What Are The Non
Changing from BCG to the following options can yield responses in selected cases with BCG-unresponsive disease. In the EAU Guidelines , it is stated that treatments other than RC must be considered oncologically inferior in this setting .
-
Further BCG therapy or related agents Patients with BCG-unresponsive NMIBC are unlikely to respond to further BCG therapy. However, there are still lines of research using modified protocols:
-
BCG plus interferon-alpha The US national Phase II multicenter trial for BCG plus interferon-alpha intravesical therapy for NMIBC showed that those with disease recurrence more than 1 year after BCG treatment had response rates similar to those of BCG naive patients . The contribution of IFN-alpha in the outcomes is unknown as there were no BCG-only arm. The same conclusions were drawn in a study focusing on CIS-only patients . However, BCG plus IFN-alpha in general did not demonstrate a significant benefit versus BCG alone in the long term. A systematic Cochrane review evaluated intravesical BCG versus intravesical BCG with IFN-alpha for treating NMIBC . They found low-quality evidence suggesting:
-
No clear differences in recurrence or progression with BCG plus IFN-
-
Increased time-to-recurrence when BCG is alternated with IFN-.
Additional high-quality, adequately powered well-conducted trials are needed to provide a more solid conclusion.
-
Nivolumab+BMS-986205 and CheckMate 7G8
Other targeted therapies
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
Guideline Statement 24
Discussion
Guideline Statement 25
Discussion
Guideline Statement 26
Selecting And Testing Gemcitabine
When Dr. Messing began research on gemcitabine as a possible way to reduce recurrences more than a decade ago, the drug was not widely used for bladder cancer. “We tried to pick an agent that we thought would be safe and effective,” he said.
The researchers decided to compare gemcitabine against placebo rather than mitomycin C, based on studies showing how infrequently patients received some form of chemotherapy following surgery despite guidelines recommending this approach.
“If the new procedure were adopted widely, we could spare patients a lot of suffering from repeated surgeries and save health care costs associated with those surgeries,” Dr. Messing said.
“Now that we have the results of the trial,” he went on, “we hope that patients and physicians will embrace this approach to treatment.”
Don’t Miss: Blue Light Test For Bladder Cancer
Failure Of Bcg Contact With The Target
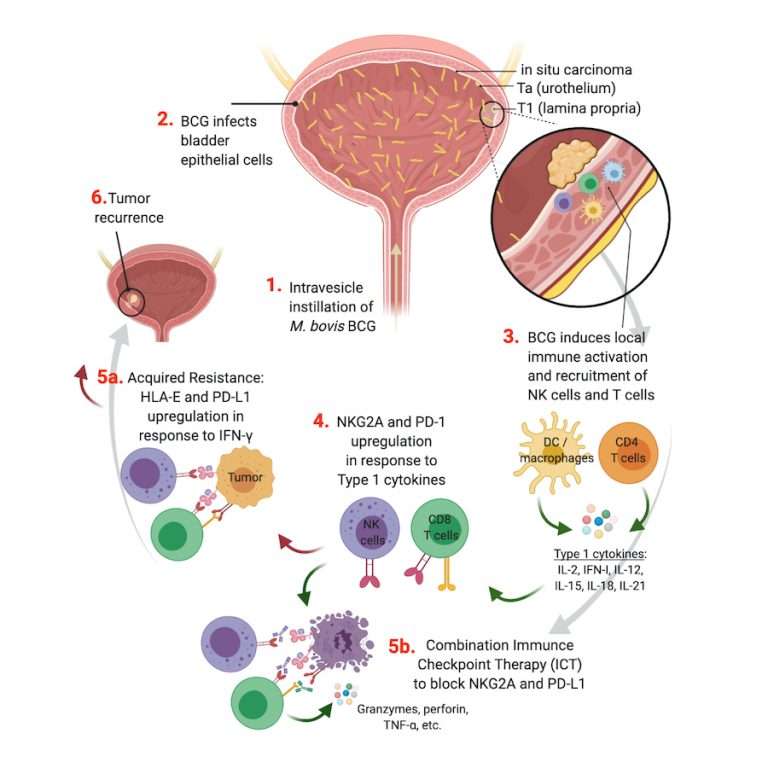
Gradual waning of the immune response. Intravesical BCG instillations induce a transient peripheral immune activation against BCG antigens. Reactivation is observed in most cases after additional BCG courses. The absence of long-lasting immune activation after a single 6-week course of BCG could be related to the increased clinical efficacy observed with BCG maintenance instillations.12,13,14
Inadequate immune response. There is strong evidence that the success of BCG therapy might be due to a preferential induction of a TH-1 response .15,16 Although somewhat controversial, TH-2 responses detected either in the peripheral circulation or locally in the bladder are associated with poorer outcomes and might explain failure to respond to BCG therapy.17
Natural resistance-associated macrophage protein gene polymorphisms. The NRAMP1 gene has been implicated in susceptibility to infectious diseases and in response to BCG. Data suggest implication of the NRAMP1 gene in bladder cancer recurrence and response to BCG.18
Unresponsive tumour. Many recent investigations have determined whether biological markers might predict disease progression and/or response to treatment.19 An excellent review was provided a couple of years ago by Saint and colleagues.20
What Causes Bladder Cancer
Bladder cancer occurs when cells within the lining of the bladder wall begin to grow in a disordered, uncontrolled way.
Exactly what prompts this disordered growth is not fully known. However, several factors associated with a higher risk of bladder cancer have been identified, including:
- Age most people diagnosed with bladder cancer are older than 55 years.
- Sex compared to women, men are 4 times more likely to develop bladder cancer.
- Smoking smoking is associated with around half of all bladder cancers in men and women.
- Race in the United States, White Americans have the highest rate of bladder cancer.
- Previous bladder cancer people who have had bladder cancer may have a recurrence.
- Workplace exposures certain chemicals in some workplaces may contribute to higher rates of bladder cancer in workers. For example, painters, hairdressers, and truck drivers are at increased risk.
- Arsenic in drinking water.
- Certain types of medication.
Also Check: Treatment Of Muscle Invasive Bladder Cancer
Treatment Of Failure Of Intravesical Therapy
7.6.1. Recurrence during or after intravesical chemotherapy
Patients with NMIBC recurrence during or after a chemotherapy regimen can benefit from BCG instillations. Prior intravesical chemotherapy has no impact on the effect of BCG instillations .
7.6.2. Treatment failure after intravesical BCG immunotherapy
Several categories of BCG failures, broadly defined as any HG disease occurring during or after BCG therapy, have been proposed . Non-muscle-invasive BC may not respond at all or may relapse after initial response . Some evidence suggests that patients with BCG relapse have better outcomes than BCG refractory patients .
To be able to specify the subgroup of patients where additional BCG is unlikely to provide benefit, the category of BCG-unresponsive tumour was defined. Further BCG instillations in these patients are associated with an increased risk of progression . The category of BCG-unresponsive tumours comprises BCG-refractory and some of BCG-relapsing tumours . The definition was developed in consultation with the U.S. Food and Drug Administration , in particular to promote single-arm trials to provide primary evidence of effectiveness in this setting .
Non-HG recurrence after BCG is not considered as BCG failure.
Table 7.2: Categories of high-grade recurrence during or after BCG
7.6.3. Treatment of BCG-unresponsive tumours, late BCG-relapsing tumours, LG recurrences after BCG treatment and patients with BCG intolerance
|
Summary of evidence |
Cystectomy Remains The Standard Option For Patients With Bcg
No established and effective intravesical therapies are available for patients whose tumors recur after BCG, representing a clinically important unmet need. Radical cystectomy provides cancer eradication in a significant number of HG NMIBC cases . In the series of Stein and coworkers , the 10-year recurrence-free survival for patients with lymph node-negative tumors was 86% for T0, 89% for Tis, 74% for Ta, and 78% for T1 tumors. Several studies since have shown the advantage of performing early cystectomy in high-risk NMIBC patients, particularly in the case of BCG failure. It remains the standard of care in the case of BCG-unresponsive patients following adequate BCG treatment .
However many patients are elderly, have significant comorbidities with a diminished performance status, and/or are unwilling to undergo radical extirpative surgery.
You May Like: What Happens When A Bladder Infection Goes Untreated
Bladder Cancer Recurrence: A Persistent Fear For Patients
- Reactions 0 reactions
One of the hardest parts of living with bladder cancer is dealing with the risk of recurrence. For some, recurrences pop up every few months or years, and the relief of being “cancer-free” is short-lived. For others, bladder cancer is diagnosed, treated, and the person remains in remission but the fear that it could come back looms overhead. For others still, remission has yet to be achieved.
No matter your experience, there are similar worries, milestones, and ways of coping. Our Bladder Cancer In America 2019 survey found the many ways by which bladder cancer recurrences affect our community.
Cost Issues And Follow
Finally there is a cost issue with bladder cancer and follow-up. Leal et al. looked at the economic costs of bladder cancer across the European Union . These were 4.9 billion in 2012, of which health care costs were 2.9 billion , productivity loss 1.1 billion and informal care costs 0.9 billion . Bladder cancer costs represented 5% of total health care cancer costs and 3% of all cancer costs in the EU in 2012. Of note, difference between the least and most expensive country was> tenfold. For follow-up costs, all three fields play a role. Interestingly, Mossanen et al. used a Markow model to specifically evaluate costs of surveillance of NMIBC Their index patient was a compliant 65-year-old male, and they used four health states: no evidence of disease, recurrence, progression/cystectomy and death. The cumulative costs over a 5-year period were USD 52,125, 146,250 and 366,143 for low-, intermediate- and high-risk, respectively. Costs for recurrence were highest in the low-risk group, but still not more than 8% of the total costs of low risk. Progression and subsequent treatment results in much higher costs , even when not frequent in low-risk patients.
In all, there is certainly an opportunity to reduce patient burden and costs in an adapted follow-up strategy with a marker with a high NPV, where the financial benefit obviously depends on the price of the marker. Prospective studies will be necessary to validate these assumptions on national levels.
Don’t Miss: What Is T1 High Grade Bladder Cancer
Ask Your Doctor For A Survivorship Care Plan
Talk with your doctor about developing a survivorship care plan for you. This plan might include:
- A suggested schedule for follow-up exams and tests
- A schedule for other tests you might need in the future, such as early detection tests for other types of cancer, or tests to look for long-term health effects from your cancer or its treatment
- A list of possible late- or long-term side effects from your treatment, including what to watch for and when you should contact your doctor
- Diet and physical activity suggestions
- Reminders to keep your appointments with your primary care provider , who will monitor your general health care.
Development Of Therapeutic Bcg For Bladder Cancer
The anti-tumor potential of BCG was first noted in 1929 when an autopsy series by Pearl noted a lower rate of cancer in patients who had tuberculosis . Around the same time, Holmgren also published a description of the anti-neoplastic nature of BCG. Further studies of BCG revealed its ability to retard transplanted tumor growth, first in mice systemically infected with BCG and later with direct injection of BCG into the tumor . This work also specifically found that close contact between BCG and the tumor was needed for efficacy. A later study by Bast determined that a lower tumor burden led to improved treatment efficacy . With these studies in mind, Morales surmised that instilling BCG into the bladder via a catheter, the same route utilized for thiotepa, after TURBT, would allow for similar BCG-tumor direct contact. He began recruiting patients for his research in 1972.
Recommended Reading: How Do You Fix Nerve Damage In The Bladder
Any Recurrence After Bcg And Diet For Bladder Caner
My husband was diagnosed as pT1 G3 . Age 56
1. First TURBT 16 Feb 2017. 25 mm tumour. Second TURBT 30 March 2017 – small recurrence on scar this time Grade 2.
He’s had 6 BCG followed by 3 maintenance. His last BCG was 31 July. October cystoscopy showed ”there where some areas of telangiectasia radiating from the posterior wall visualised”.20 November last year he had TURBT number three and there was no recurrent tumour and all his biopsies were negative.However after this third TURBT he suffered severe urinary retention and because of Christmas he still has the catheter in. We saw his consultant as QE Birmingham yesterday and were given the options of continue with BCG or neo bladder. My husband has decided to continue with BCG – obviously once they sort out the catheter issue. Has anyone had a recurrence after ongoing BCG treatment?The consultant said there was 30% change of recurrence – which we both took as a 70% success rate of no recurrence. Also has anyone changed their diets or taken supplements, herbs etc to improve their chances of beating BC ?
High Grade T1 Disease

In any patient with T1HG disease, re-resection must be performed. This identifies the 2940% of patients that will be upstaged to muscle-invasive disease , thus requiring more radical intervention, and ensures complete tumor resection to maximize the effect of adjuvant therapy. One study demonstrated that re-resection itself reduces the rate of recurrence but not progression , likely a result of a more complete resection. In those with confirmed T1HG disease after re-resection, pooled group analysis of multiple small studies identifies a progression rate of 27.2% in patients treated with BCG induction alone , while those treated with induction and maintenance had a 19.0% progression rate . Recently, a large multicenter retrospective individual patient data analysis of 2451 patients reported a progression rate of 19% at a median of 5.2 years follow-up.
In reviewing unpublished data from the National Phase 2 BCG/IFN study, 61 BCG failure patients with recurrent T1 disease were identified, of which 51% were disease-free at 1 year and 38% at 2 years . While this demonstrated a good response to therapy, we caution over-interpretation of this data, given the small number of patients and unknown rate of progression in the group.
You May Like: Does Uti Cause Bladder Leakage
Possible Side Effects Of Bcg
There are a number of things you can do to manage the side effects of BCG. Talk to your care team about these recommendations. They can help you decide what will work best for you. These are some of the most common or important side effects:
Bladder Irritability
This medication can cause irritation to the bladder, including difficulty or painful urination , blood in the urine , and increased urgency , or frequency of urination. Patients are advised to increase fluid intake after administration of this medication to âflushâ the bladder. You should report any of the urinary symptoms listed above that last more that 48 hours to your healthcare team for further management instructions.
Fatigue
Fatigue is very common during cancer treatment and is an overwhelming feeling of exhaustion that is not usually relieved by rest. While on cancer treatment, and for a period after, you may need to adjust your schedule to manage fatigue. Plan times to rest during the day and conserve energy for more important activities. Exercise can help combat fatigue a simple daily walk with a friend can help. Talk to your healthcare team for helpful tips on dealing with this side effect.
Flu-like Symptoms
Your doctor or nurse can recommend medication and other strategies to relieve aches, pains, and generalized malaise.
BCG Infection Reaction
What Are The Side Effects
Some patients have difficulty completing long-term BCG therapy because of irritation in the bladder.2 To help with this irritation, the treatment frequency may be adjusted to give you a longer break between treatments. You may not notice any reaction after the first few BCG treatments. After the third treatment, patients usually start to experience bladder irritation pain or burning during urination, joint pain, fatigue, and flu-like symptoms that can last a few days. Most symptoms and side effects can be treated with over-the-counter pain medicines.
While BCG is a fairly common treatment for bladder cancer, every person has different experiences. Itâs important to talk to your doctor about any questions or concerns you may have at any point during your treatment. Being mentally prepared for what to expect can help to reduce stress or uncertainty about treatment or help you think of additional questions for your healthcare team.
Don’t Miss: Pain When My Bladder Is Full
Predictive Markers For The Recurrence Of Nonmuscle Invasive Bladder Cancer Treated With Intravesical Therapy
Yasuyoshi Miyata
1Department of Urology and Renal Transplantation, Nagasaki University Hospital, 1-7-1 Sakamoto, Nagasaki 852-8501, Japan
Academic Editor:
Abstract
High recurrence rate is one representative characteristic of bladder cancer. Intravesical therapy after transurethral resection is often performed in patients with nonmuscle invasive bladder cancer to prevent recurrence. Bacillus Calmette-Guérin and several anticancer/antibiotic agents, such as mitomycin C and epirubicin, are commonly used for this therapy. BCG treatment demonstrates strong anticancer effects. However, it is also characterized by a high frequency of adverse events. On the other hand, although intravesical therapies using other anticancer and antibiotic agents are relatively safe, their anticancer effects are lower than those obtained using BCG. Thus, the appropriate selection of agents for intravesical therapy is important to improve treatment outcomes and maintain the quality of life of patients with NMIBC. In this review, we discuss the predictive value of various histological and molecular markers for recurrence after intravesical therapy in patients with NMIBC.
1. Introduction
2. Clinical Background and Pathological Features
3. Cell Proliferation
| 2015/ |
4. Apoptosis and Apoptosis-Related Molecules
4.1. TP53
4.2. p63
4.3. Survivin
4.4. Bcl-2 Family
5. Angiogenesis and Angiogenesis-Related Molecules
6. Other Cancer-Related Molecules
7. Immune System
| Variable |
7.2. Tumor-Associated Macrophage
Intermediate Risk Early Bladder Cancer
People with intermediate-risk non-muscle-invasive bladder cancer should be offered a course of at least 6 doses of chemotherapy. The liquid is placed directly into your bladder, using a catheter, and kept there for around an hour before being drained away.
You should be offered follow-up appointments at 3, 9 and 18 months, then once every year. At these appointments, your bladder will be checked using a cystoscopy. If your cancer returns within 5 years, youll be referred back to a specialist urology team.
Some of the chemotherapy medicine may be left in your urine after treatment, which could severely irritate your skin.
It helps if you sit down to urinate and that youre careful not to splash yourself or the toilet seat. Always wash the skin around your genitals with soap and water afterwards.
If youre sexually active, its important to use a barrier method of contraception, such as a condom. This is because the medicines may be present in your semen or vaginal fluids, which can cause irritation.
You also shouldnt try to get pregnant or father a child while having chemotherapy for bladder cancer, as the medicines can increase the risk of having a child with birth defects.
Read Also: What Should I Do If I Have A Bladder Infection