Predictive Factors For Residual Hg Disease At Retur
On univariable analysis, predictive factors for residual HG disease at reTUR were size> 3 cm , multifocality , concomitant CIS , NLR> 3 and BMI . On multivariable analysis, size > 3 cm , concomitant CIS , overweight and obesity status according to BMI remained as significant independent predictors for HG residual disease at reTUR .
Table 1
Association of HG/G3 on reTUR with clinical and pathologic characteristics of 1155 patients after primary T1 HG/G3 NMIBC
| All patients |
|---|
TURBT: transurethral resection of bladder tumor, OR: Odds ratio, CI: Confidence interval
Prognostic Nomogram For Os
As Table 3 shows, six models were constructed by incorporating variables progressively. The model 6 including the most C-index and AUC was defined the most ideal model. The prognostic nomogram predicting 3- and 5-year OS probability was established based on all significant factors using 561 patients from the development group . N stage and age contributed most to the prognosis of OS, as Figure 3 shows.
|
Table 3 Results of Sensitivity Analysis by Enter Factor Gradually |
|
Figure 3 Nomogram predicting 3- and 5-year bladder overall survival probability for T1HG patients after radical cystectomy. Variables include age, marital status, tumour size, tumour site, region nodes examined, N stage. Use: locate patient values at each axis. Draw a vertical line to the Pointaxis to determine how many points are attributed for each variable value. Sum the points for all variables. Locate the sum on the Total Points line. Draw a vertical line towards the 3Yrs.Surv. Prob. and 5Yrs. Surv. Prob, Prob. axes to determine respectively the 3-, and 5-year survival probabilities. |
Validation Of The Nomogram
Internal validation was performed for the nomogram of OS. The C-index of the nomogram was 0.732 in the development group and 0.752 in the validation group. It was significantly higher than that of the AJCC stage, which was 0.590 and 0.559, respectively. The calibration curve in the development and validation group showed good agreement between actual observations and predicted outcomes in the probability of 3-year and 5-year survival . Meanwhile, ROC curves were used to investigate the discriminative ability of the model . The 3-year and 5-year AUC in the development group was higher than that of the AJCC stage . A similar condition was also seen in the validation group . All these results suggested that the nomograms better predictive performance was confirmed compared with the traditional AJCC staging system.
|
Figure 4 The development group. Calibration plots of the nomogram for 5-year calibration plots of the nomogram for 3-year. |
|
Figure 5 The validation group. Calibration plots of the nomogram for 3-year calibration plots of the nomogram for 5-year. |
|
Figure 6 ROC curves of the nomogram predicting 3-year OS of the development group ROC curves of the nomogram predicting 5-year OS of the development group. Abbreviation: ROC, receiver operating characteristic. |
|
Figure 7 ROC curves of the nomogram predicting 3-year OS of the validation group ROC curves of the nomogram predicting 5-year OS of the validation group. Abbreviation: ROC, receiver operating characteristic. |
Read Also: Does Azo Bladder Control Cause Weight Gain
Treatment Of Bcg Unresponsive Tumours Late Bcg
Patients with BCG unresponsive disease are unlikely to respond to furtherBCG therapy RC is therefore the standard and preferred option. Currently, several bladderpreservation strategies are being investigated such as cytotoxic intravesical therapies , device assisted instillations intravesical immunotherapy , systemic immunotherapy or gene therapy .
A phase III RCT including predominantly high-risk NMIBC patients failing atleast a previous induction course of BCG, MMC combined with microwave-induced hyperthermiaprovided 35% overall DFS at 2 years as compared to 41% in the control arm . In the pre-planned sub-analysis, MMC and microwave-induced thermotherapyshowed lower response rates in CIS recurrences but higher DFS in non-CIS papillary tumours . Recently, the systemic immunotherapeutic drugpembrolizumab was granted FDA approval based on currently unpublished data . Promising data from a phase III multicentre RCT withintravesical nadofaragene firadenovec were published recently showing a complete response in53.4% in patients with BCG-unresponsive CIS .
At the present time, treatments other than RC are considered oncologicallyinferior in patients with BCG unresponsive disease . Various studies suggestthat repeat-BCG therapy is appropriate for non-high-grade and even for some high-graderecurrent tumours namely those relapsing beyond one year after BCG exposure .
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
Guideline Statement 24
Discussion
Guideline Statement 25
Discussion
Guideline Statement 26
Don’t Miss: Bladder Leakage Only At Night
Treatment Decision Strategy Based On Risk Factors
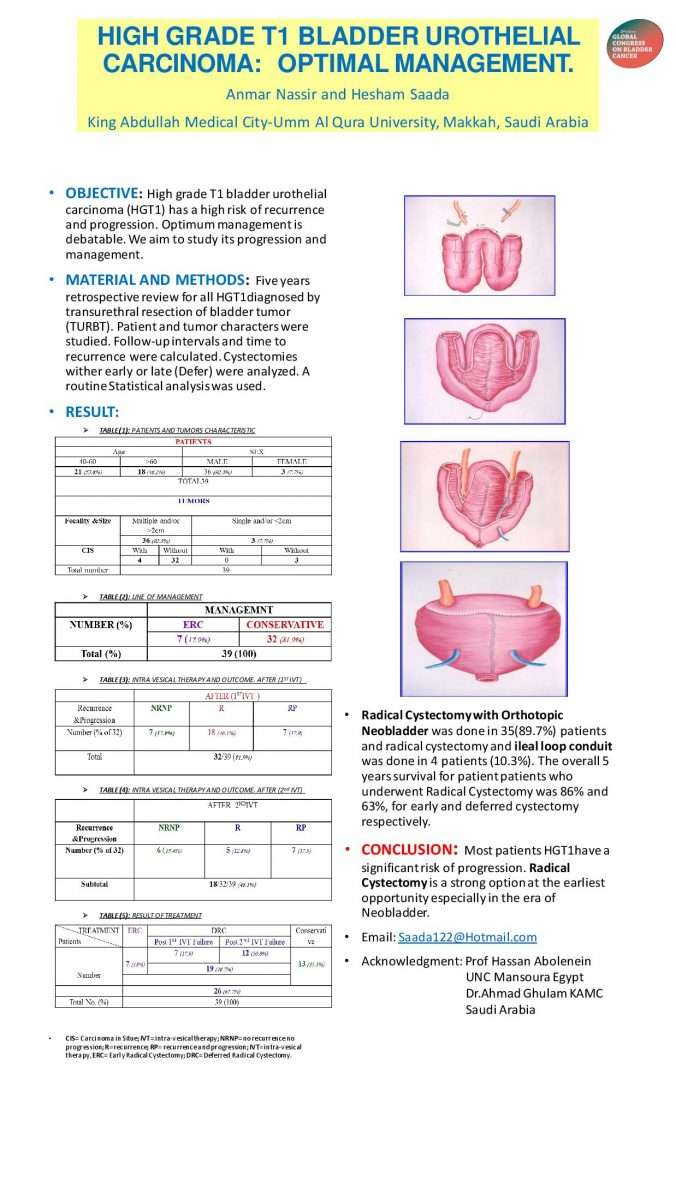
Kitamura and Kakehi suggested that optimal management strategies should be based on pathological findings from second TUR specimens in patients with T1 disease. They recommended that patients with T0 upon second TUR be considered for BCG therapy or watchful waiting. A randomized controlled study is ongoing comparing watchful waiting to BCG therapy in high-grade T1 disease with T0 on second TUR . In cases of Ta or T2 on second TUR, unarguably patients should undergo BCG therapy or cystectomy, respectively. In the case of T1 on second TUR, however, questions remain as to which treatment is the optimal treatment for high-grade T1 disease . Such approaches are reasonable to select optimal treatment. However, if molecular risk classifiers for predicting progression or BCG response are included, it may help select treatment modalities for high-grade T1 patients, although they require validation in multiple large scale cohorts. Fig. 4 illustrates a proposed algorithm for treatment decision-making in high-grade T1 bladder cancer.
Proposed algorithm for decision-making in high-grade T1 bladder cancer. TUR, transurethral resection CIS, carcinoma in situ BCG, bacillus Calmette-Guérin.
Strategy Of The Procedure
The goal of TURB in TaT1 BC is to make the correct diagnosis and completelyremove all visible lesions. It is a crucial procedure in the management of BC. Transurethralresection of the bladder should be performed systematically in individual steps .
The operative steps necessary to achieve a successful TURB includeidentifying the factors required to assign disease risk , clinical stage , adequacy of the resection , and presence of complications . To measure the size of thelargest tumour, one can use the end of cutting loop, which is approximately 1 cm wide as areference. The characteristics of the tumour are described as sessile, nodular, papillary orflat.
Don’t Miss: Long Term Side Effects Of Bcg Treatment For Bladder Cancer
Ajcc Stage Groupings And Tnm Definitions
The American Joint Committee on Cancer has designated staging by TNM classification to define bladder cancer.
| Stage |
|---|
References
Donât Miss: How To Prevent Bladder Infections In Cats
Information Sources And Study Selection
Studies were identified by searching Ovid MEDLINE for the period 1946 to November 2013 , the Cochrane library , Google Scholar , NHS Evidence . An example search strategy was shown in Figure 1, which indicates the keywords used.
Fig. 1
Search strategy.
In addition, reference lists of relevant articles were searched to identify other relevant studies . For articles that did not have a complete electronic version of the full text available, the article was requested from the British Library Document Supply Service 2 articles were obtained through this means.
Also Check: Men’s Overactive Bladder Treatment
Summary Of Evidence And Guidelines Forstratification Of Non
|
Summary of evidence |
|
|
The EAU NMIBC 2021 scoring model and risk tablespredict the short- and long-term risks of disease progression in individualpatients with primary NMIBC using either the WHO 1973 or the WHO 2004/2016classification system . |
|
|
The 2006 EORTC scoring model and risk tables predictthe short- and long-term risks of disease recurrence and progression inindividual patients with NMIBC using the WHO 1973 classification system . |
|
|
Patients with TaG1/G2 tumours receiving chemotherapyhave been further stratified into three risk groups for recurrence, taking intoaccount the history of recurrences, history of intravesical treatment, tumourgrade , number of tumours and adjuvant chemotherapy . |
2a-b |
|
In patients treated with 5 to 6 months of BCG, theCUETO scoring model predicts the short- and long-term risks of diseaserecurrence and progression using the WHO 1973 classification system . |
|
|
In patients receiving at least 1 year of BCGmaintenance prior recurrence rate and number of tumours are the most importantprognostic factors for disease recurrence. Stage and grade are the mostimportant prognostic factors for disease progression and disease-specificsurvival patient age and grade are the most important prognosticfactors for overall survival . |
Understanding The Statistics: Cancer Survival
It is important to remember that all cancer survival numbers are based on averages across huge numbers of people. These numbers cannot predict what will happen in your individual case.
Survival rates will not tell you how long you will live after you have been diagnosed with bladder cancer. But, these numbers can give you an idea of how likely your treatment will be successful. Also, survival rates take into account your age at diagnosis but not whether you have other health conditions too.
Don’t Miss: What Kind Of Doctor Does Bladder Prolapse Surgery
Scoringmodel Using The Who 2004/2016 And Who 1973 Classification Systems
6.1.2.1.EAU NMIBC 2021 scoring model
To update the risk of disease progression and create new prognostic factorrisk groups using both the WHO 1973 and WHO 2004/2016 classification systems , individual patient data from 3,401 primary patients treated from1990 to 2018 were used . Only patients treatedwith TURB +/- intravesical chemotherapy were included, those treated with adjuvantintravesical BCG were excluded because BCG may reduce the risk of disease progression. Fromthe multivariate analysis, tumour stage, WHO 1973 grade, WHO 2004/2016 grade, concomitantCIS, number of tumours, tumour size and age were independent predictors of diseaseprogression .
This is the only available model, where the WHO 2004/2016 classificationsystem is included as one of parameters to calculate an individual patients riskgroup and probability of progression. As the WHO 2004/2016 classification system is the maingrading classification system used by pathologists, the Guidelines Panel recommends to usethe 2021 EAU NMIBC scoring model for risk groups definition .
As the 2021 EAU NMIBC scoring model determines the riskof tumour progression, but not recurrence, any of models mentioned in Section 6.1.1 may beused for calculation of an individuals risk of disease recurrence.
Bladder Cancer And Its Stages
Bladder cancer is a disease that can have varying symptoms and severity according to its stage. The estimated life expectancy of people who are diagnosed with bladder cancer is dependent on their condition and treatment.
The stages of bladder cancer have different levels of effects to the patient. Although living with bladder cancer can be difficult and challenging, do not lose hope as some of the stages of bladder cancer can be treated.
If people with bladder cancer receive treatment early on the first stage of cancer, the symptoms can be neutralized. The stages of bladder cancer usually depend on the formation of cancer in other parts of the body. If the first stage is managed early, the spread of cancer can be stopped.
Also Check: Can A Bladder Infection Turn Into A Kidney Infection
Scoringmodels Using The Who 1973 Classification System
6.1.1.1.The 2006 European Organisation forResearch and Treatment of Cancer scoring model
To be able to predict both the short- and long-term risks of diseaserecurrence and progression in individual patients, the EORTC Genito-Urinary Cancer Grouppublished a scoring system and risk tables based on the WHO 1973 classification in 2006 . The scoring system is based on the six most significantclinical and pathological factors in patients mainly treated by intravesical chemotherapy:
- Number of tumours
- Concurrent CIS
- WHO 1973 tumour grade.
Using the 2006 EORTC scoring model, individual probabilities of recurrenceand progression at one and five years may be calculated.
6.1.1.2.The model for patients with TaG1/G2 tumours treated with chemotherapy
Patients with TaG1/G2 tumours receiving chemotherapy were stratified intothree risk groups for recurrence, taking into account the history of recurrences, history ofintravesical treatment, tumour grade , number of tumours and adjuvant chemotherapy.
6.1.1.3.Club Urologico Español deTratamiento Oncologico scoring model for BCG-treated patients
- gender
- associated CIS
- WHO 1973 tumour grade.
6.1.1.4.The 2016 EORTC scoring model forpatients treated with maintenance BCG
Cellular Classification Of Bladder Cancer
More than 90% of bladder cancers are transitional cell carcinomas derived from the uroepithelium. About 2% to 7% are squamous cell carcinomas, and 2% are adenocarcinomas. Adenocarcinomas may be of urachal origin or nonurachal origin the latter type is generally thought to arise from metaplasia of chronically irritated transitional epithelium. Small cell carcinomas also may develop in the bladder. Sarcomas of the bladder are very rare.
Pathologic grade of transitional cell carcinomas, which is based on cellular atypia, nuclear abnormalities, and the number of mitotic figures, is of great prognostic importance.
References
You May Like: Prostate And Bladder Cancer Survival Rate
You May Like: How Effective Is Immunotherapy For Bladder Cancer
Detection Of Residual Disease And Tumour Upstaging
The significant risk of residual tumour after initial TURB of TaT1 lesionshas been demonstrated .
A SR analysing data of 8,409 patients with Ta or T1 HG BCdemonstrated a 51% risk of justify persistence and an 8% risk of under-staging in T1tumours. The analysis also showed a high risk of residual disease in Ta tumours, but thisobservation was based only on a limited number of cases. Most of the residual lesions weredetected at the original tumour location .
Another meta-analysis of 3,556 patients with T1 tumoursshowed that the prevalence rate of residual tumours and upstaging to invasive disease afterTURB remained high in a subgroup with detrusor muscle in the resection specimen. In thesubgroup of 1,565 T1 tumours with detrusor muscle present, persistent tumour was found in58% and under-staging occurred in 11% of cases .
Treating Bladder Cancer That Progresses Or Recurs
If cancer continues to grow during treatment or comes back after treatment , treatment options will depend on where and how much the cancer has spread, what treatments have already been used, and the patient’s overall health and desire for more treatment. Its important to understand the goal of any further treatment if its to try to cure the cancer, to slow its growth, or to help relieve symptoms as well as the likely benefits and risks.
For instance, non-invasive bladder cancer often comes back in the bladder. The new cancer may be found either in the same place as the original cancer or in other parts of the bladder. These tumors are often treated the same way as the first tumor. But if the cancer keeps coming back, a cystectomy may be needed. For some non-invasive tumors that keep growing even with BCG treatment, and where a cystectomy is not an option, immunotherapy with pembrolizumab might be recommended.
Cancers that recur in distant parts of the body can be harder to remove with surgery, so other treatments, such as chemotherapy, immunotherapy, targeted therapy, or radiation therapy, might be needed. For more on dealing with a recurrence, see Understanding Recurrence.
Read Also: Lemon Juice For Bladder Infection
The Rational And Benefits Of The Second Look Transurethral Resection Of The Bladder For T1 High Grade Bladder Cancer
Francesco Soria1,2, Giancarlo Marra2, David DAndrea1, Paolo Gontero2, Shahrokh F. Shariat1,3,4,5 on behalf of the EAU Young Academic UrologistsUrothelial Cancer Working party
1Department of Urology and Comprehensive Cancer Center, Medical University of Vienna 2Division of Urology, Department of Surgical Sciences, San Giovanni Battista Hospital, University of Studies of Torino , Karl Landsteiner Institute of Urology and Andrology , 4Department of Urology, Weill Cornell Medical College, New York Presbyterian Hospital University of Texas Southwestern Medical Center , USA .
Contributions: Conception and design: F Soria, SF Shariat Administrative support: None Provision of study material or patients: None Collection and assembly of data: F Soria, G Marra, D DAndrea Data analysis and interpretation: None Manuscript writing: All authors Final approval of manuscript: All authors.
Correspondence to:
Keywords: Re-TUR second look transurethral resection of the bladder T1HG non-muscle invasive bladder cancer
Submitted Aug 10, 2018. Accepted for publication Oct 22, 2018.
doi: 10.21037/tau.2018.10.19