For Patients With A Urostomy
If you had a radical cystectomy and now have a urostomy, you might worry even about everyday activities at first. You might have to alter some of your daily routines because of changes in how you urinate. Other issues such as having sex might also cause concerns .
Its normal to have worries and concerns when adjusting to such a major change. But its important to know there are health care professionals who are specially trained to help people with their urostomies. They can teach you to take care of your urostomy and help you cope with the changes it brings. You can also ask the American Cancer Society about programs offering information and support in your area. For more information, see our Urostomy Guide.
Data Collection And Patient Follow
Data Collection
All patients received routine hematological examination, computed tomography, transabdominal ultrasound, urine cytology or tissue biopsy, cystoscopy prior to surgery in order to diagnose NMIBC, and finally confirmed by postoperative pathology. Pre-operative baseline clinical pathology and laboratory data such as age, gender, body mass index , smoking history, tumor size, pathological T stage, and grade were obtained through electronic medical records in the hospital and reviewed. All histopathology reports were based on the eighth edition of Tumor-Node-Metastasis staging system, and the grade was assessed based on the 2004 WHO grading system.18,19 Tumor size was the sum of the longest diameters of all postoperative pathological specimens. According to the blood test results , the preoperative serum albumin concentration, total cholesterol concentration and total peripheral lymphocyte count of all individuals were used to calculate the CONUT score. Based on the previous study,12 the scoring criteria of CONUT are illustrated in Table 1.
|
Table 1 The Scoring System for the Controlling Nutritional Status Scale |
Follow-Up
Cost Issues And Follow
Finally there is a cost issue with bladder cancer and follow-up. Leal et al. looked at the economic costs of bladder cancer across the European Union . These were 4.9 billion in 2012, of which health care costs were 2.9 billion , productivity loss 1.1 billion and informal care costs 0.9 billion . Bladder cancer costs represented 5% of total health care cancer costs and 3% of all cancer costs in the EU in 2012. Of note, difference between the least and most expensive country was> tenfold. For follow-up costs, all three fields play a role. Interestingly, Mossanen et al. used a Markow model to specifically evaluate costs of surveillance of NMIBC Their index patient was a compliant 65-year-old male, and they used four health states: no evidence of disease, recurrence, progression/cystectomy and death. The cumulative costs over a 5-year period were USD 52,125, 146,250 and 366,143 for low-, intermediate- and high-risk, respectively. Costs for recurrence were highest in the low-risk group, but still not more than 8% of the total costs of low risk. Progression and subsequent treatment results in much higher costs , even when not frequent in low-risk patients.
In all, there is certainly an opportunity to reduce patient burden and costs in an adapted follow-up strategy with a marker with a high NPV, where the financial benefit obviously depends on the price of the marker. Prospective studies will be necessary to validate these assumptions on national levels.
You May Like: Can Bladder Infection Cause Urine Leakage
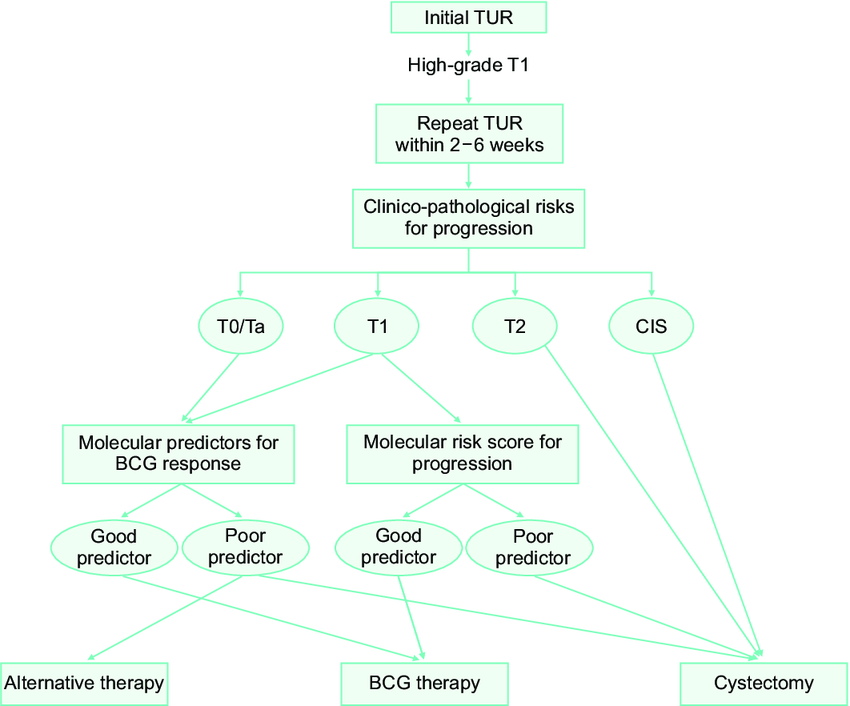
Treatment For Hg T1 Bladder Cancer With Pt1 Histology At Second Tur
In theory, T1 tumors can be completely removed by TUR. However, residual T1 tumors in second TUR specimens are associated with future muscle-invasive disease. Herr et al. evaluated the relationships between the second TUR pathology and future progression of 352 patients with T1 bladder cancer on initial TURBT. Of the 92 patients with residual T1 disease at the second TUR, 82% progressed to muscle invasion within 5 years. In contrast, of the 260 patients without lamina propria invasion at the second TUR, only 19% progressed at 5 years. A multi-institutional study including 1136 patients with T1 bladder cancer who underwent radical cystectomy demonstrated that 50% of these cancers were upstaged to muscle-invasive disease after cystectomy . Another collaborative study including 167 patients who underwent radical cystectomy for T1 G3 bladder cancer revealed that 50% of the patients were pathologically upstaged on cystectomy specimens and 28% had extravesical disease. Other contemporary series showed upstaging in the cystectomy specimen in 2051% . Ark et al. demonstrated that the survival rate for patients who were appropriately staged was significantly higher than for those who were understaged at the final pathology from radical cystectomy.
Treating Stage Iii Bladder Cancer
These cancers have reached the outside of the bladder and might have grown into nearby tissues or organs and/or lymph nodes . They have not spread to distant parts of the body.
Transurethral resection is often done first to find out how far the cancer has grown into the bladder wall. Chemotherapy followed by radical cystectomy is then the standard treatment.Partial cystectomy is rarely an option for stage III cancers.
Chemotherapy before surgery can shrink the tumor, which may make surgery easier. Chemo can also kill any cancer cells that could already have spread to other areas of the body and help people live longer. It can be especially useful for T4 tumors, which have spread outside the bladder. When chemo is given first, surgery to remove the bladder is delayed. The delay is not a problem if the chemo shrinks the cancer, but it can be harmful if it continues to grow during chemo. Sometimes the chemo shrinks the tumor enough that intravesical therapy or chemo with radiation is possible instead of surgery.
Some patients get chemo after surgery to kill any cancer cells left after surgery that are too small to see. Chemo given after cystectomy may help patients stay cancer-free longer, but so far its not clear if it helps them live longer. If cancer is found in nearby lymph nodes, radiation may be needed after surgery. Another option is chemo, but only if it wasn’t given before surgery.
Also Check: Quick Fix For Bladder Infection
Disclosure Of Potential Conflicts Of Interest
J. Bellmunt reports grants from FIS PI16/00112 , grants from Friends of Dana-Farber , other funding from Retired Professional Fire Fighters Cancer Fund , and other funding from Whole Foods Golf Classic for bladder cancer research during the conduct of the study. A. Rodriguez-Vida reports grants from Takeda, grants and personal fees from MSD, personal fees from Clovis, personal fees from Sanofi, personal fees from BMS, personal fees from Roche, personal fees from Janssen, personal fees from Astellas, and personal fees from Bayer outside the submitted work. K.W. Mouw reports other funding from Pfizer outside the submitted work. E.M. Van Allen reports personal fees from Tango Therapeutics, other compensation from Syapse , personal fees and other from Enara Bio , personal fees and other compensation from Manifold Bio , personal fees and other compensation from Monte Rosa , personal fees from Invitae, personal fees from Genome Medical , grants from BMS, and grants from Novartis outside the submitted work. G. Getz reports grants from IBM, grants from Pharmacyclics, and personal fees from Scorpion Therapeutics outside the submitted work in addition, G. Getz has a patent for MuTect issued, a patent for MutSig issued, a patent for POLYSOLVER issued and with royalties paid from Neon Therapeutics, a patent for ABSOLUTE pending, and a patent for Bladder Cancer Classification pending. No potential conflicts of interest were disclosed by the other authors.
Treating Stage 0 Bladder Cancer
Stage 0 bladder cancer includes non-invasive papillary carcinoma and flat non-invasive carcinoma . In either case, the cancer is only in the inner lining layer of the bladder. It has not invaded the bladder wall.
This early stage of bladder cancer is most often treated with transurethral resection with fulguration followed by intravesical therapy within 24 hours.
Read Also: Women’s Bladder Falling Out
Another Option For Reducing Recurrences
Other studies have demonstrated that giving patients with low-grade bladder cancer the chemotherapy drug mitomycin C through a catheter following surgery can reduce the chance of a recurrence. These studies led professional groups in the United States and Europe to recommend this approach for patients with low-grade disease that has not invaded the muscle.
In the United States, however, few patients receive this treatment, in part because of concerns about the side effects of mitomycin C, as well as the availability and cost of the drug, noted Dr. Messing. Mitomycin C can be toxic if it leaks out of the bladder through a hole, and the drug can also cause severe rashes when it comes in contact with skin.
Gemcitabine, on the other hand, is a well-tolerated, readily available drug that “comes at relatively little cost in terms of side effects or expense,” said Dr. Messing. The side effects were similar between the two groups in the trial and were generally manageable, he added.
Some patients with advanced bladder cancer already receive gemcitabine, noted Piyush Agarwal, M.D., who heads the Bladder Cancer Section in NCI’s Center for Cancer Research and was not involved in the trial. “So, it makes sense that the drug would be used to treat patients with low-grade bladder cancer.”
Dr. Agarwal predicted that the new study would lead to revisions in treatment guidelines to include gemcitabine as an option for reducing recurrences in the patients with low-grade bladder cancer.
Treatment For Hg Pt1 Bladder Cancer With Pt2 Or More Histology At Second Tur
There is no doubt about the need to perform radical cystectomy for patients with muscle-invasive disease at the second TUR. Most of these tumors are understaged at the initial TURBT due to technical problems, and may not be large or bulky like muscle-invasive tumors that are diagnosed at the initial TURBT and/or with computed tomography or magnetic resonance imaging. The discussion on the treatment strategies for these tumors does not include whether cystectomy should be performed but whether neoadjuvant chemotherapy and/or extended lymph node dissection should be performed.
Several randomized Phase III trials and meta-analyses demonstrated the survival benefit of cisplatin-based neoadjuvant chemotherapy for patients with MIBC. However, whether neoadjuvant chemotherapy prolongs the survival of patients with T1 cancer at the initial TURBT and with muscle-invasive disease detected by a second TUR is unclear. Neoadjuvant chemotherapy offers potential advantages in tumor downstaging and eradication of micrometastases, so this therapy should be indicated for patients who have risk factors for locally advanced disease or nodal metastasis.
Read Also: Can Men Get Bladder Infections
How Is Bladder Cancer Treated
Treatment for bladder cancer depends on
- The stage of cancer.
- If cancer has spread beyond the lining of the bladder.
- The extent of cancer spread.
Treatment options based on tumor grade
- High-grade bladder cancer: High-grade cancers that are life-threatening and spread quickly need to be treated with chemotherapy, radiation or surgery.
- Low-grade cancers: Less aggressive cancers have a low chance of becoming high grade and do not require aggressive treatments, such as radiation or bladder removal.
Treatment options may vary depending on the tumor stage.
Comparison Of Recurrence Risk Among Patients With Different Eortc
During the five-year follow-up period, 33 of 94 patients experienced intravesical recurrence, including 3 cases in the low-risk group, 7 cases in the intermediate-risk group, and 23 cases in the high-risk group. In addition, the KaplanMeier analysis demonstrated that the EORTC-GUCG risk scoring system had a significant correlation with RFS, and the high-risk group patients had shorter RFS than the other two groups .
|
Figure 1 Survival curve of RFS in patients at risk for different EORTC-GUCG risk scores. |
You May Like: Go Less Bladder Control Side Effects
Understanding The Statistics: Cancer Survival
It is important to remember that all cancer survival numbers are based on averages across huge numbers of people. These numbers cannot predict what will happen in your individual case.
Survival rates will not tell you how long you will live after you have been diagnosed with bladder cancer. But, these numbers can give you an idea of how likely your treatment will be successful. Also, survival rates take into account your age at diagnosis but not whether you have other health conditions too.
Ask Your Doctor For A Survivorship Care Plan
Talk with your doctor about developing a survivorship care plan for you. This plan might include:
- A suggested schedule for follow-up exams and tests
- A schedule for other tests you might need in the future, such as early detection tests for other types of cancer, or tests to look for long-term health effects from your cancer or its treatment
- A list of possible late- or long-term side effects from your treatment, including what to watch for and when you should contact your doctor
- Diet and physical activity suggestions
- Reminders to keep your appointments with your primary care provider , who will monitor your general health care.
Don’t Miss: What Are The Survival Rates Of Bladder Cancer
Other Options During Follow
Since 2019, the EAU guideline has a recommendation on outpatient fulguration or laser vaporization of small papillary recurrences in follow-up of patients known with previous low-grade Ta tumors . Although the recommendation is weak, this is often common practice in daily routine. Outpatient fulguration obviously does not prevent a cystoscopy, but it does reduce subsequent therapeutic burden.
Bladder Cancer And Treatment Options For Recurrence
If your bladder cancer recurs, you will undergo tests to find out more about the cancer cells.1-3 The type of treatment will depend on where the cancer cells have recurred and what type of treatments you received before. After learning more about the recurrence, your cancer care team will discuss all the possible treatment options that are available for you.
Some treatment options that can be used for bladder cancer recurrence, either alone or in combination, include:
- Surgery
Also Check: How Is Immunotherapy Administered For Bladder Cancer
How Long Will You Live If You Have Bladder Cancer
The survival rate depends on the stage of cancer at diagnosis and other health issues.
Overall, 70 to 90 percent of people with localized bladder cancer will live for at least five years or more. The physician calculates this with the help of survival rates. Survival rates indicate the percentage of people who live with a certain type of cancer for a specific time. The physician often uses an overall five-year survival rate. Factors that may affect survival rate include
Table. Five-year survival rates of different stages of bladder cancer
| Bladder cancer SEER stages | Five-year relative survival rate |
|---|---|
| In situ alone | 96 |
| All SEER stages combined | 77 |
The surveillance, epidemiology, and end results stages are taken from the SEER database, maintained by the National Cancer Institute. SEER database groups cancers into localized, regional, and distant stages.
- Localized: There is no indication that cancer has spread outside the bladder.
- Regional: Cancer has invaded the nearby structures or lymph nodes.
- Distant: Cancer has spread to distant parts of the body, such as the lungs, liver, or bones.
Thus, bladder cancer, if detected in the early stage is treatable and has higher survival rates. However, if the cancer is detected in the advanced stages, treatment becomes difficult and the survival rate is low.
Developing A Treatment Plan
In cancer care, different types of doctors often work together to create a patients overall treatment plan that combines different types of treatments.This is called a multidisciplinary team. This team is usually led by a urologist, a doctor who specializes in the genitourinary tract, or a urologic oncologist, a doctor who specializes in treating cancers of the genitourinary tract. Cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, and others.
Treatment options and recommendations depend on several factors, including:
-
The type, stage, and grade of bladder cancer
-
Possible side effects
-
The patients preferences and overall health
Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
The first treatment a person is given for advanced urothelial cancer is called first-line therapy. If that treatment stops working, then a person receives second-line therapy. In some situations, third-line therapy may also be available.
Adjuvant systemic therapy is treatment that is given after radical surgery has been completed. In bladder cancer, adjuvant therapy is usually cisplatin-based chemotherapy or treatment in a clinical trial. Neoadjuvant therapy is treatment that is given before surgery, such as cisplatin-based chemotherapy.
Don’t Miss: Does Prostate Cancer Spread To Bladder
Is Repeat Transurethral Resection Always Needed In High
- 1Urology and Renal Transplantation Unit, Department of Medical and Surgical Sciences, University of Foggia, Foggia, Italy
- 2Department of Epidemiology, University of Foggia, Foggia, Italy
- 3Section of Pathology, Department of Clinical and Experimental Medicine, University Hospital of Foggia, Foggia, Italy
- 4Urology Department, Hospital de Braga ICVS, University of Minho, Braga, Portugal
- 5Division of Urology, Department of Surgery, VCU Health, Richmond, VA, United States
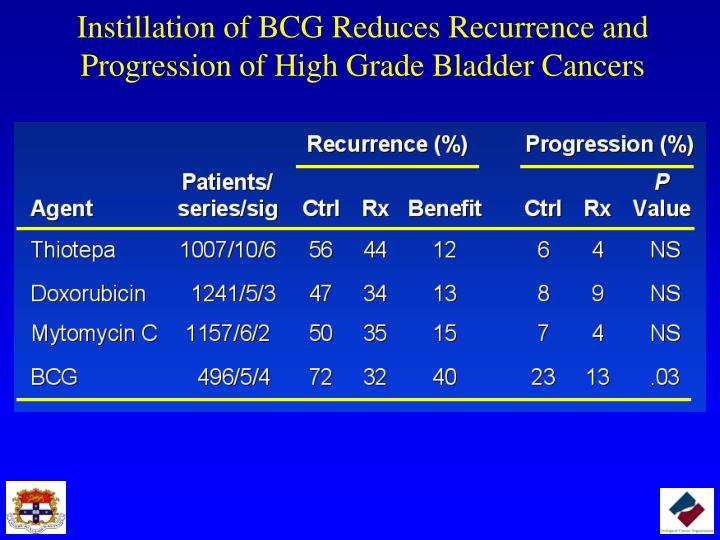
Treating Stage I Bladder Cancer
Stage I bladder cancers have grown into the connective tissue layer of the bladder wall , but have not reached the muscle layer.
Transurethral resection with fulguration is usually the first treatment for these cancers. But it’s done to help determine the extent of the cancer rather than to try to cure it. If no other treatment is given, many people will later get a new bladder cancer, which often will be more advanced. This is more likely to happen if the first cancer is high-grade .
Even if the cancer is found to be low grade , a second TURBT is often recommended several weeks later. If the doctor then feels that all of the cancer has been removed, intravesical BCG or intravesical chemo is usually given. If all of the cancer wasn’t removed, options are intravesical BCG or cystectomy .
If the cancer is high grade, if many tumors are present, or if the tumor is very large when it’s first found, radical cystectomy may be recommended.
For people who arent healthy enough for a cystectomy, radiation therapy might be an option, but the chances for cure are not as good.
Don’t Miss: Stage 4 Bladder Cancer Symptoms