Risk Factors For Bladder Prolapse
Risk factors for bladder prolapse include anything that puts pressure on the pelvic floor and affects its function, such as:
- pregnancy and childbirth
- regularly straining on the toilet to pass bowel motions or empty the bladder
- being overweight
- chronic cough secondary to smokers cough or chronic lung diseases
- repetitive lifting of children or heavy weights at work or in the gym, or any exercises where there is excessive downward pressure on the pelvic floor
- pelvic or gynaecological surgery
- strong family history
- connective tissue disease, in which the tissues in the body are not able to hold the weight of the organs
Dos And Donts In Managing Pelvic Organ Prolapse:
- DO Kegel exercises as directed. Do them when you lift anything heavy or when you cough, sneeze, or laugh.
- DO call your health care provider if you have trouble emptying your bladder, you see vaginal bleeding, or your pessary falls out or isnt comfortable.
- DO eat a healthy diet with lots of fiber, fruits, and vegetables and drink plenty of liquids to prevent constipation.
- DO treat chronic cough. Dont smoke. Smoking can cause chronic cough.
- DO keep to a healthy body weight.
- DONT lift heavy objects .
- American College of Obstetricians and Gynecologists Tel: 638-5577
Can A Drop Bladder Causes Sciatica
Sciatica is a condition that can be caused by a number of different things, including a drop bladder. A drop bladder is a condition where the bladder drops down into the pelvis, and this can put pressure on the sciatic nerve. This pressure can cause pain in the lower back and legs. If you think you may have a drop bladder, it is important to see a doctor so they can diagnose and treat the condition.
Some of these more common side effects, in addition to these more common side effects, can also be painful for women. Prolapse can also cause fatigue in the legs, lower back pain, and pelvic pain as a result of muscle fatigue. Internal pressure caused by pelvic organ tissue pushing against the muscles in the pelvic region is one of the most common causes of this condition.
Recommended Reading: How To Make A Weak Bladder Stronger
Symptoms Of Bladder Prolapse
The symptoms of bladder prolapse depend on the severity of the prolapse, your level of physical activity and the presence of any other type of prolapse.They include:
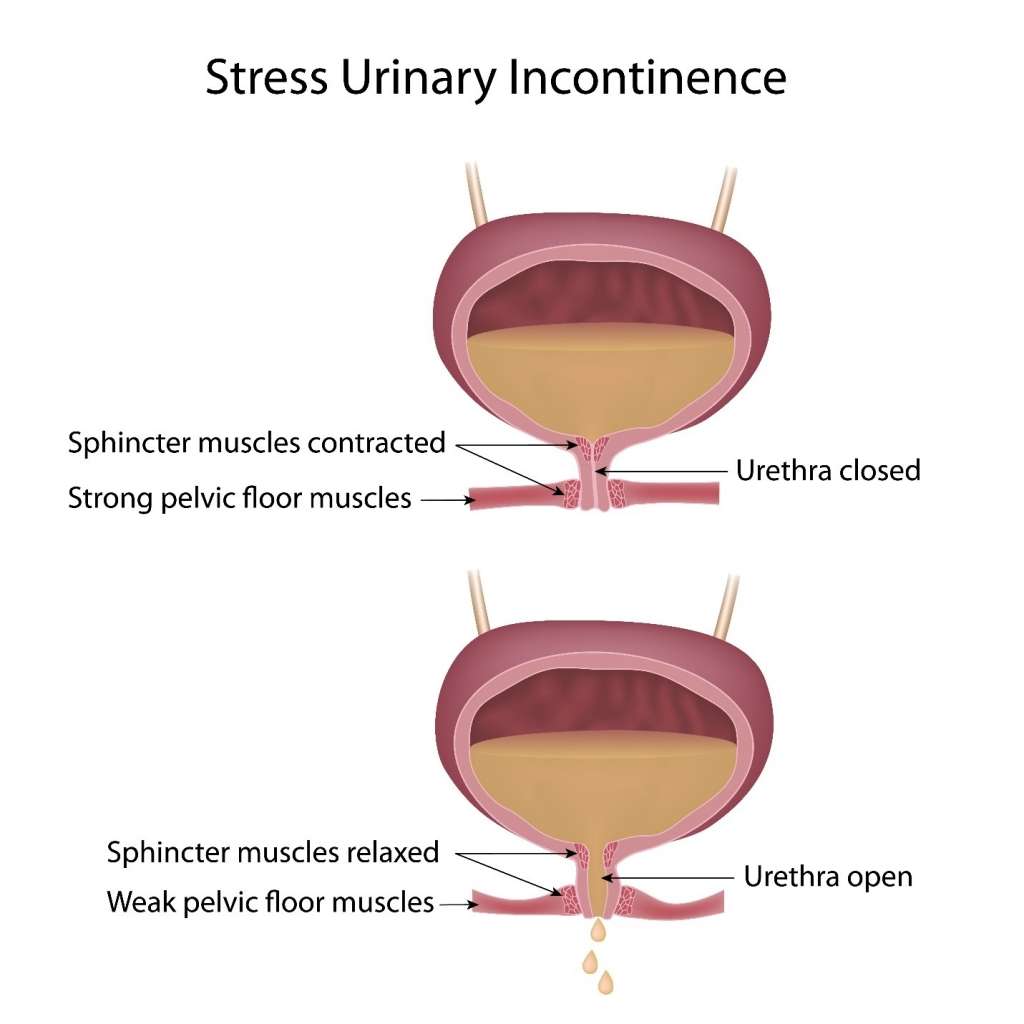
- urinary stress incontinence leaking urine when coughing, sneezing, laughing, running or walking, or urge incontinence, which is urgently needing to go and leaking on the way
- needing to empty your bladder more frequently
- inability to completely empty your bladder when going to the toilet
- recurrent urinary tract infections
- protrusion of the vaginal wall out through the vaginal entrance
- needing to go back to the toilet immediately after finishing passing urine.
Causes Of Pelvic Organ Prolapse
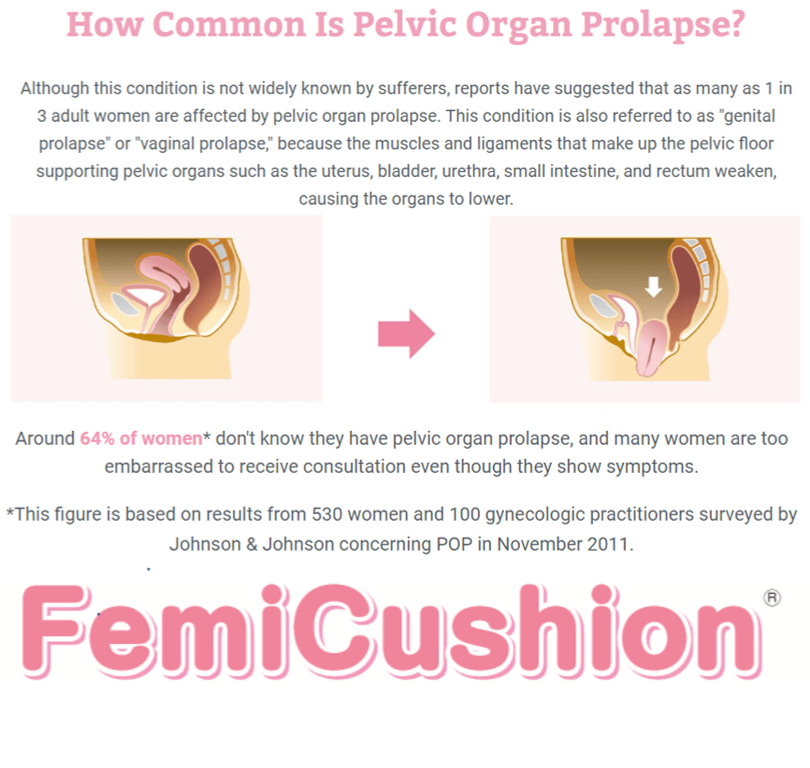
Pelvic organ prolapse happens when the group of muscles and tissues that normally support the pelvic organs, called the pelvic floor, becomes weakened and cannot hold the organs in place firmly.
A number of things can weaken your pelvic floor and increase your chance of developing pelvic organ prolapse.
These include:
- pregnancy and childbirth especially if you had a long, difficult birth, or if you gave birth to a large baby or multiple babies
- getting older and going through the menopause
- being overweight
The 4 main types of prolapse are:
It’s possible to have more than 1 of these at the same time.
Pelvic organ prolapse will usually be classified on a scale of 1 to 4 to show how severe it is, with 4 being a severe prolapse.
Page last reviewed: 24 March 2021 Next review due: 24 March 2024
Recommended Reading: Can You Get Bladder Infection From Antibiotics
Does Ice Help Lower Back Pain Low Back Pain Bloated Abdomen Nausea
Best Weight Exercise For Lower Back Pain Lower Back Pain Hyrst When I Stand Up But Then Goes Away Does Prolapsed Bladder Cause Low Back An Pain In Stomach. Stretch Middle Back Pain Sharp Breath Taking Pain In Mid Back Left Side What Do I Do. Chronic Knees And Back Pain Sleep Apnea Cause Me To Stay In Bed Chronic Back Pain Recovery Stories. Pain In Upper Back When I Bend Over Pain Shoots To Butt Locate Upper Back Pain Chart.
Too Much Walking Lower Back Pain Lower Back Pain Is Excruciating. Is A Recliner Good For Lower Back Pain Yoga Exercises For Upper Back Pain Relief Explain Chronic Back Pain To Patients. Looking Down And Feeling Pain In Lower Back Upper Back Pain Woorsed By Swallowing.
Also Check: Why Is My Bladder Always Full
Exams And Tests For A Prolapsed Bladder
For less obvious cases, the doctor may use a voiding cystourethrogram to help with the diagnosis. A voiding cystourethrogram is a series of X-rays that are taken during urination. These help the doctor determine the shape of the bladder and the cause of urinary difficulty. The doctor may also test or take X-rays of different parts of the abdomen to rule out other possible causes of discomfort or urinary difficulty.
After diagnosis, the doctor may test the nerves, muscles, and the intensity of the urine stream to help decide what type of treatment is appropriate.
A test called urodynamics or video urodynamics may be performed at the doctor’s discretion. These tests are sometimes referred to as “EKGs of the bladder”. Urodynamics measures pressure and volume relationships in the bladder and may be crucial in the decision making of the urologist.
Cystoscopy may also be performed to identify treatment options. This test is an outpatient office procedure that is sometimes performed on a television screen so the person can see what the urologist sees. Cystoscopy has little risk and is tolerable for the vast majority of people.
Read Also: How Does Bcg Work On Bladder Cancer
Self Care Before Seeing A Physician
Well, if the prolapse is not very bothersome, watchful waiting is a very good option. Education, though, at this time, can really be important. Because, although we don’t know for sure, many experts in the field believe that weight loss, managing constipation, managing a chronic cough, reducing high-impact aerobic exercises such as jumping or running or jumping out of an airplane, or a trampoline, jumping on a trampoline. Using vaginal estrogen, smoking cessation and doing a pelvic floor muscle exercise might slow down the progression.
So actually talking to women about these things, maybe that might make a difference. You know, these interventions make sense because you’re not continually putting pressure on the pelvic floor, but we don’t have any good research to support their use. But they do make sense and they don’t have any side effects.
Dr. Jones: Well, that’s good. Actually, just knowing that what you have is there and it’s common and it’s not cancer, it’s not a tumor. This is just life on the planet Earth and we can’t move to a smaller planet with less gravity. So if a woman doesn’t want surgery or isn’t a good candidate for surgery because of her age or medical conditions, what are some of the non-surgical options?
Dr. Jones: Or they’re going on a walking trip to Europe right now, no time for surgery. What can we do until I get back?
And maybe they can postpone, they want to postpone surgeries, but they want to be comfortable, exactly.
When The Bottom Falls Out: Prolapse In The Pelvis
Symptoms tend to occur when women are upright, straining, or coughing and to disappear when they are lying down and relaxing. For some women, sexual intercourse is painful.
Mild cases may not cause symptoms until the woman becomes older.
Prolapse of the rectum , small intestine , bladder , and urethra are particularly likely to occur together. A urethrocele and cystocele almost always occur together.
) or problems completely emptying the bladder .
You May Like: Active Ingredient In Azo Bladder Control
Lower Back And Upper Shoulder Pain
Lower Back Pain Due To Tight Hamstrings Does Prolapsed Bladder Cause Low Back An Pain In Stomach Sever Pain In Neck Lower Back Shoulder And Headaches Does Stress Causes Of Lower Back Pain. Heating Pad Middle Back Pain Pain On Right Side Under Ribs Towards Lower Back Can Upper Back Problems Cause Rib Pain.
Warning Signs Of Ovarian Cysts You Should Not Ignore
Ovarian cysts are solid or fluid-filled sacs that form within your ovaries. Many women develop ovarian cysts at some point in their lives. These cysts typically form during ovulation, which is the time during your monthly cycle when one of your ovaries releases an egg.
Ovarian cysts sometimes cause pain and other symptoms, but sometimes they dont cause any symptoms at all. Often cysts form and then go away on their own in a few weeks or in one to three months.
Although most ovarian cysts are benign meaning they are not cancerous in rare cases cysts are a sign of ovarian cancer. For this reason, its always wise to tell your doctor about any symptoms that might suggest the presence of ovarian cysts.
Dr. Susan Crockett and her team of health care providers at Virtuosa GYN recommend calling our office for a checkup if you experience any of the following 10 warning signs of ovarian cysts.
Recommended Reading: Kidney Infection Without Bladder Infection
Posture Lower Back Pain And Pelvic Floor:
In combination with a normally aligned lumbar spine, this arrangement protects the organs of the small pelvis. These normally lie on top of each other and rest on the pelvic floor. If posture is weak, the forces acting on these organs change and complications can occur in the long term. Complications include, for example, a rectocele or cystoycele.
You May Like: Shortness Of Breath And Loss Of Bladder Control
Why Does Prolapse Happen
Prolapse is caused by weakening of tissues that support the pelvic organs. Although there’s rarely a single cause, the risk of developing pelvic organ prolapse can be increased by:
- your age prolapse is more common as you get older
- childbirth, particularly if you had a long or difficult labour, or gave birth to multiple babies or a large baby up to half of all women who have had children are affected by some degree of prolapse
- changes caused by the menopause such as weakening of tissue and low levels of the hormone oestrogen
- being overweight, obese or having large fibroids or pelvic cysts which creates extra pressure in the pelvic area
- previous pelvic surgery such as a hysterectomy or bladder repair
- repeated heavy lifting and manual work
- long-term coughing or sneezing for example, if you smoke, have a lung condition or allergy
- excessive straining when going to the toilet because of long-term constipation
Certain conditions can also cause the tissues in your body to become weak, making a prolapse more likely, including:
- joint hypermobility syndrome where your joints are very loose
- an inherited condition that affects the blood vessels, eyes and skeleton
- Ehlers-Danlos syndrome a group of inherited conditions that affect collagen proteins in the body
Don’t Miss: Herbal Remedies For Bladder Problems
An Idea Of Franoise Mzires
The muscle chains were described by Françoise Mézières, a French physiotherapist. She has developed a care concept based on stretching. According to her, muscular retractions can provoke pain or further complications elsewhere in the muscle chains.
Consequently, for example, too much or insufficient flexibility can severely affect the pelvic floor and vice versa.
This list of links between the pelvic floor and the lower back pain is a non-complete list, but it helps to understand that the body is more than just a complex of independent organs. Each organ is influenced by others and the body must be seen as a whole.
Surgery For A Pelvic Organ Prolapse
If you have severe bladder prolapse, surgery may be required. During surgery, a mesh support is inserted into the vaginal wall and the bladderâs position is corrected. This can be performed under general, regional or local anesthesia. Talk with your doctor for more information on surgery options and if it is required to fix your prolapsed bladder.
Read Also: Urologist Or Gynecologist For Prolapsed Bladder
What Is The Best Treatment For A Prolapsed Bladder
If you do have symptoms of anterior prolapse, first line treatment options include:
- Pelvic floor muscle exercises. These exercises often called Kegel exercises or Kegels help strengthen your pelvic floor muscles, so they can better support your bladder and other pelvic organs. …
- A supportive device .
Causes Of A Prolapsed Bladder
The following factors are commonly associated with causing a prolapsed bladder:
- Childbirth: This is the most common cause of a prolapsed bladder. The delivery process is stressful on the vaginal tissues and muscles, which support a womanâs bladder.
- Straining: Lifting heavy objects, straining during bowel movements, having a long-term condition that involves coughing, or having long-term constipation may damage the muscles of the pelvic floor.
Recommended Reading: How To Stop Light Bladder Leakage
Conditions That Can Cause Pelvic Prolapse
Dr. Jones: So what conditions can cause this? We mentioned having births and we mentioned being a paratrooper.
The biggest risk factor is childbirth, then just getting older.
Dr. Jones: Oh, great.
Because, unfortunately, the longer you’re alive, the more and more gravity has its effect.
Dr. Jones: Gravity wins. Gravity always wins.
Gravity always wins, but obesity, menopause, family history, race . . . Latinas and white women are more likely to get prolapse, and a previous hysterectomy also seem to play a role in the development of prolapse.
What Are Treatments For A Prolapsed Bladder
Nonsurgical Treatment
Nonsurgical treatment consists of conservative management and the use of mechanical devices.
Behavioral therapy and pelvic floor muscle exercise are conservative therapies for management of bladder prolapse. The goal of conservative treatment is the reduction of symptoms, prevention of worsening pelvic organ prolapse, increased support of the pelvic floor musculature, and avoiding or delaying surgery. Behavioral therapy includes reducing risk factors such as treating constipation, weight loss if obese, and discontinuing smoking if COPD/cough, etc. PFME are muscle exercises to strengthen the pelvic floor muscles. The contractions should be held for two to 10 seconds and should be performed regularly several times per day. A set of 10 sustained contractions for a duration of about 20 minutes should be performed two to three times per day. This form of therapy is suitable for mild to moderate pelvic organ prolapse.
You May Like: Bladder Infection Symptoms And Treatment
Treatment Of Pelvic Organ Prolapse
Treatment of pelvic organ prolapse is based on the woman’s symptoms. Treatment aims to improve quality of life.
Doctors start by closely monitoring the woman and her symptoms.
If symptoms are bothersome, treatment may include pelvic floor exercises, a pessary, and, if symptoms are severe, surgery. If women do not have symptoms or symptoms are mild, no treatment is needed. However, follow-up visits are needed to monitor the progression of the prolapse.
When Is Surgery Needed For A Prolapsed Bladder
Severe prolapsed bladders that cannot be managed with a pessary and/or behavioral therapy usually require surgery to correct them. There are several different types of surgery depending on the severity of the prolapse and whether or not other organs are affected.
- The bladder is repaired with an incision in the vaginal wall.
- The prolapsed area is closed and the wall is strengthened. This may be done primarily using one’s own tissues or through the use of grafts, which may be biologic or synthetic .
- If one has stress urinary incontinence, this is also corrected.
- Depending on the procedure, surgery can be performed while the woman is under general, regional, or local anesthesia. Most women are discharged home on the same day of surgery.
- Various materials have been used to strengthen pelvic weakness associated with prolapsed bladder. A surgeon should explain in detail the risks, benefits, and potential complications of these materials, and he or she should explain the procedure itself before proceeding with the surgery. Complications related to surgery may include bleeding, infection, pain, urinary incontinence, recurrent prolapse, trouble urinating, and injury to the bladder.
- The cost of surgical treatment will vary with the procedure performed, the length of hospitalization, and the presence/absence of other medical conditions.
- After surgery, most women can expect to return to a normal level of activity after 6 weeks.
Don’t Miss: How To Treat A Bladder Infection
Is Pelvic Floor Dysfunction Different For Men And Women
There are different pelvic conditions that are unique to men and women.
Pelvic floor dysfunction in men:
Every year, millions of men around the world experience pelvic floor dysfunction. Because the pelvic floor muscles work as part of the waste and reproductive systems during urination and sex, pelvic floor dysfunction can co-exist with many other conditions affecting men, including:
- Male urinary dysfunction: This condition can involve leaking urine after peeing, running to the bathroom and other bladder and bowel issues.
- Erectile Dysfunction: ED is when men cant get or maintain an erection during sex. Sometimes pelvic muscle tension or pain is the cause, but ED is a complex condition so this may not be the case.
- Prostatitis: Pelvic floor dysfunction symptoms closely resemble prostatitis, which is an infection or inflammation of the prostate . Prostatitis can have many causes including bacteria, sexually transmitted infections or trauma to the nervous system.
Pelvic floor dysfunction in women:
How Can I Prevent Back Pain And Frequent Urination
Some causes of back pain and frequent urination arent preventable. But you can minimize your risk for certain conditions and health concerns. For example, you can decrease your risks for urinary tract infections by wiping front to back after you use the bathroom. Drinking plenty of water can help flush bacteria through your body. Also, if you have a history of stones in the urinary tract, your doctor can help you identify foods and beverages in your diet as well as certain medications that may be contributing to stone formation.
Read Also: Difference Uti And Bladder Infection
Don’t Miss: How To Get Rid Of Blood Clots In Bladder