What Causes Bladder Pressure
Doctors arent sure what exactly causes IC. What they do know is that the bladder normally fills and then tells your brain to use the bathroom. It communicates this through the nerves in your body.
With IC, these signals get mixed up. You may feel like you need to urinate more frequently but without a lot of urine at each bathroom trip.
Bladder pressure may also be caused by:
- a defect in the lining of the bladder
- an autoimmune reaction
IC is more common in women than in men. Some people who have IC, also have other health issues such as irritable bowel syndrome and fibromyalgia. Other pain syndromes are also possible.
People who have both fair skin and red hair also have a greater risk of IC.
IC is primarily diagnosed in people in their 30s or older.
Botox For An Overactive Bladder
Although not commonly used, Botox is a handy muscle relaxer for a variety of conditions, including an overactive bladder. The compound is injected right into the bladder, and patients can experience fewer uncomfortable contractions and increased bladder capacity for up to a year after the injection has taken place.
However, Botox isnt without its dangers. Some patients find that after the procedure they retain urine too much, and experience pain and complications . For these reasons, Botox for overactive bladder treatment is only considered for certain people.
What Do Bladder Spasms Feel Like
Normally, the bladder gently fills with urine and you slowly become aware of the need to urinate. This feeling is your cue to start looking for a bathroom.
But in people who have bladder spasms, the sensation occurs suddenly and often severely. A spasm itself is the sudden, involuntary squeezing of a muscle. A bladder spasm, or “detrusor contraction,” occurs when the bladder muscle squeezes suddenly without warning, causing an urgent need to release urine. The spasm can force urine from the bladder, causing leakage. When this happens, the condition is called urge incontinence or overactive bladder.
People who have had such spasms describe them as a cramping pain and sometimes as a burning sensation. Some women with severe bladder spasms compared the muscle contractions to severe menstrual cramps and even labor pains experienced during childbirth.
You May Like: Best Pills For Bladder Infection
What Is Overactive Bladder
Overactive bladder syndrome is characterized by the occurrence of urinary urgency which is a sudden compelling desire to urinate that is difficult to postpone. It is usually accompanied by frequent urination and nocturia . It is also commonly accompanied by urgency incontinence, where urine is accidently lost with urgency. This commonly manifests as the inability to get to the bathroom on time once urgency starts. OAB is quite common and affects about 11-16% of adults to varying degrees. Although it is common, that does not mean that a person who is affected by OAB should simply live with the condition, as many do. For some OAB can have a profound effect on quality of life causing disruptions at work, curtailing of social activities, reduction of sexual intimacy, and interfere with sleep. However, it is important to know that there are effective treatments for the symptoms of OAB.
There are other conditions such as urinary tract infections , polyps or tumors in the bladder, and excessive drinking of fluids that can cause similar symptoms and these conditions should be ruled out by your health care provider before embarking on OAB treatment.
Section : Patient Presentation
Symptoms. When symptoms of urinary frequency and urgency, with or without urgency incontinence, are self-reported as bothersome the patient may be diagnosed with overactive bladder .27 Additionally, a caregiver or partner may perceive these symptoms as bothersome and lead the patient to seek care. It is common for patients to have suffered with their symptoms for an extended time before seeking medical advice.
Differentiation. OAB symptoms may occur only at night, causing a single symptom of nocturia. The differential of nocturia includes nocturnal polyuria ,28 low nocturnal bladder capacity or both. In nocturnal polyuria, nocturnal voids are frequently normal or large volume as opposed to the small volume voids commonly observed in nocturia associated with OAB. Sleep disturbances, vascular and/or cardiac disease and other medical conditions are often associated with nocturnal polyuria. As such, it is often age-dependent, increasing in prevalence with aging and with poorer general health.
Don’t Miss: Where Do You Feel Bladder Pain
Etiology Of Refractory Overactive Bladder
Refractory OAB might have more severe symptoms or have underlying pathophysiology not resolved after initial medication. The possible pathophysiology of refractory OAB includes occult neurogenic bladder, such as minor stroke, early dementia, Parkinsonism, and brain lesion bladder outlet obstruction such as bladder neck dysfunction , small prostate, urethral stricture and urethral incompetence-related OAB aging process and urothelial dysfunction chronic bladder inflammation central sensitization and autonomic dysregulation.
Because OAB in women has similar symptomatology with other common urologic diseases such as recurrent UTI, the majority of women with OAB are often diagnosed as UTIs and empirically treated without performing a urine culture as a routine care. In fact, when urine cultures are obtained, less than half of the women have a positive urine culture, suggesting that empiric treatment of UTIs without cultures commonly lead to a misdiagnosis of UTI. However, more and more evidence showing chronic low-grade bacterial bladder colonization might exacerbate OAB symptoms and may explain why the current OAB treatment strategies are not always successful. For OAB refractory to conventional medication such as antimuscarinics and beta-3 adrenoceptor agonist, mirabegron, using newer technologies such as 16S RNA sequencing and extended culture techniques, might find organisms that might be responsible for persistent OAB symptoms.
Studies Correlate Overactive Bladder Onset After A Covid
BALTIMORE, Sept. 10, 2021 /PRNewswire/ — The burden of COVID-19 can affect not only a patient’s respiratory health, but their bladder health as well. Two new studies being presented this year at the American Urological Association’s 2021 Annual Meeting demonstrate the relationship between COVID-19 and the onset of or worsening of symptoms of Overactive Bladder . The following study was presented during a virtual press session, which was moderated by Dr. Suzette Sutherland. The recording of this session is now available for viewing.
Abstracts Include:
Publication # MP29-15COVID-19 Associated Cystitis : Increased Urinary symptoms and biomarkers of Inflammation in Urine in Patients with Acute COVID-19
Emerging evidence suggests the bladder is one of many organs targeted by Severe Acute Respiratory Syndrome Coronavirus 2 , which contributes significantly to COVID-19 morbidity and leads to organ-specific complications. Hear from the first U.S. group to identify severe and bothersome de novo genitourinary symptoms in patients with confirmed SARS-CoV-2 infection, termed COVID-19 Associate Cystitis . The study sought to determine if this was associated with pro-inflammatory cytokines in the urine of patients.
Key findings:
Publication # MP63-02New or Worsening Overactive Bladder Symptoms After Recovery from COVID-19
Key findings:
Full abstracts can be viewed online:
Publication Number: MP29-15
|
Contact: |
Recommended Reading: How Do You Treat A Bladder Infection
Complementary Alternative And Integrative Therapies And Practices
There may be steps you can take on your own to improve your bladder control, either with or without medical therapies.
Keeping a bladder diary tracking your urination as well as food and beverage intake, and other activities can help you figure out what foods or behaviors might contribute to OAB.
Changing your urination behaviors may help train your brain to send signals to urinate in a more regular way. Techniques that may be helpful include:
- Double voiding
- Delayed voiding
- Timed urination
Its a good idea to talk with your doctor about these techniques before trying any of them.
You may also benefit from exercises that use your pelvic floor muscles, including the following:
- Kegels This exercise involves squeezing your pelvic muscles tight for a few seconds, then relaxing and repeating this for a set number of repetitions.
- Quick Flicks When you have the urge to urinate, you may be able to help control it by quickly squeezing and relaxing your pelvic muscles over and over.
Analysis Of Prostaglandins Inflammatory Chemokines And Cytokines
An association between inflammatory biomarkers and OAB has previously been suggested. To explore this, we investigated whether levels of these markers were altered in MSU samples from OAB and control patients. No significant differences between the OAB and control samples were noted for any of the markers evaluated , the mean values of which were within the normal physiological range for a healthy person.
Table 5 Concentrations of inflammatory prostaglandins, chemokines, and cytokines in OAB patients and controls.
Recommended Reading: Where Do You Feel Bladder Spasms
Difference Between Overactive Bladder Urinary Incontinence And Urinary Tract Infection
Overactive bladder , also known as overactive bladder syndrome, is a condition where there is a frequent feeling of needing to urinate to a degree that it negatively affects a persons life. The frequent need to urinate may occur during the day, at night, or both. Risk factors include obesity, caffeine, and constipation. Poorly controlled diabetes, poor functional mobility, and chronic pelvic pain may worsen the symptoms. People often have the symptoms for a long time before seeking treatment and the condition is sometimes identified by caregivers. Diagnosis is based on a persons signs and symptoms and requires other problems such as urinary tract infections or neurological conditions to be excluded. The amount of urine passed during each urination is relatively small. Pain while urinating suggests that there is a problem other than overactive bladder. Specific treatment is not always required. If treatment is desired pelvic floor exercises, bladder training, and other behavioral methods are initially recommended. Weight loss in those who are overweight, decreasing caffeine consumption, and drinking moderate fluids, can also have benefits. Medications, typically of the anti-muscarinic type, are only recommended if other measures are not effective. They are no more effective than behavioral methods however, they are associated with side effects, particularly in older people.
There are four main types of incontinence:
Lifestyle Steps That Can Help
There are several general self-care measures for urinary incontinence you can try. And with OAB, it may also be especially important to focus on your fluid intake, so try these tips too:
- drink enough fluid it can be tempting to avoid drinking, so that you dont keep needing to run to the toilet. But if you dont drink enough, your pee will become more concentrated, which can irritate your bladder and make you need to pee more often
- pace your fluid intake try to drink smaller amounts, regularly throughout the day
- time it right if youre having to get up in the night to pee, try drinking more of your daily fluid intake in the morning
- limit certain drinks caffeinated drinks such as tea and coffee, alcohol and fizzy drinks can increase how much pee you make or irritate your bladder
Some women also find certain foods can irritate their bladder, such as acidic fruits, tomatoes, chocolate and spicy food. You could try cutting these out for a week if you think they could be causing your symptoms. If it makes a difference, try reintroducing them 1 at a time to help you figure out whats causing the problem. Sometimes, just cutting down on something might be enough to help.
Don’t Miss: Loss Of Bladder Control While Coughing
Treatment Of Bladder Spasms
How your doctor treats your bladder spasms depends on what exactly is causing your painful symptoms. But in general, therapy may involve one or more of the following treatments. A combination of treatments often works best.
Botox. Botulinum-A toxin has been shown to reduce nerve-related bladder spasms in children and adults. Botox prevents nerves from releasing chemicals that tell muscles to contract. The Botox is injected directly into the bladder muscle wall.
Change in diet. This may help prevent bladder pain if certain foods and beverages are the culprit behind your spasms. Keeping a food diary, which tracks your meals and your symptoms, can be helpful.
Timed voiding. This involves timed trips to the bathroom to urinate, usually every 1.5 to 2 hours. Timed voiding is especially helpful for children. As the bladder spasms get better and fewer wetting accidents occur, you can extend the time between trips to the bathroom.
Pelvic floor exercises . Kegels and other forms of physical therapy help strengthen the bladder and other muscles that help the body hold in urine. Kegels, combined with biofeedback, are often a good way to help reduce bladder spasms in children. To tighten your pelvic muscles, squeeze your muscles in the same way as if you were trying to stop the flow of urine or prevent yourself from passing gas. Kegel exercises take practice, and tightening the wrong muscles can put more pressure on your bladder. Ask your doctor for specific instructions.
What Causes An Overactive Bladder
The exact cause of an overactive bladder is a mystery. However, several factors are known to contribute to the involuntary contraction of the bladder muscle, improper bladder function, and other symptoms associated with an overactive bladder.
Some nervous system abnormalities that can cause an overactive bladder include:
- Spinal cord injury
Other causes of overactive bladder can include:
- Nerve damage or trauma caused by surgery or certain therapies
- Trauma to the pelvis or abdomen
- Urinary Tract Infection
- Bladder cancer/tumours
- Enlarged prostate
There are also several risk factors that can increase the chances of an overactive bladder. These include:
- Age the risk of overactive bladder increases as you age
- Gender women tend to be more susceptible than men because menstruation, pregnancy and menopause all lead to a rise in oestrogen levels and weaker pelvic floor muscles. For men, an enlarged prostate or damage from prostate surgery can cause an overactive bladder.
- Obesity increased weight puts additional pressure on the bladder.
- Diabetes can affect the nerves that control bladder function.
- Pregnancy causes excess pressure on the bladder.
- Spinal injury damage to the spinal cord can disrupt signals sent to the bladder, causing involuntary contract of bladder muscles.
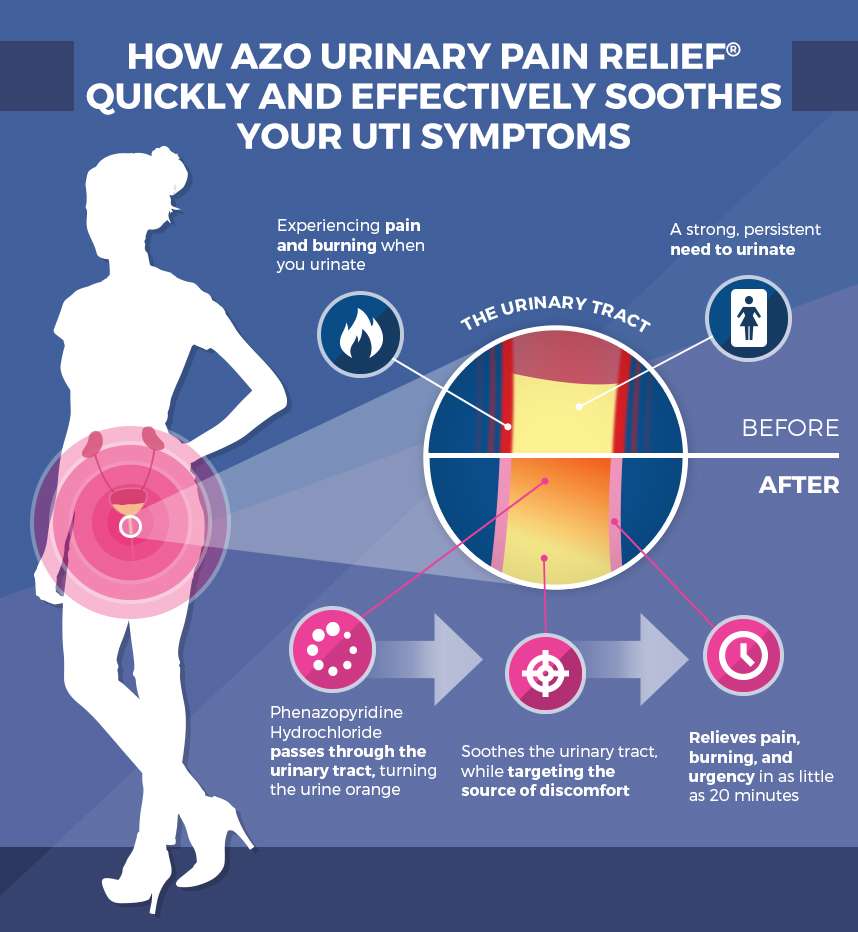
Read Also: What Helps With Bladder Infection Pain
Seven Effective Treatments For Overactive Bladder
Overactive bladder occurs when sudden or frequent urges to urinate become hard to control, and can often lead to leakage .
In order to best treat overactive bladder, a urologist must pinpoint the underlying cause. Treatment will depend on symptom severity and the degree to which they impact someone’s quality of life. In general, there are three approaches to treatment: medication, behavioral interventions, and surgery.
Signs And Symptoms Of Overactive Bladder
Symptoms of overactive bladder vary from person to person, and may include:
- Sudden, urgent need to urinate
- Difficulty holding in urine
- Frequent urination
- Unintentional loss of urine with urgent need to urinate
- Waking up more than once or twice at night to urinate
The defining symptom of overactive bladder is sudden, strong urges to urinate. You may fear that youll leak urine on the way to the bathroom.
Even if you dont actually leak urine, OAB can disrupt your life and may cause significant distress.
You May Like: Why Do I Get Bladder Infections So Easily
How Can Nerve Stimulation Help Overactive Bladder
There are several treatments that involve stimulating your nerves to help improve overactive bladder. Your nerves help communicate the message that your bladder needs to be emptied to your brain. By treating the nerves, your healthcare provider can improve your bladder control. Nerve stimulation is a reversible treatment that is considered when conservative treatments have not worked or have not been tolerated. Conservative treatments include behavioral therapies and medications.
There are several types of nerve stimulation treatments. These can include:
Alternative Treatments To Consider For Oab
Most urologist begin OAB treatment using lifestyle changes, as previously discussed. However, in some individuals, these alterations arent enough to bring lasting relief. If you have tried performing pelvic floor exercises, bladder training, physical therapy, and food and drink control without seeing any results, talk to your doctor about your eligibility for alternative treatments. Two of the best options include InterStim and Botox injections.
Also Check: Causes Of Repeated Bladder Infections
Treatment Options For Overactive Bladder
- Behavioral therapies to help you regain control of their bladder
- Watch the type, quantity and timing of food and drink that you take in
- Avoiding foods and beverages that are likely to cause OAB symptoms
- Regular toileting to prevent the bladder from getting too full
- Weight Loss: Being overweight puts extra pressure on your bladder. Weight loss may help relieve some of the symptoms of OAB.
- Urinate on a Schedule: Sometimes, the message that the bladder is full comes without warning and often too late. In these cases, women find that they lose urine on the way to the bathroom. There isn’t enough time between the message and their ability to get to the bathroom before they start to leak. Voiding on a schedule, also referred to as “Timed Voids” may help prevent urgency and urgency incontinence.
Perspectives Of Treatment And Prevention Of Recurrent Urinary Tract Infection
Treatment of recurrent UTI should follow the following sequence: correct possible LUTD, large PVR, and high voiding pressure behavioral modifications and avoidance of risk factors nonantimicrobial measures and antimicrobial prophylaxis, which should be attempted also in this order. Antimicrobial prophylaxis should be used after nonantimicrobial therapy failure. The antimicrobial prophylaxis can be used continuously for 36 months. For women, a postcoital antimicrobial prophylaxis was effective in the prevention of recurrent UTI. Continuous antimicrobial prophylaxis for 6 or 12 months significantly both reduced the rate of UTIs during treatment failure, but did not differ between groups after cessation of prophylaxis. It is possible that prolonged antimicrobial prophylaxis cannot change the host innate immunity, the underlying pathophysiology of voiding dysfunction, or the urothelial dysfunction due to patients’ bladder condition. Improvement of patient’s barrier function and decrease of chronic bladder inflammation might be more helpful than antimicrobial prophylaxis.
Recommended Reading: Bladder Control Problems At Night