Bcg Immunotherapy For Transitional
Donald L. Lamm, MDOncology
Prior to the advent of BCG immunotherapy, bladder carcinoma in situ often progressed to muscle invasion. Intravesical chemotherapy completely eradicates the disease in 50% of patients, but fewer than 20% remain disease free after 5 years. Complete responses have been reported in 70% or more of BCG treated patients, nearly two-thirds of which are durable.
Prior to the advent of BCG immunotherapy, bladder carcinoma in situ often progressed to muscle invasion. Intravesical chemotherapy completely eradicates the disease in 50% of patients, but fewer than 20% remain disease free after 5 years. Complete responses have been reported in 70% or more of BCG treated patients, nearly two-thirds of which are durable. Controversy over the optimal induction and maintenance regimens for BCG immunotherapy remain, but SWOG investigators have demonstrated that complete response rates can be increased from the expected 73% to 87% with just three additional BCG instillations given at 3 months. In complete responders, maintenance BCG using three weekly treatments at 6-month intervals improves long-term complete response rates from 65% to nearly 90%. Caution must be exercised to avoid serious side effects.
What Are The Types Of Bladder Cancer Tumors That May Form
Three types of bladder cancer may form, and each type of tumor can be present in one or more areas of the bladder, and more than one type can be present at the same time:
- Papillary tumors stick out from the bladder lining on a stalk. They tend to grow into the bladder cavity, away from the bladder wall, instead of deeper into the layers of the bladder wall.
- Sessile tumors lie flat against the bladder lining. Sessile tumors are much more likely than papillary tumors to grow deeper into the layers of the bladder wall.
- Carcinoma in situ is a cancerous patch of bladder lining, often referred to as a flat tumor. The patch may look almost normal or may look red and inflamed. CIS is a type of nonmuscle-invasive bladder cancer that is of higher grade and increases the risk of recurrence and progression. At diagnosis, approximately 10% of patients with bladder cancer present with CIS.
Risk Adjusted Surveillance And Follow
Guideline Statement 32
32. After completion of the initial evaluation and treatment of a patient with NMIBC, a clinician should perform the first surveillance cystoscopy within three to four months.
Discussion
The natural history of NMIBC is often characterized by recurrence, even for solitary, small, low-grade papillary tumors. At the time of first evaluation and treatment, none of the existent risk stratification tools or urinary biomarkers is sufficiently sensitive and specific to predict which patient will have an early tumor recurrence. Therefore, the only reliable way to know in a particular patient whether they are at risk for early recurrence is by cystoscopic visualization of the urothelium at a relatively early interval after the first treatment/resection. In addition, visualization at a relatively early interval allows the treating urologist to verify that the initial resection was complete. The Panel, therefore, felt that the first repeat cystoscopic evaluation should occur three to four months after the initial treatment and evaluation, regardless of the patients overall risk.
Guideline Statement 33
33. For a low-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent surveillance cystoscopy six to nine months later, and then annually thereafter surveillance after five years in the absence of recurrence should be based on shared-decision making between the patient and clinician.
Discussion
Don’t Miss: What Causes Bladder Leakage When Coughing
How Can I Prevent Bladder Cancer
You may not be able to prevent bladder cancer, but it may be helpful to know the risk factors that may increase the chance youll develop bladder cancer. Bladder cancer risk factors may include:
- Smoking cigarettes: Cigarette smoking more than doubles the risk of developing bladder cancer. Smoking pipes and cigars or being exposed to second-hand smoke also increases that risk.
- Cancer treatments: Radiation therapy is the second-most common risk factor. People who have certain chemotherapy drugs may also develop an increased risk of bladder cancer.
- Exposure to certain chemicals: People who work with chemicals, such as aromatic amines , are at an increased risk. Extensive exposure to rubber, leather, some textiles, paint and hairdressing supplies, typically related to occupational exposure, also appears to increase the risk.
- Infections: People who have frequent bladder infections, bladder stones or other urinary tract diseases may have an increased risk of developing bladder cancer.
- Past bladder cancer: People with a previous bladder cancer are at increased risk to form new or recurrent bladder tumors.
Bladder Reconstructions And Stomas
If you have had your bladder removed, the way you pass urine will change. There are several options that your treatment team will talk to you about:
- Urostomy is where doctors create a new hole in your abdomen called a stoma. Urine drains from the stoma to the outside of your abdomen into a special bag.
- Neobladder is where a new bladder made from your small bowel forms a pouch inside your body to store urine. You will pass urine by squeezing your abdominal muscles. You will also pass a small tube into the neobladder each day to help drain the urine.
- Continent urinary diversion is a pouch made from your small bowel inside your body to store urine. The urine empties through a hole called a stoma to the outside of your abdomen into a special bag.
A bladder reconstruction is a big change in your life. You can speak with a continence or stomal therapy nurse for help, support and information. You can also call Cancer Council . You may be able to speak with a trained Cancer Council volunteer who has had cancer for tips and support.
If you find it difficult to adjust after your bladder reconstruction, it may help to be referred to a psychologist or counsellor.
Note: If you have a stoma, you can join a stoma association for support and free supplies. For more information about stoma associations, visit the Australian Council of Stoma Associations.
Recommended Reading: Bladder Cancer Recurrence After 5 Years
Stage Of Cancer Carcinoma In Situ And Additional Terms
A common question is, What stage of cancer is carcinoma in situ? Carcinoma in situ is referred to as stage 0 cancer. At this stage, cancer is considered non-invasive. Stage 1 cancers and beyond are considered invasive, meaning that even if low, there is a potential they could spread. Other terms that may be used in defining the same thing as carcinoma in situ or stage 0 cancer include:
- Non-infiltrating
- Intra-epithelial
Risk Factors For Bladder Cancer
There are some things that can make you more likely to develop bladder cancer. These are called risk factors and they include:
- smoking chemicals in cigarettes can cause bladder cancer, so if you smoke, your risk is up to 3 times that of a non-smoker
- age most people with bladder cancer are over 60 years of age
- being male men are around 3 times more likely than women to develop bladder cancer
- chemicals being in contact with certain chemicals for a long period of time, like aromatic amines, benzene products and aniline dyes, which have been linked to bladder cancer
- chronic infections frequent infections of the bladder over a long period of time
- previous cancer treatments some types of radiation therapy around the pelvis, and the chemotherapy drug cyclophosphamide
- family history a first degree relative with bladder cancer increases risk up to nearly 2 times higher than the general population.
Having these risk factors doesnt mean you will develop bladder cancer. Often there is no clear reason for getting bladder cancer. If you are worried about your risk factors, ask your doctor for advice.
Recommended Reading: Treatment For Prolapsed Uterus And Bladder
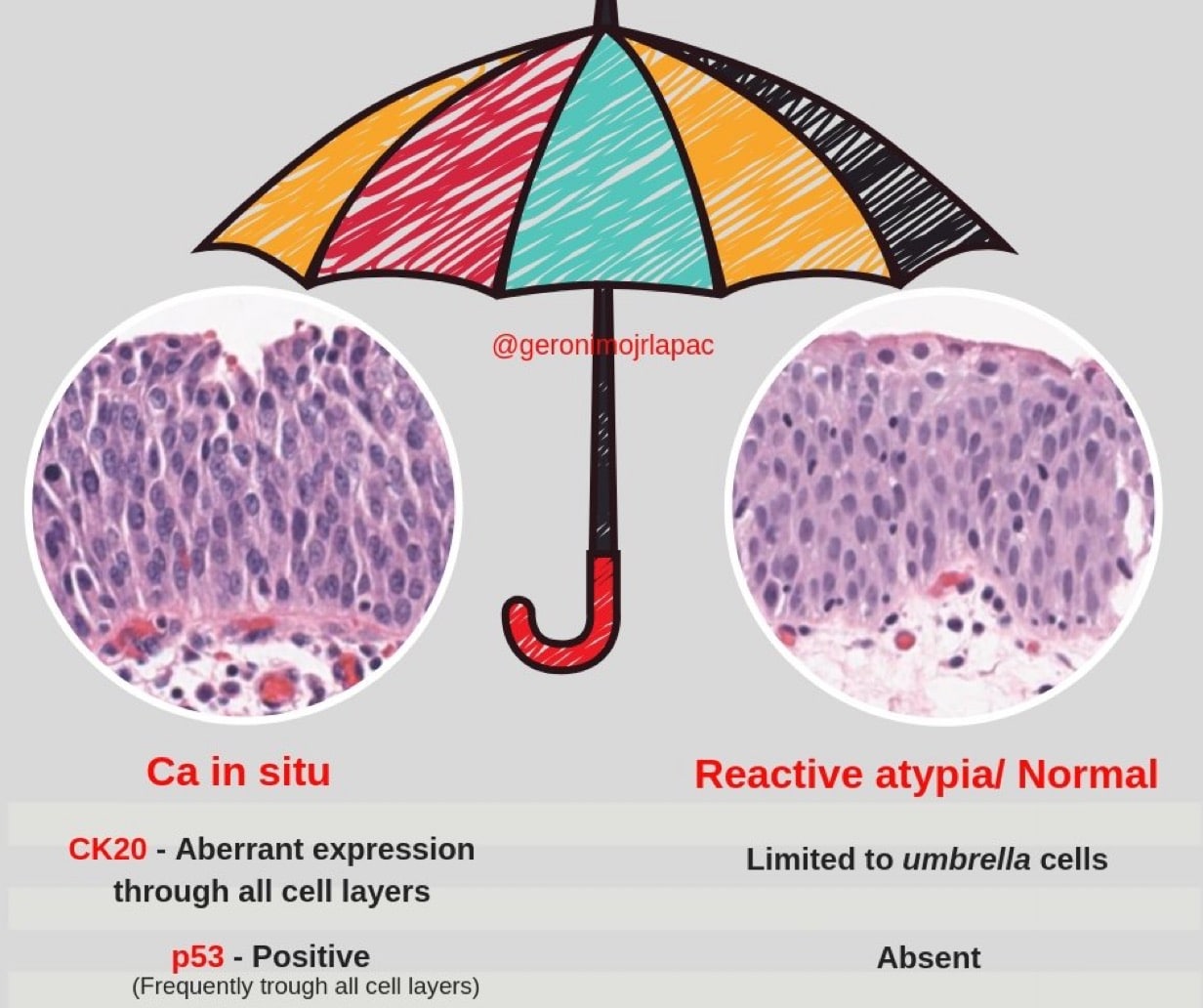
Carcinoma In Situ Of The Urinary Bladder
Carcinoma in situ is a general term that refers to a cancer that is still confined to the cells in which it initially started and has not spread into any nearby tissue. In some tissues, breast for example, it is not considered a cause for much concern. THIS IS NOT THE CASE FOR BLADDER CANCER. Bladder carcinoma in situ is always high grade and requires immediate treatment.
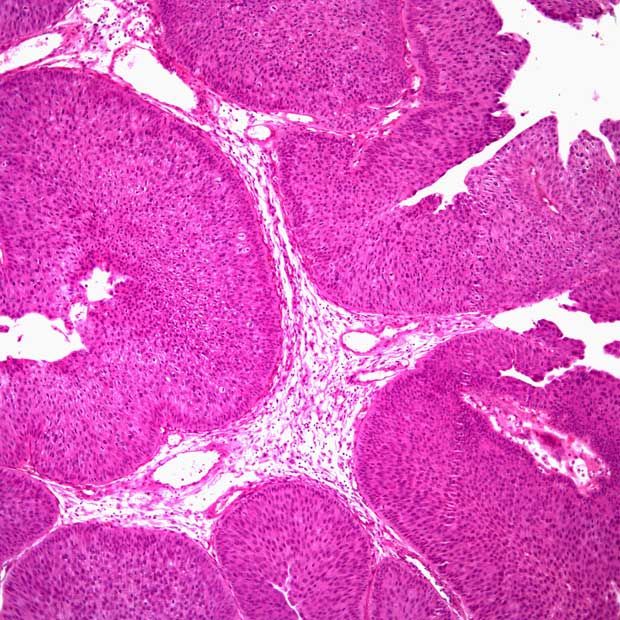
Bladder CIS presents itself as a flat, rash- or moss-like growth on the bladder lining. In some cases it may not be visible upon examination and only shows up when biopsy samples are examined by a pathologist. Bladder CIS is high grade, which means that the cells are very abnormal and are rapidly dividing. CIS has the potential to spread much more quickly than low grade tumors. CIS is often discovered along with papillary tumors or it may be present alone.
The standard of treatment for non-invasive Bladder CIS is immunotherapy. This involves local application of an immune-stimulating agent directly in the bladder. Statistically it has been found that CIS has a high rate of response to this type of treatment. Immunotherapy, along with frequent examinations by a urologist can be very effective.
B History Part : Epidemiology
Bladder carcinoma is the 4th most common cancer in males and 7th most common cancer in females. It is approximately twice as common in white men as opposed to African-American men and one and one-half times as common in white women as opposed to African-American women. The overall incidence of bladder carcinoma increases directly with age and median age at diagnosis is 70 years.
The largest risk factors in the development of bladder carcinoma are carcinogen environmental exposures. The single greatest risk factor is tobacco exposure, which confers an approximate 2-4 increase in the risk of developing bladder cancer. Latency from exposure is estimated at 20 years and smoking cessation does reduce risk profile. It is important to ask about occupational exposure as certain populations are at risk . Both cyclophospamide and ifosfamide are risk factors with or without the known side effect of hemorraghic cystitis. Pelvic irradiation confers an increased risk as well. Indwelling catheters and bladder calculi increase risk for squamous cell carcinoma.
Don’t Miss: Does Zantac Cause Bladder Cancer
There Are Three Ways That Cancer Spreads In The Body
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
You May Like: Bladder Cancer Prognosis In Elderly
Treating Stage I Bladder Cancer
Stage I bladder cancers have grown into the connective tissue layer of the bladder wall , but have not reached the muscle layer.
Transurethral resection with fulguration is usually the first treatment for these cancers. But its done to help determine the extent of the cancer rather than to try to cure it. If no other treatment is given, many people will later get a new bladder cancer, which often will be more advanced. This is more likely to happen if the first cancer is high-grade .
Even if the cancer is found to be low grade , a second TURBT is often recommended several weeks later. If the doctor then feels that all of the cancer has been removed, intravesical BCG or intravesical chemo is usually given. If all of the cancer wasnt removed, options are intravesical BCG or cystectomy .
If the cancer is high grade, if many tumors are present, or if the tumor is very large when its first found, radical cystectomy may be recommended.
For people who arent healthy enough for a cystectomy, radiation therapy might be an option, but the chances for cure are not as good.
Risk Groups For Early Bladder Cancer
Doctors put early bladder cancer into 3 risk groups. These groups describe how likely it is that your cancer will spread further, or come back after treatment.
The 3 risk groups are:
- intermediate risk
Your doctor tells you whether your cancer is low risk, intermediate risk or high risk. Knowing your risk group helps them decide which tests and treatment are best for you.
Your risk group depends on:
- the size of your tumour
- what the cells look like under a microscope
- how many tumours there are
- the type of bladder tumour
- whether you have had treatment in the last year for early bladder cancer
Read Also: Radiotherapy Success Rate For Bladder Cancer
Other Ways Of Describing Bladder Cancer
In addition to its cell type, bladder cancer may be described as noninvasive, non-muscle-invasive, or muscle-invasive.
-
Noninvasive. Noninvasive bladder cancer includes noninvasive papillary carcinoma and carcinoma in situ . Noninvasive papillary carcinoma is a growth found on a small section of tissue that is easily removed. This is called stage Ta. CIS is cancer that is found only on or near the surface of the bladder, which is called stage Tis. See Stages and Grades for more information.
-
Non-muscle-invasive. Non-muscle-invasive bladder cancer typically has only grown into the lamina propria and not into muscle, also called stage I. Non-muscle-invasive cancer may also be called superficial cancer, although this term is being used less often because it may incorrectly suggest that the cancer is not serious.
-
Muscle-invasive. Muscle-invasive bladder cancer has grown into the muscle of the bladder wall and sometimes into the fatty layers or surrounding tissues or organs outside the bladder.
It is important to note that non-muscle-invasive bladder cancer has the potential of spreading into the bladder muscle or to other parts of the body. Additionally, all cell types of bladder cancer can spread beyond the bladder to other areas of the body through a process known as metastasis.
Prognosis And Survival For Bladder Cancer
If you have bladder cancer, you may have questions about your prognosis. A prognosis is the doctors best estimate of how cancer will affect someone and how it will respond to treatment. Prognosis and survival depend on many factors. Only a doctor familiar with your medical history, the type and stage and other features of the cancer, the treatments chosen and the response to treatment can put all of this information together with survival statistics to arrive at a prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person that the doctor will consider when making a prognosis. A predictive factor influences how a cancer will respond to a certain treatment. Prognostic and predictive factors are often discussed together. They both play a part in deciding on a treatment plan and a prognosis.
The following are prognostic and predictive factors for bladder cancer.
You May Like: Bladder Infection In Toddler Girl Symptoms
Early Bladder Cancer Staging
Early bladder cancer means the cancer cells are only in the inner lining of the bladder. They have not grown through the inner lining and into the deeper muscle layer of the bladder. It is early in its development.
Early bladder cancer is also called superficial bladder cancer, or non muscle invasive bladder cancer.
Cancer Stages For Superficial Bladder Cancer
Ta: The most common superficial bladder cancer is stage Ta. This tumor looks like a cauliflower in the bladder, and it does not grow into any of the layers of the bladder. Further treatments for single Ta tumors are usually not needed. Patients do need to come back for regular cystoscopy to make sure the tumor does not come back. In patients with tumors that come back, or patients with many of these tumors at the initial surgery, medicine can be given inside the bladder to prevent cancer from coming back. Stage Ta cancers do come back with some regularity, but they rarely change into cancers that can grow into the bladder wall or go to other parts of the body.
You May Like: Best Natural Remedy For Bladder Infection
C History Part : Competing Diagnoses That Can Mimic Bladder Carcinoma
As the most common presenting symptom of bladder carcinoma is painless hematuria, any disease process that causes hematuria can mimic the disease. Most common amongst these are urinary tract infections and kidney stones, or primary neoplasm elsewhere in the genito-urinary tract. A history of trauma and any recent instrumentation should be elicited. In females, endometriosis should be considered. Rheumatologic causes such as Goodpasture syndrome, immunoglobulin A nephropathy and glomerular diseases are possible.
Erbb2 Expression As Potential Risk
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Unlimited fulltext viewing Of this article
- Organize, annotate And mark up articles
- Printing And downloading restrictions apply
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Don’t Miss: Bladder Cancer That Has Metastasized