Can Response To Therapy Be Predicted
The potential for concentrations of urinary neutrophils to predict antitumor activity has already been discussed however, other parts of the immune response have also been put forward to perform the same purpose. Measurement of tumor-infiltrating dendritic cells and tumor-associated macrophages has been proposed as a means by which to predict the response to BCG therapy. Ayari et al assessed levels of CD83+ dendritic cells and CD68+ macrophages in patients with high-risk NMIBC treated with transurethral resection of bladder tumor and maintenance BCG. Their results suggested that patients with low levels of CD83+ tumor-infiltrating dendritic cells responded better to maintenance BCG than patients with higher levels at the time of resection. In the same cohort, a similar effect was seen in those patients who recruited more CD68+ tumor-associated macrophages, ie, there was an increased risk of recurrence. Further studies are required to confirm these preliminary findings, but if validated, the pretreatment levels of these immune cells may have relevance in determining the treatment regime for individual patients.
What To Expect Before Bcg Treatment
Before you are scheduled for BCG therapy, you will have to go through a screening test. This screening will determine whether you are eligible for BCG treatment or not. Factors considered during this screening test include the patients age, cancer type and stage, and overall health.
The doctor along with a radiation therapist will determine the best course of treatment for your condition and also ask you to avoid drinking too much fluid like water, juice, or caffeine.
If you are eligible, you will be given a date to schedule your treatment and will receive specific instructions on how to prepare. Once BCG is injected into the bladder, you will have to wait for 1-2 hours before urinating. This will allow the medicine to reach all the areas of the bladder.
Also Read:- What are the Symptoms of Urinary Bladder Cancer?
The success rate of bladder cancer treatment will vary depending on the age of the patient and the stage of the disease. Bladder cancer is a common and treatable disease, but bladder cancer treatment can be complex and challenging.
There are different treatment options available, each with different pros and cons. The best treatment option for you will depend on your situation and health.
We hope the information was helpful for you to understand what BCG treatment is, its symptoms, and what you can expect after the treatment. This method of treatment is considered a form of immunotherapy, which is an emerging form of cancer treatment.
Moving From The Lab To The Clinic
Dr. Glickmans laboratory is now collaborating with urologic surgeon Bernard H. Bochner to explore the clinical implications of this discovery particularly, whether analyzing a patients bladder cancer cells can reliably predict his or her responsiveness to BCG therapy.
With the support of a grant from The Society of MSKCC, Dr. Redelman-Sidi is trying to develop a lab test that would analyze urine samples, which usually contain cancer cells shed from the bladder. These cells could be tested both for their tendency to take up BCG and also for the presence of BCG-activating, cancer-causing mutations.
This would allow us to screen early-stage patients routinely before starting BCG therapy to make sure its the best course of treatment, Dr. Glickman says.
Don’t Miss: How Do You Diagnose Overactive Bladder
Intravesical Therapy For Bladder Cancer
With intravesical therapy, the doctor puts a liquid drug right into your bladder rather than giving it by mouth or injecting it into your blood. The drug is put in through a soft catheter that’s put into your bladder through your urethra. The drug stays in your bladder for up to 2 hours. This way, the drug can affect the cells lining the inside of your bladder without having major effects on other parts of your body.
Is Immunotherapy Right For Me

If you have metastatic bladder cancer, when the disease has spread to other parts of your body, youâve probably tried other treatments. If they havenât worked, you still have options, including immunotherapy.
These medicines can spur your body’s immune system to identify and destroy cancer cells.
Talk carefully with your doctor to decide whether immunotherapy is a good choice for your treatment.
Making your decision
Your doctor will think about a few things before they recommend immunotherapy for you:
- The type of cancer you have
- How far the disease has spread in your body, called the stage of your cancer
- The chances your disease will come back
- The size and number of tumors
- Other treatments youâve already tried
When making your decision, ask your doctor a few questions to get a better idea of the role immunotherapy might play in your overall treatment plan, such as:
- Why are you recommending immunotherapy for me?
- Will immunotherapy be the only treatment I get right now? How does it work with other types of bladder cancer treatment?
- How will it help me?
- What kind of side effects should I expect?
- How long will the treatment last? What is the process like?
Read Also: Sudden Loss Of Bowel And Bladder Control
What Is The Immune System And How Does It Work With Cancer
The immune system is a natural part of our body. Its role is to get rid of foreign or damaged material and cells before they cause trouble.
Most of the time, our immune system can find foreign invaders like bacteria and viruses, and destroy them. The immune system uses signals to attack them while leaving healthy cells alone.
Cancer is different from an illness caused by a bacteria or virus. It involves the uncontrolled growth of normal body cells. In other words, cancer cells may not be found by the immune system. Though they look different under the microscope, cancer cells can hide and grow. One way cancer cells hide is to express proteins on their surface to turn-on a “checkpoint” to stop an immune system attack.
The National Cancer Institute studied common tumors in its Cancer Genome Atlas project. The research showed that bladder cancer, skin cancer and lung cancer have the most cellular changes . These types of cancer may be more likely to respond to treatments that help the immune system find cancer cells, called “immunotherapies”.
What is Immunotherapy?
Immunotherapy is any treatment that makes the immune system stronger. For cancer, it helps the body find and attack cancer cells. The field of immuno-oncology studies how the immune system interacts with cancer. It uses that information to make new treatments.
What Happens Under Normal Conditions?
What Happens When Cancer Cells Grow and Hide?
Three things help cancers hide from the immune system:
Immunological Hallmarks For Clinical Response To Bcg In Bladder Cancer
- 1Translational Immunology Institute , SingHealth-DukeNUS Academic Medical Centre, Singapore, Singapore
- 2Duke-NUS Medical School, Singapore, Singapore
- 3Division of Pathology, Singapore General Hospital, Singapore, Singapore
- 4Institute of Molecular Cell Biology , Agency of Science, Technology and Research , Singapore, Singapore
- 5Department of Urology, Singapore General Hospital, Singapore, Singapore
Read Also: Stage 4 Bladder Cancer Symptoms
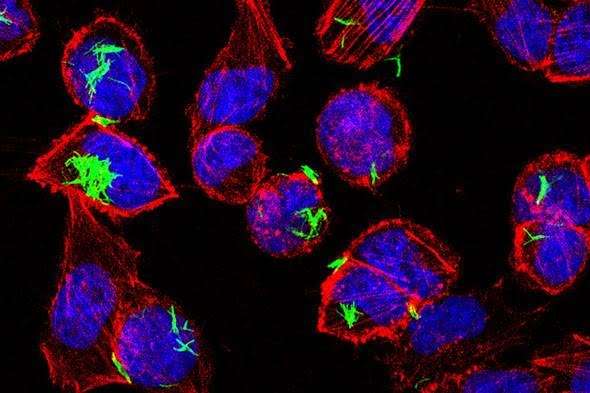
Infection Of Urothelial Cells
Ratliff demonstrated the role of fibronectin in the attachment of BCG to tumor cells in the late 1980s. BCG is then internalized into the tumor cells, a step that appears to be fundamental to the subsequent immune response. This was demonstrated in experiments where an antifibronectin antibody inhibited the antitumor effect of BCG. In a mouse model, BCG has been found in urothelial cells within 24 hours of instillation. This finding has been supported by in vitro studies in human bladder cancer cell lines.,
Treatment Of Superficial Bladder Cancer
The treatment of bladder cancer in general depends on numerous factors, including stage and grade of the disease, patient age, and their co-morbidity. The standard treatment of superficial bladder cancer is a transurethral resection, this initial resection usually removes the tumour but it is known that they have a great propensity to recur. It is important to realise that some tumours progress, and in those which do it is vital that they are recognised so that further treatment can be instigated. A significant breakthrough in the last decade has been the clear definition of prognostic factors, which determine later recurrence. Using these factors it is possible to identify different patient subgroups and tailor their treatment and subsequent follow up accordingly. The most important factors are easily assessed at transurethral resection and are listed in box 1.
Don’t Miss: Best Pills For Bladder Infection
Optimization Of The Use Of The Scarce Vials Of Bcg
As soon as BCG shortages began, different strategies were adopted at different levels, from improvements in BCG production to modifications of the recommended treatment.
Improving BCG Production
The production of BCG is not an easy matter. Due to the slow growth of the mycobacteria, any inaccuracy during the manufacturing process can lead to a large loss of time and money, as the BCG shortages have proven. For this reason, some researchers proposed optimizing BCG bulk production by modifying the growth in pellicles to the use of bioreactors or evaluating the possibility of extending the shelf life of the already manufactured BCG vials.
Regulatory Issues/Favorable Policies
Variations in Clinical Guidelines Recommendations
For intermediate-risk NMIBC patients
-
Intravesical chemotherapy must be used as a first-option treatment instead of BCG. Induction once a week for six to eight weeks plus a monthly maintenance schedule for one year.
-
For second-line treatment, a one-third dose of BCG instead of full-dose BCG can be used. In that case, different patients can be treated the same day clustered in groups of three to avoid BCG wastage.
-
Maintenance BCG can be omitted.
For high-risk NMIBC
Different Strains Of Bcg
There are several different strains of BCG available. The more commonly used strains include the Tice strain produced by Organon Teknika, the RIVM strain produced by Bilthoven, and the Connaught strain produced by Connaught Laboratories. Morales used a strain of BCG which came from the Institut Armand Frappier in Montreal, in fact BCG-Connaught is derived from this strain.
As there are several commercially available strains of BCG, uncertainty exists in the literature about whether the various strains of BCG have identical immunotherapeutic efficacy and identical clinical effectiveness. Given this fact direct comparison between clinical studies is difficult when different strains of BCG have been used.
Don’t Miss: How To Flush Bladder Infection
Current Alternatives To Bcg
Research on improving NMIBC therapy has mainly focused on rescue patients who do not respond to BCG therapy, since BCG is truly efficacious in the majority of patients for avoiding recurrence and progression episodes. The alternative treatment options include virus and other bacteria different from BCG as vehicles for specific tumor growth inhibition agents or immunostimulatory components, chemotherapeutic agents, new delivery options for current therapies, and systemic immunotherapies that have to be demonstrated to be efficacious in other types of cancers .
Current alternative research for nonmuscle invasive bladder cancer treatment.
Virus-Based Treatments
Bacteria-Based Treatments
Chemotherapeutic Treatments and Improved Delivery
Different strategies can improve the use of chemotherapy for treating NMIBC. The appearance of new agents, the combination of different chemotherapeutic agents, the use of hyperthermia for improving intravesical instillation, or other strategies have been considered for improving the treatment of intermediate- and high-risk NMIBC patients.
The efficacy of intravesical therapies can also be improved through delivery adaptations such as hyperthermia, electromotive drug administration or new devices.
Checkpoint Inhibitors in Nonmuscle-Invasive BC
Who Can Have This Treatment
BCG is appropriate for noninvasive and minimally invasive bladder cancers. It usually follows a procedure called transurethral resection of bladder tumor . Its intended to help prevent recurrence.
This treatment only affects cells inside the bladder. Its not useful for later stage bladder cancer that has spread into or beyond the bladder lining, or to other tissues and organs.
Also Check: Natural Ways To Control Overactive Bladder
Study Approval And Specimens
Five patients with NMIBC who underwent transurethral resection to remove all endoscopically visible tumors followed by BCG instillations in Singapore General Hospital were recruited upon informed consent according to guidelines from institutional review board . The patientsâ baseline clinicopathological parameters were analyzed . After two-four weeks, the patients received weekly intravesical BCG instillations for six times as standard protocol . Upon completion of the 6 doses instillations, surgical specimens were obtained to confirm that no neoplastic pathology of the mucosa by the pathologists. Tissue specimens were obtained from: pre-BCG resected tumor , pre-BCG adjacent non-tumor tissue and post-BCG NT urothelial tissue. Blood specimens were obtained before and two time points after BCG instillations at 1 month and 3 months . Two patients withdrew from the study and stopped BCG treatment before the last time point due to BCG toxicities/intolerance.
A small piece of pre- and post-BCG tissues were subjected to RNA sequencing analysis. Tissue-infiltrating leukocytes were isolated from pre- and post-BCG tissues with enzymatic digestion: 100μg/ml Collagenase IV and 100μg/ml DNase1 and peripheral blood mononuclear cells from blood using Ficoll-Paque layering, both as previously described . TILs were analyzed using flow cytometry and PBMCs were stored with 10% DMSO in liquid nitrogen until later analysis with CyTOF.
Availability Of Data And Materials
The datasets supporting the conclusions of this article are available in the National Health Insurance Research Database, Taiwan .
Only citizens of the Republic of China who fulfill the requirements of conducting research projects are eligible to apply for the National Health Insurance Research Database . The use of NHIRD is limited to research purposes only. Applicants must follow the Computer-Processed Personal Data Protection Law and related regulations of National Health Insurance Administration and NHRI , and an agreement must be signed by the applicant and his/her supervisor upon application submission. All applications are reviewed for approval of data release.
Recommended Reading: Test To Detect Bladder Cancer
When You Have It
You usually have BCG into the bladder once a week for 6 weeks. This is called the induction course.
You may then have BCG into the bladder every few weeks or months for the next 1 to 3 years. This will depend on your risk of developing invasive bladder cancer. This is called maintenance BCG therapy.
You usually have treatment at the cancer day clinic.
Evidence For Reduction Of Recurrence Of Bladder Cancer By Bcg
There is now a large body of evidence demonstrating the superior efficacy of BCG in the treatment of bladder cancer when compared with TUR alone or TUR and chemotherapy. The European Association of Urology guidelines on NMIBC in 2013 report a total of five meta-analyses to substantiate this claim. In addition, there have been individual randomized controlled trials comparing BCG with epirubicin and IFN, mitomycin C, and epirubicin alone, all of which showed BCG to be the best agent with respect to preventing recurrence.
You May Like: Can You Swim With A Bladder Infection
Failure Of Bcg Contact With The Target
Gradual waning of the immune response. Intravesical BCG instillations induce a transient peripheral immune activation against BCG antigens. Reactivation is observed in most cases after additional BCG courses. The absence of long-lasting immune activation after a single 6-week course of BCG could be related to the increased clinical efficacy observed with BCG maintenance instillations.12,13,14
Inadequate immune response. There is strong evidence that the success of BCG therapy might be due to a preferential induction of a TH-1 response .15,16 Although somewhat controversial, TH-2 responses detected either in the peripheral circulation or locally in the bladder are associated with poorer outcomes and might explain failure to respond to BCG therapy.17
Natural resistance-associated macrophage protein gene polymorphisms. The NRAMP1 gene has been implicated in susceptibility to infectious diseases and in response to BCG. Data suggest implication of the NRAMP1 gene in bladder cancer recurrence and response to BCG.18
Unresponsive tumour. Many recent investigations have determined whether biological markers might predict disease progression and/or response to treatment.19 An excellent review was provided a couple of years ago by Saint and colleagues.20
Surgery After Bcg Failure
The EAU guidelines recommend cystectomy as the treatment of choice for CIS failing adequate BCG and as an option in other high-risk tumours.3 Similarly, the Canadian guidelines state that in patients with high-risk NMIBC with BCG failure, the option of radical cystectomy should be recommended and discussed with the patient .22 The guidelines also suggest that immediate cystectomy may be initially offered to patients with T1G3/T1HG and to patients with high-grade tumours with concomitant CIS or multiple recurrent high-grade tumours . The advantage of cystectomy in superficial tumours that failed BCG treatment is obvious. Tumour-specific survival is between 80% and 90% at 5 years, and thereby approaches the 5-year tumour-specific survival of patients with superficial bladder cancer.11
However, cystectomy for high-risk superficial disease is not only an invasive procedure linked to significant morbidity, but also has a number of other problems associated with it. When patients with NMIBC have a recurrence with invasive disease, a window of opportunity may be overlooked. For instance, in 62 patients with a high-grade recurrence and treated with cystectomy who had failed adequate BCG treatment, the 5-year disease-specific survival rate of progressive patients was only 38%, significantly lower than in those patients without invasive tumour. The authors identified the presence of a tumour in the prostatic urethra before cystectomy as a factor associated with shorter survival.48
You May Like: Bladder Problems After Spinal Surgery
Is There A Better Bcg Strain
The EAU guidelines on NMIBC report no conclusive evidence for a difference in clinical efficacy between the various BCG strains. However, in light of new evidence, this statement is now controversial. A prospective randomized controlled trial by Rentsch et al set out to establish if there was a difference in treatment outcomes between two commonly used strains of BCG, ie, Connaught and Tice. Patients with high-risk NMIBC were given six installations of either BCG Connaught or BCG Tice, and the clinical data were backed up with further tests in murine models. The authors reported a statistically significant benefit of BCG Connaught over BCG Tice with respect to 5-year recurrence-free survival. There was no difference in BCG-related adverse effects. Analysis of the experimental data suggested a more pronounced Th1 response and greater T-cell recruitment in the bladders of BCG Connaught mice. This study suggests that there may be a benefit of BCG Connaught, although further, larger-scale studies will be required in order to validate this finding. Further, if the genes responsible for producing this apparent difference can be confirmed, this could provide valuable information with regard to identification of new targets for potential future immunotherapies.