladder
Which Chemo Drugs Are Used To Treat Bladder Cancer
Chemo drugs may be used alone or in combination, depending on what theyre being used for, a persons overall health, and other factors.
When chemo is given with radiation, the most common drugs used include:
When chemo is used without radiation, the most common combinations include:
- Gemcitabine and cisplatin
- Dose-dense methotrexate, vinblastine, doxorubicin , and cisplatin
- Cisplatin, methotrexate, and vinblastine
- Gemcitabine and paclitaxel
For some people, the side effects of getting more than one chemo drug might be too much to handle. For those people, treatment with a single drug, such as gemcitabine or cisplatin, may be an option. Other drugs sometimes used alone for bladder cancer include, docetaxel, paclitaxel, doxorubicin, methotrexate, ifosfamide, and pemetrexed.
Doctors give chemo in cycles, with each period of treatment followed by a rest period to allow the body time to recover. Each cycle typically lasts for a few weeks.
Most bladder cancers are transitional cell cancers, but there are other types as well, including squamous cell carcinoma, adenocarcinoma, and small cell carcinoma. These rare types of bladder cancer may be treated with drugs different from those listed above.
Surgery And Radiation Therapy
Endoscopic TURBT is the first-line treatment to diagnose, stage, and treat visible tumors. TURBT is not effective for CIS, because the disease is often so diffuse and difficult to visualize that complete surgical removal may not be feasible. It is critically important to surgically remove all nonmuscle-invasive disease prior to beginning intravesical therapy. When a combination of papillary tumor and CIS is present, the papillary tumor is removed before treatment of the CIS is initiated.
The EAU guidelines recommend the use of fluorescence-guided resection, as it is more sensitive than conventional white-light cystoscopy for detection of tumors. The added detection rate with fluorescence-guided cystoscopy is 20% for all tumors and 23% for CIS. The FDA has approved the use of blue-light cystoscopy with 5-aminolevulinic acid in patients suspected or known to have nonmuscle-invasive bladder cancer on the basis of prior cystoscopy.
As many as 20% of patients initially diagnosed with CIS may have unrecognized invasion beyond the lamina propria. Thus, they may not respond to intravesical therapy. These patients are candidates for radical cystectomy or radiation therapy and/or chemotherapy. Radiation therapy with or without chemotherapy is of limited benefit in patients with pure CIS but can be useful in some patients with muscle-invasive transitional cell carcinoma .
Lymph node dissection
Small cell carcinoma
Adenocarcinoma and lymphoma
Squamous cell carcinoma
Recommended Reading: What Helps A Bladder Infection
How Can Chemotherapy Be Used To Treat Bladder Cancer
Systemic chemotherapy affects cancer cells located in the bladder as well as in different parts of the body, so it is most often used to treat patients with advanced bladder cancer.1,2 Bladder cancer typically starts growing in the thin layer of cells that line the bladder, but it can continue to grow into the muscle of the bladder wall and spread beyond the bladder to other parts of the body.
How Is Chemotherapy Given
Most chemotherapy is given as an out-patient in an oncology unit. Thenurses are specially trained in talking to you about chemotherapy and in givingthe treatment.
Before you start your treatment you will need to have a blood test andbe seen by a doctor or nurse. Sometimesthis will be on the same day as your treatment, or some centres have a twoappointment system – a pre-chemotherapy assessment on one day and chemotherapydelivery on a different day.
The nurse will then insert a fine plastic tube into a vein in your arm. It may feel a little uncomfortable whilst it is beinginserted. Sometimes, chemotherapy is given through a vein in the crook of thearm or through a fine plastic tube inserted under theskin into a long vein near the collar bone. This is called a central line.
Before the chemotherapy is given, you will be given an anti-sicknessdrug which may be given though the cannula or as a tablet. If you are havingoutpatient treatment, you can go home after the chemotherapy. The cannula isremoved before you go home, unless you have a PICC or central line. If you haveeither a PICC or central line, you will be taught how to look after it whilstat home and how to shower etc with it in place.
Read Also: Robotic Surgery For Prolapsed Bladder