Will I Be On A Special Diet After Surgery
Specific diet recommendations will be given at the time of discharge. Most patients will be able to eat a regular diet at the time of discharge. However, it is common for the intestines to slow down after this type of surgery, so we recommend eating smaller, more frequent meals, and drinking plenty of liquids until your initialfollow-up appointment.
Patient Selection And Assessment Of Data
From October 2010 through March 2014, 185 consecutive patients underwent open RC at Sapporo Medical University Hospital and 9 affiliate institutions participating in the Sapporo Medical University Urologic Oncology Consortium project. Patients who had received prior external beam radiotherapy were excluded from this study. Preoperative characteristics of the patients such as age, sex, BMI, ECOG-PS, the ASA score, Charlson Comorbidity Index , smoking history, presence of hydronephrosis, serum creatinine and neoadjuvant chemotherapy were recorded prior to RC. BMI was calculated preoperatively according to the WHO guidelines, and divided into the following subgroups. The clinical stage and surgical parameters such as the operating time, intraoperative blood loss and transfusion requirement were recorded immediately after surgery. Pathological examination was performed by experienced pathologists at each institution according to the 2009 TNM classification. The postoperative complications were updated appropriately in a timely manner during the hospital stay. After discharge, the patients were told to come to the hospital where they had undergone surgery if they felt any change of their health status. Thus, complete information about complications was collected within a period of 90 days after surgery. This study was approved by the institutional review board of Sapporo Medical University .
Open Versus Robot Assisted Rc
Despite advances in technology and patient care, open RC still has high rates of perioperative complication and mortality even in the most experienced hands at high volume centers . For many abdominal surgeries, the minimally invasive approach is deemed superior with respect to postoperative recovery and peri-operative morbidity without influencing cancer-free rates. With the advent of robotic assisted surgery, there is the potential to improve surgeon precision and dexterity while reducing surgeon fatigue. With this in mind, there have been numerous studies looking to see if robot-assisted RC can improve outcomes of this highly morbid surgery. In 2015, Bochner and colleagues reported on a randomized controlled trial comparing ORC and RARC. The trial was closed prematurely at the time of a planned interim analysis when it was apparent that an improvement in the 90-day rate of grade 25 complications with RARC would not be met with further patient enrollment . The trial showed decreased blood loss and increased length of surgery, but the length of stay and pathology outcomes were similar and RARC was significantly less cost effective .
In the RAZOR trial, Parekh and colleagues randomly assigned 302 patients across 15 US institutions to undergo ORC or RARC between 2011 and 2014 . They demonstrated non-inferiority of RARC in comparison to ORC with respect to 2-year progression-free survival .
Also Check: Malignant Neoplasm Of Bladder Unspecified Icd 10
Changing A Urostomy Appliance On My Own
The first day, she changed everything with instructive dialogue as I watched. The next day when she came, I wanted to see if I could do it on my own. She talked me through everything, and as I was taking the washcloth off of my stoma, it sprouted urine out as if I was walking past a barrel of clams at a fresh seaside market or something! I screamed and slammed the washcloth into my belly to cover my stoma. We laughed and I apologized for screaming. I just had not expected that!
Four years later, I can predict it all a bit better. My stoma is still unpredictable. I have to really pay attention when I’m changing my appliance so that I don’t end up spraying everything with urine.
How Is Life After A Cystectomy
After a few weeks, you should be able to return to work or school and resume light physical activities.
After you recover from a cystectomy, it may take time to adjust to the changes to your body. If you have an ostomy bag, the following tips may help you adjust faster:
- Empty the bag before its half-full to keep it flat.
- Use warm water, a washcloth and mild, fragrance-free soap to clean and rinse the skin around your stoma.
- After you wake up, change your pouch before you drink anything to help prevent dripping.
- After you empty your bag, add a pouch of ostomy deodorant to help control odors.
- Use ostomy powder when you change your bag to reduce skin irritation.
Some people find it helpful to be upfront with others about their ostomy bag. Ultimately, its up to you to decide how open you want to be about your surgery and ostomy. Your healthcare provider can recommend how and when to explain your surgery and ostomy bag to others.
Read Also: Can You Strengthen Bladder Muscles
Radical Cystectomy: Risk Versus Reward For Patients With Bladder Cancer
Although muscle-invasive disease is often treated by removal of the bladder, experts reveal potential high risk of death.
Standard treatment for patients with muscle-invasive bladder cancer is radical cystectomy, which involves surgery to remove all the bladder and nearby tissues and organs. But researchers from Mount Sinai in New York explained that the standard procedure is associated with life-altering implications because of the need to create a new way to pass urine out of the body after the organ has been removed and, potentially, considerable risk of death.
Radical cystectomy is a curative backbone of treatment for muscle-invasive bladder cancer, Matthew Galsky, M.D., professor of medicine, hematology and medical oncology at Mount Sinai, said in an interview with CURE. However, the median age of onset bladder cancer in the United States is the mid- to late-70s. Cystectomy is a major operation and not without risks.
In a study published in JNCI Cancer Spectrum, they examined the risk of early death post-cystectomy in nearly 8,000 patients with muscle-invasive bladder cancer who underwent radical cystectomy without perioperative chemotherapy within the National Cancer Database from 2003-2012.
We were a bit surprised by the proportion of patients in this large who would be considered at high risk for cystectomy-related mortality, Galsky said.
Related Content:
What Were Some Of The Notable Findings Were Any Of Those Surprising To You And Your Coauthors
To look at this, we used the Mayo Clinic Cystectomy Registry. We identified a little over 3700 patients that had cystectomy between 1980 and 2020. Our primary outcome was a patient experiencing a VTE within 90 days of their surgery. After multivariable adjustment, we did find a significant association between blood transfusion and developing a VTE.
I think what was surprising to us is that when we specifically looked at timing, there did appear to be a unique time that was at a higher risk than others. We looked at transfusion as a 3-tiered variable. The first group had no transfusions. Group number 2 had an intraoperative transfusionso got a blood transfusion during surgery, and that included patients regardless of whether they needed one after surgery, so both with and without. The third group had only a postoperative transfusionso not in the operating room, but only afterwards. When we looked at it this way, we found only the patients that had an intraoperative transfusion had a higher risk of VTE, not those that got it afterwards.
We then looked at it as a continuous variable. Each unit of blood that you got during surgery was associated with about 7% higher odds of a VTE within 90 days. That finding was robust to a number of sensitivity analyses. We looked at number of lymph nodes removed, operative time, we used an interaction term for year of surgery, along with blood transfusion. Despite all those adjustments, we still found the same significant result.
Recommended Reading: Will Losing Weight Help Bladder Leakage
What Kind Of Support And Help Can I Expect
You will not go through this surgery alone.While in the hospital you will be given instructions on the care of your catheters and stents. A nurse specializing in stomas will see you several times if you have a stoma. For many of our patients, visiting nurses will come to your home daily to help you care for your drains and check on you after you are discharged from the hospital.
A radical cystectomy and urinary diversion can present a difficult emotional adjustment. Support is available to help patients deal with this impact on their lives. A social worker is part of the team to care for patients while in the hospital. Patients or their families can request a social worker to help provide emotional support during this difficult time. After discharge, the social worker can provide names and numbers of support groups. You can call 825-7171 to talk to the social workers.
Clinicians Should Limit Intraoperative Blood Transfusion During Radical Cystectomy Expert Says
Each unit of blood that you got during surgery was associated with about 7% higher odds of a VTE within 90 days, says Timothy D. Lyon, MD, FACS.
In the following interview, Timothy D. Lyon, MD, FACS, discusses his recent Journal of Urology study1 that found an increased risk of venous thromboembolism following radical cystectomy when blood transfusion occurred intraoperatively. Lyon is a urologic oncologist at Mayo Clinic in Jacksonville, Florida.
Recommended Reading: Bladder Pacemaker For Urinary Retention
What Happens During A Cystectomy
A special team of healthcare providers will perform a cystectomy. The team typically includes:
- An anesthesiologist.
The anesthesiologist will sedate you with general anesthesia. You wont be awake, wont move and wont feel any pain during the procedure.
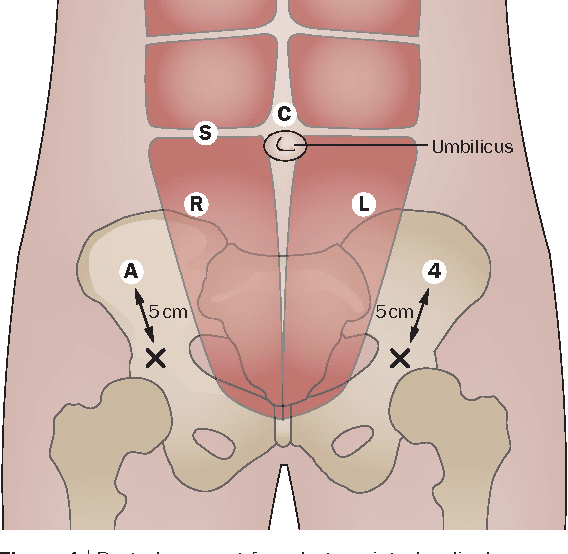
Your urologist will perform your cystectomy using one of two different surgical approaches:
- Open cystectomy. Your urologist accesses your bladder and the tissues around it with one, long vertical surgical incision of about six to seven inches between your belly button and pubic bone. Theyll then insert their gloved hands into your body cavity through the incision to perform the operation.
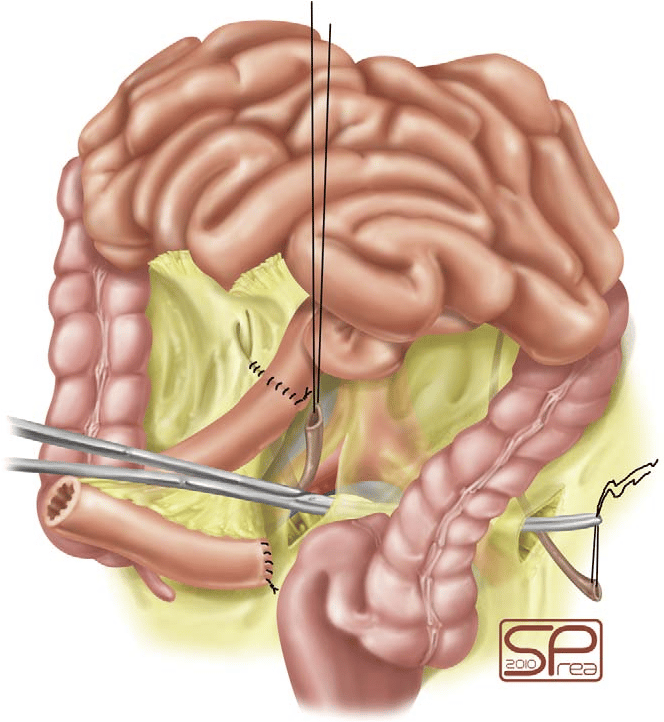
- Minimally invasive cystectomy. Your urologist will first inflate your abdomen with carbon dioxide to create a working space. Theyll then make five to six very small incisions in your abdomen so that they can insert long, thin instruments, including a camera, into your body cavity. Laparoscopic surgery means your urologist uses these instruments to perform the surgery with these tools. Robotic surgery involves attaching the instruments to a surgical robot that your urologist controls through a surgical console . A surgical robot enhances the operation by providing three-dimensional vision as well as more precise movements.
How long does cystectomy surgery take?
A cystectomy takes approximately six hours to perform.
What About Exercise/activity
- You can do gentle exercise such as walking less than 1.5km
- Avoid strenuous activity, heavy lifting or engage in sports for 6 weeks to prevent wound complications such as hernias
- Avoid driving a car until you have no pain and not on any pain killers. This can vary from patient to patient but can take a number of weeks. Beware of fatigue as this may affect concentration and is very common after any operation. If in doubt it is safer to wait longer until commencing driving
- Returning to work depends on the physical demands of your duties. Although you may be able to return to work after a few weeks if there are low physical demands, be aware that fatigue is common after any major operation and can persist for up to 6 months. In most cases, up to 3 months may be required off work after this major open cancer operation. medical certificates can be supplied as required.
- Avoid overseas travel for 6 weeks as a minimum . Any non-essential travel should probably be put off for at least 3 months.
Read Also: What Is Bladder Sling Surgery
Changes To Your Bowels
Having a recto sigmoid pouch can cause bowel changes. This is because part of your bowel has been removed and is now shorter. You may notice that:
- your poo is looser than normal
- you go to the toilet more frequently
- you get constipated and need medicine to help you go
It can take some time to return to normal, often a few months or longer.
Effects Of Cystectomy On Urination
Bladder surgery can affect how you pass urine. If you have had a partial cystectomy, this might be limited to having to go more often .
If you have a radical cystectomy, you’ll need reconstructive surgery to create a new way for urine to leave your body. Depending on the type of reconstruction, you might need to learn how to empty your urostomy bag or put a catheter into your stoma. Aside from these changes, urinary diversion and urostomy can also lead to:
- Blockage of urine flow
- Absorption problems
The physical changes that come from removing the bladder and having a urostomy can affect your quality of life, too. Discuss your feelings and concerns with your health care team.
To learn a lot more about urostomies, see Urostomy Guide.
Also Check: Can Tamoxifen Cause Bladder Cancer
Can I Shower Bathe And Swim With A Urostomy
A stoma is a one-way door, so waterâs not a problem. You can shower and bathe with or without your pouch. But itâs best not to use bath oils or soaps with moisturizer.
Swimming isnât a problem, either. It helps to:
- Wear a smaller bag or a waterproof cover when you swim.
- Wear your pouch, but empty it before you get into the water.
- Use waterproof tape around the edges of the pouch.
- Wait a few hours after you put on a new pouch before you swim.
The Severity Of The Pain Post
When you wake up from surgery, you will feel like you were cut from chin to crotch. When I woke up from my surgery, the pain is unreal despite being given pain meds. My surgery was planned for 8 hours and ended up taking 9 hours. I’m not even sure exactly how long I was “out” as it all blended together for the first few days. In actuality, my scar is only about 4-5 inches, but I could have sworn in those first few weeks that it was much, much larger! Obviously, with time, it gets better, but it is definitely a level of pain that I was not prepared for.
Don’t Miss: How Do They Inject Botox Into The Bladder
Sexual Effects Of Urostomy
Its normal people to be concerned about having a sex life with a urostomy. Having your ostomy pouch fit correctly and emptying it before sex reduces the chances of a major leak. A pouch cover or small ostomy pouch can be worn with a sash to keep the pouch out of the way. Wearing a snug fitting shirt may be more comfortable. Choose sexual positions that keep your partners weight from rubbing against the pouch. For more tips, see Urostomy Guide.
What Happens Before The Operation
You will be admitted to the hospital the day of your operation. The anesthesiology team will talk to you about their portion of the surgery. If you are a candidate, you may receive an epidural, which is a good option to manage post-surgery pain. The usual hospital stay is 6 to 8 days. On the day of surgery, your family can wait for you in the surgical waiting area on the first floor of the Ronald Reagan Hospital . It usually takes 4 to 8 hours to complete this operation. On completion of the operation the surgeon will contact your family there.
A portion of your intestines will be used to create the urinary diversion. It is important that the entire intestine be clean before surgery, and that you prepare your gastrointestinal tract prior to admission to the hospital. Your surgeon will provide you specific instructions for the bowel preparation.
Also Check: Bladder Cut During C Section Malpractice
Will My Physical Activity Be Restricted After Surgery
It is critical to remain active even while you are recovering from surgery. Walking every day is important and will speed up the healing process, decrease depression, and increase muscle tone. It takes approximately 6 weeks for the surgical area to heal completely. Please do not do any heavy lifting, strenuous exercises, or excessive stair climbing during this time. You may drive a car 3 to 4 weeks after surgery if you feel well and are not taking any more prescription pain medications.
What Is A Neobladder
A neobladder is type of internal reservoir for storing urine. Using a portion of small intestine, the urologist reconstructs the tubular shape of the intestine and creates a sphere. The surgeon then connects the pouch to the urethra, creating a neobladder, in which case the patient can void normally. By tensing the abdominal muscles and relaxing certain pelvic muscles, the patient is able to push the urine through the urethra.
Recommended Reading: Can The Bladder Heal Itself
Device Issues And Urinating In A New Way
Tami Walker is a WOC nurse at the University of Michigan, and she sees her job as not only treating patients physical wounds, but also rebuilding their self-esteem. The surgeon goes through a lot of the clinical part of it, Walker says, but not how to live every day. Although Walker counsels some neobladder patients pre-operatively, she spends most of her time helping patients with their urostomies: Walker introduces them to different pouching systems shows them how they attach to the stoma, empty out, and need to be replaced and provides direct care for complications.
General leakage from not having the proper fit is the biggest problem, she says. The adhesive on urostomy pouches doesnt always stick well to a patients abdomen, especially as their body contour shifts in the first eight weeks after surgery.
Months after her operation, Florida resident Nikki Saltzburg, 44, is still trying to figure out how her stoma works. Every time she changes her urostomy bag, she carries a toolbox of materials into the bathroom: an anti-adhesive aerosol to remove the old pouch, a stencil and pair of scissors to cut a hole in the new pouch, a sticky paste to attach the pouch to her stoma, and a handheld fan to dry her skin. It still takes me a while, and the challenge is the stoma doesnt stop leaking urine, Saltzburg says, so urine can be running down your stomach or spraying somewhere.
Read More:Changing Cancer Care, So Patients No Longer Feel Like a Number