Role Of Antibiotics And Catheter Materials
Antibiotic Prophylaxis Is There a Role?
Much like the role of urethral stenting in hypospadias repair, there is substantial variation in practice methods amongst pediatric urologists with regards to antibiotic prophylaxis with urinary catheterization and minor lower urinary tract procedures. Although guidelines exist, these are geared toward the adult urologic patient.
To address this chasm, in 2017, Glaser and associates surveyed members of the Society for Pediatric Urology regarding antibiotic use with catheterization. A significant majority, 78%, prescribed daily prophylaxis with a hypospadias stent in place, but disagreement abound thereafter. Interestingly, urologists over 50 years and fellowship-trained pediatric urologists were more likely to prescribe prophylaxis for hypospadias stents. Extensive variation existed with prophylaxis for Foley catheters, percutaneous nephrostomy tubes, suprapubic tubes and internal doublej ureteral stents, with 3050% of respondents not prescribing prophylaxis for these drainage systems. Additionally, the majority of respondents do not routinely prescribe a dose of prophylaxis prior to tube removal aside from removal of a ureteral stent.42
Catheter Coatings
Slide : Prepping For Catheter Insertion Procedure3
- Cleanse hands and don gloves
- Get your buddy to help at the bedside
- Place resident in the supine position
- For a femaleapply topical lidocaine jelly if needed for comfort
- Inspect catheter kit and remove it from its outer packaging to form a sterile field
- Remove gloves and wash hands!
3. Willson M, Wilde M, Webb M, et al. Nursing interventions to reduce the risk of catheterassociated urinary tract infection: part 2: staff education, monitoring, and care techniques. J Wound Ostomy Continence Nurs. 2009 36:137-54. PMID: 19287262.
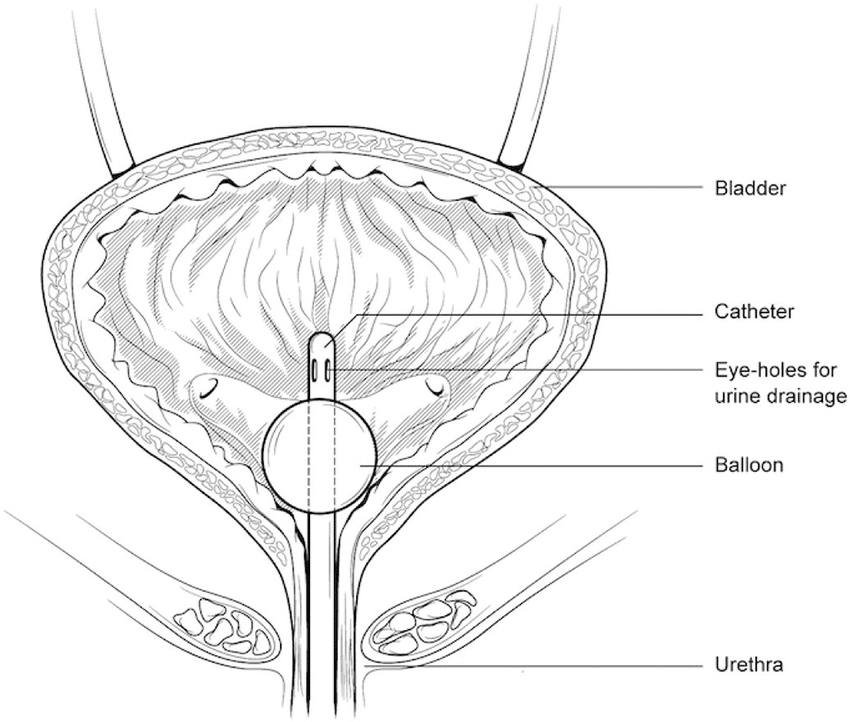
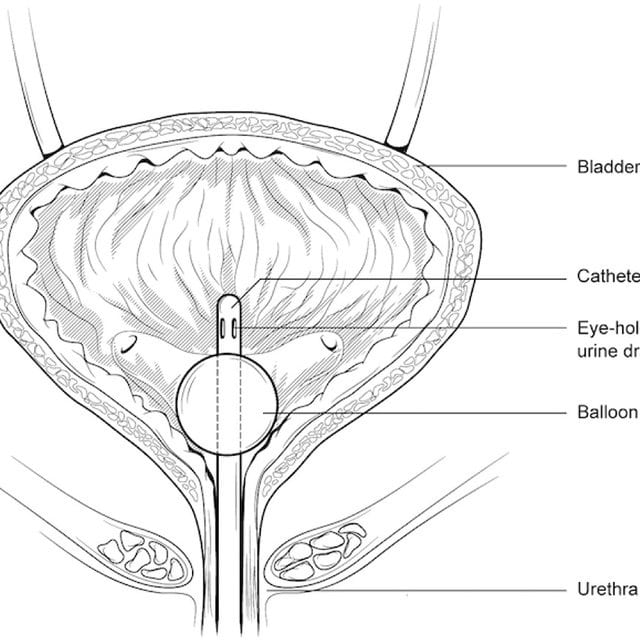
Slide : Indwelling Urinary Catheters1
Images: Figure l. Routes of entry of uropathogens to catheterized urinary tract.An image depicts the male and female lower urinary tract system, and the difference in placement of a catheter in the bladder.
Source: Maki DG, Tambyah PA. Engineering out the risk of infection with urinary catheters. Emerg Infect Dis. 2001 Mar-Apr 7:342-7.*CMS, State Operations Manual, 2014.
1. Maki DG, Tambyah PA. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001 7:342-7. PMID: 11294737.
You May Like: How To Stop Bladder Leakage When Running
What Medications Treat A Prolapsed Bladder
- In mild cases of prolapsed bladder, estrogen may be prescribed in an attempt to reverse bladder prolapse symptoms, such as vaginal weakening and incontinence. For more severe degrees of prolapse, estrogen replacement therapy may be used along with other types of treatment.
- Estrogen can be administered orally as a pill or topically as a patch or cream. The cream has very little systemic absorption and has a potent effect locally where it is applied.
- Topical administration has less risk than the oral preparations.
Why Might I Need To Use A Catheter

There are many reasons why you may need to have a catheter. Some reasons include:
- bladder problems
- problems with the nerves controlling the bladder. For example, if you have a spinal injury
- urinary retention
- during labour and childbirth if an epidural has been used
- some types of bladder tests and treatments
- having certain types of surgery
- people who are very unwell in hospital
Also Check: How To Get Relief From A Bladder Infection
Slide : Hygiene And Standard Precautionscatheter Insertion Procedure23
- Don sterile gloves.
- Cover resident’s lower abdomen and upper thighs with dignity cover.
- Organize contents of tray on sterile field
- Pour antiseptic solution over swabs in tray compartment.
- Squeeze sterile catheter lubricant onto tray.
2. Gould CV, Umscheid CA, Agarwal RK, et al. Centers for Disease Control and Prevention. Guidelines for prevention of catheter-associated urinary tract infections 2009. Atlanta, GA: US Department of Health and Human Services, CDC 2009. Accessed January 28, 2016.3. Willson M, Wilde M, Webb M, et al. Nursing interventions to reduce the risk of catheterassociated urinary tract infection: part 2: staff education, monitoring, and care techniques. J Wound Ostomy Continence Nurs. 2009 36:137-54. PMID: 19287262.
Deviation Of Catheter Tip
Subsequently, we focused on the movement of each catheter tip during one set of predetermined operations with the device at velocities of 20, 40, 60, 80, and 100 mm/s in water. The distances that the catheter tips moved from their resting point are shown . The tips of all the catheters barely moved under the pulling term even on increasing the velocity. Under the pushing term, the tip of FC moved significantly in proportion to its velocity followed by the tip of NC, while the tip of OEFC barely moved even on increasing the velocity .
Figure 4
Deviation of each catheter tip. The upper panels of show the photographs of each catheter tip when the syringe was pulled at 20 or 100 mm/s. The lower panel of shows the distance that catheter tips have moved from their resting points. The upper panels of show the photographs of each catheter tip when the syringe was pushed at 20 or 100 mm/s. The lower panel of shows the distance that catheter tips have moved from their resting points. All operations were performed with our device at velocities of 20, 40, 60, 80, or 100 mm/s in water. Black arrows indicate the location of each hole and red dots indicate resting points.
Also Check: How Long Can A Puppy Hold His Bladder
How Do You Care For A Urinary Catheter
One-time use catheters and reusable catheters are available. For reusable catheters, be sure to clean both the catheter and the area where it enters the body with soap and water to reduce the risk of a UTI. One-time use catheters come in sterile packaging, so only your body needs cleaning before inserting the catheter.
You should also drink plenty of water to keep your urine clear or only slightly yellow. This will help prevent infection.
Empty the drainage bag used to collect the urine at least every 8 hours and whenever the bag is full. Use a plastic squirt bottle containing a mixture of vinegar and water or bleach and water to clean the drainage bag. Read more on clean intermittent self-catheterization.
While UTIs are the most common side effects associated with urinary catheters, there are other potential side effects that you may discuss with your doctor. These include:
- bladder spasms and pain, which may feel like stomach cramps
- blood or other debris getting trapped inside the catheter tube, which may stem from blockage in the catheters drainage system
- catheter leakage, which may happen from a blockage in the system, or from pushing during toileting if youre constipated
- urethra or bladder injuries
While not all side effects from urinary catheter use are completely avoidable, you may help reduce your risk with certain dietary and hygiene steps, as well as preventing blockages in the catheters drainage system.
Discuss the following risk factors with your doctor:
What Is A Catheter
A catheter is a tube that is inserted into your bladder, allowing urine to drain freely. The catheter tube is attached to a drainage bag , where the urine can be collected.
Catheters are usually inserted through the urethra .
Some people with urinary problems need catheters permanently, but more often people need them for a short time.
Recommended Reading: Swanson Go Less Bladder Control Formula
Force Required For Irrigation
For a more precise evaluation of the efficiency of MBW using each catheter, we fabricated an automatic irrigation device for a 60 ml catheter tip syringe. Detailed image of the device and schematic image of our methodology using it were shown in Fig. AC. Video of the actual operation can be seen in Supplementary information. At a velocity of 20 mm per second , for example, the syringe moved about 13.5 ml syringe scale per second , and the pulling time was completely consistent with the pushing time: between the ranges of 2159 and 2190 ms .
Figure 2
An automatic irrigation device. An automatic irrigation device for a 60 ml catheter tip syringe was used to repeat a predetermined movement at a constant velocity. Detailed photographs of the device. The tip of each catheter, attached to a syringe, was inserted into different types of containers appropriate for the experiment. The syringe was set to start operation from the 0 scale, pulled to 30 scale, and pushed to 0 scale, repeating the operation three times. This series of operations was considered in a single set.
Figure 3
Force required for irrigation. Images of the output waveform of the required force when the operation was performed at 20 mm/s in water. The force required in the pulling direction was indicated as plus and the force required in the pushing direction was indicated as minus. Multiple comparisons of average values of the force required for pulling and pushing at a velocity of 20, 40, 60, 80, and 100 mm/s.
Slide 1: Securing Drainage Bag
- Advance tubing another 3-5 cm once you see urine in the tubing
- Inflate balloon with 10 cc sterile water
Recommended Reading: Treating Overactive Bladder At Night
Warnings And Common Errors
-
Be sure to maintain strict sterile technique during the procedure to avoid urinary tract infection Introduction to Urinary Tract Infections Urinary tract infections can be divided into upper tract infections, which involve the kidneys , and lower tract infections, which involve the bladder , urethra… read more .
Slide : Alternative Catheter Types
Straight Catheters
- Inserted directly into the urethra and bladder.
- Removed after insertion and drainage of bladder.
- Used intermittently.
- Placed surgically directly through skin into the bladder.
- Connected by tubing to a bag used to collect and measure urine.
External “Condom” Catheters for Men
- Does not enter the bladder.
- Connected by tubing used to collect and measure urine output.
- Cannot be used to treat acute urinary retention.
Also Check: How Long Can You Have A Bladder Infection
What Kind Of Problems Should I Watch Out For
Here are some of the problems to watch for:
- Urine stops draining out of the catheter
- You feel unwell with pain, fever and abdominal discomfort
- Urine is leaking around the catheter this can be normal around a new catheter site
- The area around the catheter becomes red and sore
- Bleeding. It is not unusual to see blood in the urine following a change of catheter but this usually settles in 24 hours.
Occasionally the skin around the catheter heals over and small skin tags form. If they become problematic i.e. bleed easily and interfere with catheter changes, they can be treated by your healthcare professional.
Some healthcare professionals recommend turning the catheter when cleaning the area to help prevent the catheter sticking to the bladder wall. If you notice anything unusual or feel unwell, contact your doctor or nurse.
Slide : Learning Objectives
Upon completion of this session, licensed staff who insert or assist in the insertion of urinary catheters will be able to
- Explain the similarities and differences between the four different types of urinary catheters
- Prepare for and insert an indwelling urinary catheter using aseptic technique and
- Summarize effective strategies in preventing CAUTIs.
You May Like: How To Get Rid Of Blood Clots In Bladder
Slide 1: Female Catheter Insertion Procedure
- Using gloved nondominant hand, identify urethra by spreading the labia
- Spread inner labia slightly with gentle traction and pull upwards toward resident’s head.
- Clean periurethral area and urethral opening using antiseptic soaked swabs using tongs, in expanding circular motion. Discard used swabs away from sterile field.
Slide 1: Insertion Avoiding Common Mistakes4
- Wash hands BEFORE and AFTER procedure
- Put on your sterile gloves after opening catheter kit
- If sterile, gloved hand gets contaminated or glove rips, then remove glove, wash hands, and don NEW sterile gloves
4. Manojlovich M, Saint S, Meddings J, et al. Indwelling urinary catheter insertion practices in the emergency department: an observational study. Infect Control Hosp Epidemiol. 2016 37:117-9. PMID: 26434781.
Read Also: Can Too Much Sugar Cause A Bladder Infection
Efficiency Of Mbw By Urologists
Three types of 22 Fr urinary catheters, a rounded tip Foley catheter with the standard two eyes, an open-ended Nelaton catheter with a side hole, and an open-ended Foley catheter with a side hole closer to the tip than NC, were evaluated. Photographs viewed from the tip or each side of the catheter were shown . The red dotted line shows the outline of each hole. The side holes were located at 9 and 17 mm respectively from the tip in FC, 8 mm in NC, and 2 mm in OEFC. The cross-section of FC was the same as that of OEFC, and each major axis of the lumen was 4 mm, while NC had 5 mm lumen diameter. Total relative area of the holes in each catheter is shown . Area of one of the holes in FC was set to 1. On comparing the area, NC had the largest holes followed by FC and OEFC.
Figure 1
The efficiency of MBW. Photographs viewed from the tip or each side of the catheters used in this study. Red dotted line shows the outline of each hole. Total relative area of the holes in each catheter. The area of one of the holes in FC was set to 1. The schematic image of how to evaluate MBW. Wasted fluids volume and decreased clots volume of soft tofu. Wasted fluids volume and decreased clots volume of hard tofu. The decreased volume of PBC after the procedure mimicking MBW was done by 11 urologists.
When Is Surgery Needed For A Prolapsed Bladder
Severe prolapsed bladders that cannot be managed with a pessary and/or behavioral therapy usually require surgery to correct them. There are several different types of surgery depending on the severity of the prolapse and whether or not other organs are affected.
- The bladder is repaired with an incision in the vaginal wall.
- The prolapsed area is closed and the wall is strengthened. This may be done primarily using one’s own tissues or through the use of grafts, which may be biologic or synthetic .
- If one has stress urinary incontinence, this is also corrected.
- Depending on the procedure, surgery can be performed while the woman is under general, regional, or local anesthesia. Most women are discharged home on the same day of surgery.
- Various materials have been used to strengthen pelvic weakness associated with prolapsed bladder. A surgeon should explain in detail the risks, benefits, and potential complications of these materials, and he or she should explain the procedure itself before proceeding with the surgery. Complications related to surgery may include bleeding, infection, pain, urinary incontinence, recurrent prolapse, trouble urinating, and injury to the bladder.
- The cost of surgical treatment will vary with the procedure performed, the length of hospitalization, and the presence/absence of other medical conditions.
- After surgery, most women can expect to return to a normal level of activity after 6 weeks.
Don’t Miss: What Happens When Your Bladder Stops Working
Urinary Decompression After Urologic Reconstruction
The role of urinary drainage via trans-anastomotic ureteral stenting or percutaneous drainage remains heavily debated with the emergence of stent-less ureteral reconstruction, specifically in pyeloplasty.37 While this debate continues for upper tract urinary decompression, urethral catheterization is seemingly ubiquitous to drain the lower urinary tract. Conventionally, the bladder is decompressed for at least 24 hours, or overnight, in instances where extravesical ureteral reimplantation is utilized unless the patient has a history of voiding or bowel dysfunction, or both. More variability is seen in intravesical ureteral reimplant as the bladder wall and mucosa are violated. Urethral catheter dwell time in these instances is based on surgeon preference.
Postoperative Urinary Retention What Is It And What Mitigation Strategies Exist
The overall risk of postoperative urinary retention in the general surgical population is 3.8%, though the cited incidence can vary widely from 5 to 70% based on the type of surgery.7 In pediatric patients undergoing lower extremity orthopedic limb surgery, up to onethird of patients may develop POUR.8
The alterations in physiology in the postoperative period can result from various types of anesthesia employed. The effects may be due to anesthesia itself, the procedure performed and technique utilized, polypharmacy intraoperatively, and postoperative pain. Although there has been a recent push away from postoperative opiate pain management, opioids are commonly still used intraoperatively and are known to decrease the sensation of bladder filling by parasympathetic inhibition.9 Additionally, they increase sphincter tone. The effect, and subsequent urinary retention, is greater with neuraxial opioids compared to intravenous administration. General anesthesia also contributes to urinary retention by increasing smooth muscle relaxation, and, conversely, decreasing bladder contractility. Finally, local neuraxial local anesthetics act at the immediate afferent and efferent junctions in the pathways pivotal to micturition. As such, longer acting agents carry a greater risk for postoperative bladder dysfunction.
Also Check: Bcg Treatment Schedule For Bladder Cancer
Catheter Size In Children One Size Does Not Fit All
Catheterization in the pediatric patient, unlike the adult patient, is often performed in conjunction with diagnostic as well as therapeutic procedures. Examples in which catheterization is diagnostic include contrast-enhanced imaging modalities such as that seen in cystourethrography. Though the procedure is commonly performed and relatively safe, there are relative contraindications to immediate catheterization including pelvic fractures, known trauma to the urethra, or blood at the meatus.17 Complications are rare considering how frequently catheterization is performed, however, they do arise. Examples include false passage creation, urethral perforation, hematuria secondary to traumatic placement, infection and subsequent delayed complication of urethral stricture formation.
Key to avoiding, or at least minimizing, complications is appropriate catheter size selection. The method for doing so varies widely and traditional selection processes rely on the childs age, body weight, or both. Exact formulas have even been derived to provide an ideal and custom approach to proper catheter sizing in children. One relies on a patients age to estimate body weight up to 10-years:22 Weight may not always be the most accurate, however, as there can be great variance of expected weight for a given age. To address this, Kopac devised a formula based entirely on body weight and correlated this with catheter size: